系统免疫指数、中性粒细胞淋巴细胞比值对川崎病静脉注射免疫球蛋白敏感性的预测价值
2022-06-08李梦醒彭韶
李梦醒 彭韶

[摘要] 目的 探討系统性免疫指数(SII)、中性粒细胞淋巴细胞比值(NLR)、血小板淋巴细胞比值(PLR)对川崎病(KD)患儿静脉注射免疫球蛋白(IVIg)敏感性的预测价值。方法 回顾性分析2019年9月至2021年7月郑州大学第一附属医院收治的115例首诊KD患儿的完整临床资料,根据静脉注射免疫球蛋白敏感性分为IVIg敏感组和IVIg不敏感组,收集KD患儿静脉注射免疫球蛋白前发热天数、白细胞计数、中性粒细胞计数、淋巴细胞计数、血小板计数、血沉(ESR)、C-反应蛋白,并计算中性粒细胞计数×(血小板计数/淋巴细胞计数)(SII)、中性粒细胞淋巴细胞比值、血小板淋巴细胞比值。结果 与IVIg敏感组相比,IVIg不敏感组NLR、C-反应蛋白水平较高,IVIg不敏感组PLT值、淋巴细胞计数、发热天数水平较低,差异均有统计学意义(P<0.05),IVIg不敏感组PLR、SII值较IVIg敏感组低,但差异无统计学意义(P>0.05)。NLR、C-反应蛋白、PLT最佳截留点分别为5.075、80.485 mg/L、347×109/L。经多因素logistic回归分析显示,NLR、CRP水平升高,PLT水平降低,分别为KD患儿静脉注射免疫球蛋白敏感性的独立危险因素。结论 NLR对 KD患儿静脉注射免疫球蛋白敏感性的预测性能更稳定,PLR、SII对KD患儿静脉注射免疫球蛋白敏感性的预测价值需要进一步探讨。
[关键词] 川崎病;系统免疫指数;中性粒细胞淋巴细胞比值;血小板淋巴细胞比值;免疫球蛋白
[中图分类号] R725.4 [文献标识码] B [文章编号] 1673-9701(2022)11-0069-04
[Abstract] Objective To explore the predictive values of systemic immune-inflammation index (SII), neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR) in sensitivity to intravenous immunoglobulin in children with Kawasaki disease (KD). Methods The complete clinical data of 115 children with KD admitted to the First Affiliated Hospital of Zhengzhou University from September 2019 to July 2021 were retrospectively analyzed. According to the sensitivity to intravenous immunoglobulin, they were divided into the intravenous immunoglobulin sensitive group and the intravenous immunoglobulin non-sensitive group. The number of fever days, white blood cell count, neutrophil count, lymphocyte count, platelet count, erythrocyte sedimentation rate (ESR), and C-reactive protein values before intravenous immunoglobulin injection were collected in the intravenous immunoglobulin sensitive group. The SII (neutrophil count×platelet count/lymphocyte count), NLR, and PLR were calculated. Results Compared with the intravenous immunoglobulin sensitive group, the intravenous immunoglobulin insensitive group had higher levels of NLR and CRP. The PLT value, lymphocyte count, and number of fever days in the intravenous immunoglobulin insensitive group were lower than those in the intravenous immunoglobulin non-insensitive group, with statistically significant differences (P<0.05). The PLR and SII values in the intravenous immunoglobulin non-insensitive group were lower than those in the intravenous immunoglobulin sensitive group, without statistically significant differences (P>0.05). The best cut-off points for NLR, CRP, and PLT values were 5.075, 80.485 mg/L, and 347×109/L, respectively. Multivariate logistic regression analysis indicated that increased level of NLR and CRP and decreased level of PLT were independent risk factors for the sensitivity to intravenous immunoglobulin in children with KD. Conclusion NLR has a more stable predictive performance in the sensitivity to intravenous immunoglobulin in children with KD. The predictive values of PLR and SII in the sensitivity to intravenous immunoglobulin in children with KD need to be further explored.2A8C9683-8A9E-46B4-8DE6-41F3EACD5843
[Key words] Kawasaki disease; Systemic immune-inflammation index; Neutrophil-to-lymphocyte ratio; Platelet-to-lymphocyte ratio; Immunoglobulin
川崎病(Kawasaki disease,KD),又称皮肤黏膜淋巴结综合征,是以全身性中、小动脉炎症病变为主要病理特征的一种免疫系统疾病,主要发生在5岁以下儿童和婴幼儿。川崎病的心脏后遗症是造成KD患儿死亡的主要原因[1]。在疾病早期及时应用静脉注射免疫球蛋白(intravenous immunoglobulin,IVIg)治疗可将冠状动脉瘤的发生率从25%降低到4%[2]。但仍有10%~20%的KD患儿在IVIg后仍持续存在反复发热的情况,称为静脉注射免疫球蛋白不敏感[3]。大量研究表明,IVIg不敏感KD患儿发生冠状动脉损害的风险较IVIg敏感患儿明显升高[4]。所以早期识别IVIg不敏感KD,并及时调整治疗方案,对改善KD患儿预后十分重要。中性粒细胞、淋巴细胞、血小板是炎症经典指标,但单一的炎症参数很容易相互影响。因此,中性粒细胞与淋巴细胞比率(NLR)、血小板与淋巴细胞比率(PLR)、血小板计数×(中性粒细胞计数/淋巴细胞计数)(SII)的整合信息更有利评估炎症和免疫状态[5-6]。目前大量研究表明,PLR、NLR、SII在评估癌症预后与IVIg敏感度及冠状动脉损伤方面有着更良好的预测性能[7-8]。本文主要通过回顾性分析郑州大学第一附属医院儿科115例首诊KD患儿的实验室指标,研究SII、NLR、PLR对KD患儿IVIg不敏感的预测价值,从而进行早期干预,现报道如下。
1 资料与方法
1.1 一般资料
收集2019年9月至2021年7月郑州大学第一附属医院收治的115例首诊KD患儿的完整临床资料,患儿入院前未IVIg。所有研究对象均满足2004年美国心脏协会(AHA)制定的KD诊断科学报告[9]中KD的临床诊断标准。IVIg不敏感川崎病的诊断标准:首次IVIg治疗36 h后体温仍超过38℃或退热2~7 d后再出现发热并伴随至少一项川崎病主要症状特征定义为IVIg不敏感[10]。其中IVIg敏感KD患儿(IVIg敏感组)84例, IVIg不敏感KD患儿(IVIg不敏感组)31例。所有患儿均发热10 d内接受IVIg。
1.2 方法
收集未静脉注射免疫球蛋白KD患儿入院次天晨起抽血检测的白细胞计数(WBC)、中性粒细胞计数(N)、淋巴细胞计数(L)、血小板计数(PLT)、血沉 (ESR)、C-反应蛋白结果,并计算SII、NLR、PLR。同时收集KD患儿的性别、年龄、发热天数、病程8周内患儿的心脏彩超结果等一般资料。根据其IVIg敏感性分为IVIg敏感组和IVIg不敏感组,分别进行单因素分析,以P<0.05为差异有统计学意义,筛选出差异有统计学意义的指标,然后进行单因素logistic回归分析危险因素,并应用ROC曲线评价其预测价值。
1.3 统计学处理
采用SPSS 23.0统计学软件进行数据分析。计数资料以[n(%)]表示,组间比较采用χ2检驗;符合正态分布的计量资料以(x±s)表示,组间比较采用独立样本t检验;非正态分布的计量资料以[M(P25,P75)]表示,组间比较采用Mann-Whitney U检验。在对KD患儿IVIg敏感度分析中有显著差异的实验室检查指标行单因素logistic回归分析,分析IVIg敏感性的影响因素;对单因素logistic回归分析中P<0.05的指标构建ROC曲线,确定截断值、ROC曲线下面积(AUC)敏感度、特异度。P<0.05为差异有统计学意义。
2 结果
2.1 两组患儿一般资料比较
共收集115例首诊KD患儿的完整临床资料,84例对IVIg敏感,31例对IVIg不敏感, IVIg敏感组中男51例(60.7%),女33例(39.3%),中位数月龄28.5个月。IVIg不敏感组男21例(67.7%),女10例(32.3%),中位数月龄27个月。两组KD患儿的性别、月龄比较,差异无统计学意义(P>0.05),具有可比性。与IVIg敏感组KD患儿相比,IVIg不敏感组KD患儿初始静脉注射免疫球蛋白前发热天数更短,差异有统计学意义(P<0.05)。见表1。
2.2 两组患儿临床资料比较
与IVIg敏感组相比,IVIg不敏感组NLR、C-反应蛋白值均较高,IVIg不敏感组PLT、淋巴细胞计数、发热天数较IVIg敏感组低,差异均有统计学意义(P<0.05); 诊断KD前白细胞计数、中性粒细胞计数、ESR、SII、PLR组间比较,差异无统计学意义(P>0.05)。见表1。
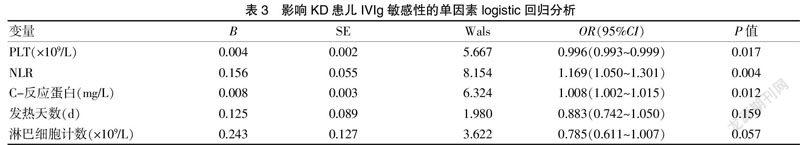
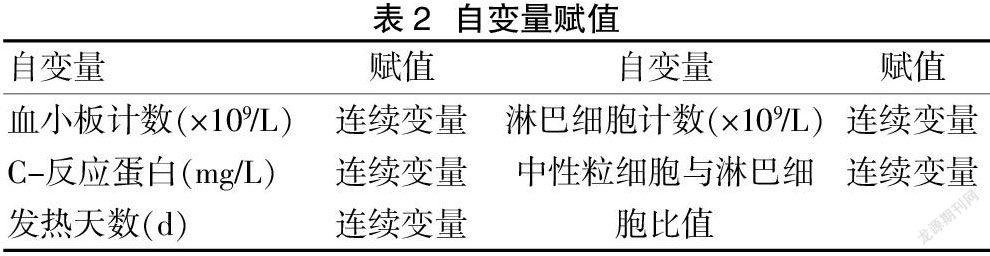
2.3 影响KD患儿IVIg敏感性的影响因素分析
logistic回归分析显示,NLR、C-反应蛋白、PLT的回归系数差异有统计学意义,发热天数、淋巴细胞计数的回归系数差异无统计学意义。NLR、C-反应蛋白、PLT的OR值分别为1.169、1.008、0.996,NLR、C-反应蛋白的OR值大于1,PLT的OR值小于1,说明NLR、C-反应蛋白升高是KD患儿IVIg不敏感的独立危险因素,PLT水平降低是预测IVIg不敏感的独立危险因素。见表2~3。
2.4 各临床指标对KD患儿IVIg敏感性的预测价值
根据ROC曲线,静脉注射免疫球蛋白前PLT对IVIg敏感的最佳预测值是347×109/L,曲线下面积为0.679,敏感度为58.3%,特异度为77.4%;NLR对IVIg敏感的最佳预测值为5.075,曲线下面积为0.679,敏感度为51.6%,特异度为84.5%;C-反应蛋白对IVIg敏感的最佳预测值为80.485 mg/L,曲线下面积为0.652,敏感度为67.7%,特异度为58.3%。见表4。2A8C9683-8A9E-46B4-8DE6-41F3EACD5843
3 讨论
IVIg敏感性预测是KD研究的热点,早期识别IVIg不敏感KD患儿并及时给予强化治疗可改善KD患儿预后。NLR、PLR、SII作为炎症和免疫激活的标志物,已被证实在评估癌症预后与冠状动脉损伤方面有着良好的预测性能。
本研究结果显示,当 NLR>5.075、C-反应蛋白>80.485 mg/L、PLT<347×109/L时应警惕IVIg不敏感。SII、PLR组间比较,差异无统计学意义(P>0.05)。作为炎症和免疫激活的标志物,NLR升高预示着严重炎症反应,与KD早期急性炎症反应过程中中性粒细胞增多和淋巴细胞减少相符[11]。Ha 等[12]研究表明,IVIg不敏感组的NLR高于IVIg敏感组。静脉注射免疫球蛋白前急性发热期IVIg不敏感组的NLR值为5.49,与本研究结果相符。 Liu等[13]研究发现,NLR和PLR是KD患者IVIg不敏感的独立危险因素,但敏感度和特异度中等, 预测IVIg敏感性效能欠佳。Kawamura等[14]发现,NLR≥3.83和PLR≥150×109/L的联合检测对KD患者IVIg敏感性的預测效果较好。本研究结果显示,IVIg敏感组与IVIg不敏感组PLR比较,差异无统计学意义(P>0.05)。重症KD患儿血小板计数呈下降趋势[15-16]。本研究结果显示,IVIg不敏感组的血小板计数、淋巴细胞计数低于IVIg敏感组,但淋巴细胞计数下调组间比较,差异无统计学意义(P>0.05),IVIg不敏感组与IVIg敏感组PLT比较,差异有统计学意义(P>0.05),与Kawamura等[14]研究结果不符。所以在静脉注射免疫球蛋白前NLR对KD患儿IVIg不敏感的预测能力较PLR更有意义。SII是一种融合淋巴细胞、中性粒细胞和血小板计数信息的综合性炎症指标,较高的SII比NLR和PLR更能反映疾病的炎症状态和免疫平衡[17-19]。Liu等[20]发现,IVIg不敏感 KD患儿的SII显著升高,但对于有血小板减少的KD患儿,IVIg不敏感组与IVIg敏感组的SII比较,差异无统计学意义(P>0.05)。本研究并未发现两组间SII比较有显著差异。本研究中IVIg不敏感组的血小板计数低于IVIg敏感组,而IVIg不敏感组的NLR高于IVIg敏感组,SII作为两者的综合炎症指标,相互影响,导致两组间SII的差异缩小(P>0.05)。因此,NLR对 KD患儿静脉注射免疫球蛋白敏感性的预测性能较PLR、SII更稳定。
综上所述,当KD患儿NLR>5.075、C-反应蛋白>80.485 mg/L、PLT<347×109/L时应警惕初始剂量IVIg治疗可能不敏感。但本研究为单中心研究,KD患儿115例,均是在发热10 d内接受IVIg(1 g/kg)治疗的初治KD患儿,可能选择偏倚,存在一定的局限性,因此,需要更大规模的多中心研究建立IVIg敏感性和KD患儿之间关系的预测指标。
[参考文献]
[1] Chang RK. Hospitalizations for Kawasaki disease among children in the United States,1988-1997[J].Pediatrics,2002,109(6):e87.
[2] Manlhiot C,Niedra E,McCrindle BW.Long-term management of Kawasaki disease: Implications for the adult patient[J].Pediatrics & Neonatology,2013,54(1):12-21.
[3] Bar-Meir M, Kalisky I, Schwartz A, Somekh E, Tasher D; Israeli Kawasaki Group. Prediction of resistance to intravenous immunoglobulin in children with kawasaki disease[J].J Pediatric Infect Dis Soc,2018,7(1):25-29.
[4] Kibata T,Suzuki Y,Hasegawa S,et al. Coronary artery lesions and the increasing incidence of Kawasaki disease resistant to initial immunoglobulin[J].International Journal of Cardiology, 2016, 214:209-215.
[5] Seiichiro T,Takashi K,Yoichi K,et al. A comparison of the predictive validity of the combination of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio and other risk scoring systems for intravenous immunoglobulin (ivig)-resistance in Kawasaki disease[J].PLos One, 2017, 12(5):e0176 957.
[6] Chantasiriwan N,Silvilairat S,Makonkawkeyoon K,et al. Predictors of intravenous immunoglobulin resistance and coronary artery aneurysm in patients with Kawasaki disease[J]. Paediatr Int Child Health,2018,38(3):209-212.2A8C9683-8A9E-46B4-8DE6-41F3EACD5843
[7] Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma[J].Clinical Cancer Research, 2014, 20(23):6212-6222.
[8] Yang YL,Wu CH,Hsu PF,et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease[J].Eur J Clin Invest,2020,50(5):e13 230.
[9] Newburger JW,Takahashi M,Gerber MA,et al. Diagnosis,treatment,and long-term management of Kawasaki disease:A statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association[J].Pediatrics,2004,114(6):1708-1733.
[10] Okada K, Hara J, Maki I,et al. Pulse methylprednisolone with gammaglobulin as an initial treatment for acute Kawasaki disease[J].European Journal of Pediatrics,2009,168(2):181-185.
[11] Zahorec R.Ratio of neutrophil lymphocyte counts-rapid and simple parameter of systemic inflammation and stress in critically ill[J].Bratislavske Lekarske Listy,2001,102(1):5-14.
[12] Ha KS,Lee J,Jang GY,et al. Value of neutrophil-lymphocyte ratio in predicting outcomes in Kawasaki disease[J].Am J Cardiol,2015,116(2):301-306.
[13] Liu X, Zhou K, Hua Y,et al. Prospective evaluation of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for intravenous immunoglobulin resistance in a large cohort of Kawasaki disease patients[J].Pediatr Infect Dis J,2020,39(3):229-231.
[14] Kawamura Y, Takeshita S, Kanai T,et al. The combined usefulness of the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in predicting intravenous immunoglobulin resistance with Kawasaki disease[J].J Pediatr,2016,178:281-284.
[15] Kobayashi T. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease[J].Circulation,2006,113(22):2606-2612.
[16] Egami K,Muta H,Ishii M,et al. Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease[J].Journal of Pediatrics,2006,149(2):237-240.
[17] Topkan E,Besen AA,Ozdemir Y,et al. Prognostic value of pretreatment systemic immune-inflammation index in glioblastoma multiforme patients undergoing postneurosurgical radiotherapy plus concurrent and adjuvant temozolomide[J].Mediators Inflamm,2020,2020:4392 189.
[18] Tsilimigras DI,Moris D,Mehta R,et al. The systemic immune-inflammation index predicts prognosis in intrahepatic cholangiocarcinoma:An international multi-institutional analysis[J]. HPB (Oxford),2020,22(12):1667-1674.
[19] Aziz MH,Sideras K,Aziz NA,et al. The systemic-immune-inflammation index independently predicts survival and recurrence in resectable pancreatic cancer and its prognostic value depends on bilirubin levels: A retrospective multicenter cohort study[J].Ann Surg,2019,270(1):139-146.
[20] Liu X,Shao S,Wang L,et al. Predictive value of the systemic immune-inflammation index for intravenous immunoglobulin resistance and cardiovascular complications in Kawasaki disease[J]. Front Cardiovasc Med,2021,8:711 007.
(收稿日期:2021-10-08)2A8C9683-8A9E-46B4-8DE6-41F3EACD5843
