PCT、IL-6、CysC联合检测对脓毒症急性肾损伤诊断及预后评估的价值
2025-02-15宋虎朱键符永玫张永标郑常龙
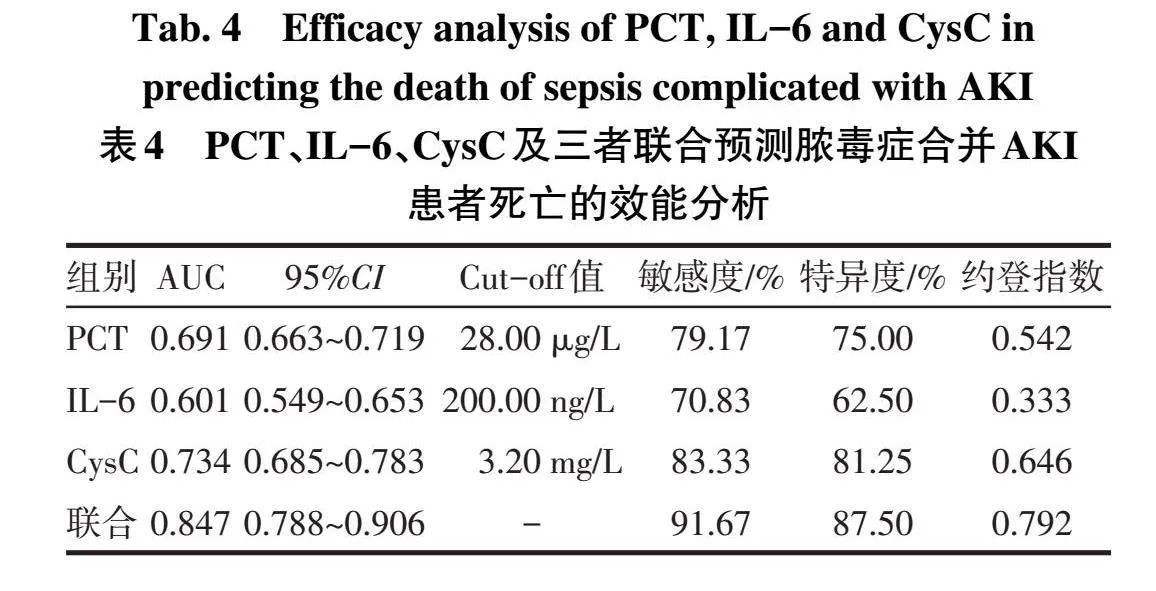





摘要:目的探讨降钙素原(PCT)、白细胞介素6(IL-6)、胱抑素(CysC)联合检测在脓毒症急性肾损伤(AKI)诊断及预后评估中的价值。方法100例脓毒症患者根据AKI发生情况分为AKI组(n=56)和无AKI组(n=44);AKI患者分为存活组(n=32)和死亡组(n=24)。收集患者临床资料,采用酶联免疫吸附试验检测PCT、IL-6、CysC水平;急性生理功能和慢性健康状况评分(APACHEⅡ)评估病情;采用受试者工作特征(ROC)曲线评估PCT、IL-6、CysC对脓毒症合并AKI诊断及死亡的预测价值。结果AKI组男性比例、年龄、高血压合并糖尿病比例、APACHEⅡ评分、血肌酐(Scr)、PCT、IL-6、CysC水平高于非AKI组,合并症比例、发病时间低于非AKI组(P<0.05)。ROC曲线结果显示,PCT、IL-6、CysC联合诊断脓毒症合并AKI的曲线下面积(AUC)为0.859,敏感度为91.07%,特异度为90.91%,联合诊断效能优于单一指标。死亡组APACHEⅡ评分、PCT、IL-6、CysC水平高于存活组(P<0.05)。ROC曲线结果显示,PCT、IL-6、CysC联合预测脓毒症合并AKI患者死亡的AUC为0.847,敏感度为91.67%,特异度为87.50%,联合预测效能优于单一指标。结论联合PCT、CysC、IL-6指标对脓毒症合并AKI诊断以及预后预测的价值更高。
关键词:脓毒症;急性肾损伤;预后;降钙素原;白细胞介素6;半胱氨酸蛋白酶抑制物C
中图分类号:R692文献标志码:A DOI:10.11958/20240835
The value of combined detection of PCT,IL-6 and CysC for the diagnosis and prognosisassessment of septic acute kidney injury
SONG Hu,ZHU Jian,FU Yongmei,ZHANG Yongbiao,ZHENG Changlong△
Department of Emergency Medicine,the Third Affiliated Hospital of Sun Yat-sen University,Guangzhou 510630,China
△Corresponding Author E-mail:zhchl5@mail.sysu.edu.cn
Abstract:Objective To explore the diagnostic and prognostic values of procalcitonin(PCT),interleukin 6(IL-6)and cystatin C(CysC)combined detection in sepsis acute kidney injury(AKI).Methods A total of 100 patients with sepsis were divided into the AKI group(n=56)and the non AKI group(n=44)according to the occurrence of AKI.The prognosis of AKIpatients was followed up,and patients were divided into the survival group(n=32)and the death group(n=24)according to the presence or absence of death.Enzyme-linked immunosorbent assay(ELISA)was used to detect PCT,IL-6 and CysC in different groups"of patients.The Acute Physiological Function and Chronic Health Status Score(APACHEⅡ)was used to assess the condition of illness.ROC curve was used to analyze the predictive values of PCT,IL-6 and CysC in the diagnosis and death of sepsis combined with AKI.Results The male ratio,age,hypertension with diabetes ratio,APACHEⅡscore,serum creatinine(Scr),PCT,IL-6 and CysC levels were higher in the AKI group than those in the non AKI group,and the ratio of complications and onset time were lower in the AKI group than those in the non AKI group(P<0.05).The ROC curve results showed that the area under the curve(AUC)of PCT,IL-6,and CysC combined for the diagnosis of sepsis complicated with AKI was 0.859,with a sensitivity of 91.07%and a specificity of 90.91%.The combined diagnostic efficacy was better than that of a single indicator.The APACHEⅡscore,PCT,IL-6 and CysC levels were higher in the death group than those in the survival group(P<0.05).The ROC curve results showed that the AUC,sensitivity and specificity of PCT,IL-6 and CysC combined in predicting mortality in sepsis patients with AKI were 0.847,91.67%and 87.50%,respectively.The combined predictive efficacy was better than that of single indicator.Conclusion The combination of PCT,CysC and IL-6 indicators is more valuable in diagnosing and predicting prognosis of sepsis with AKI.
Key words:sepsis;acute kidney injury;prognosis;procalcitonin;interleukin-6;cystatin C
脓毒症是一种感染反应失调引起的器官功能障碍综合征,主要临床表现为发热、呼吸急促、精神状态改变等[1]。急性肾损伤(acute kidney injury,AKI)是脓毒症常见的并发症,发病率约为50%[2]。AKI不仅会引起水电解质紊乱和水肿,还会加重病情,增加患者死亡风险。有研究显示,脓毒症合并AKI患者的病死率达52.2%[3]。既往临床诊断AKI以尿量、肌酐等指标为主,存在一定的滞后性。研究发现炎症反应相关指标、肾小球滤过率与脓毒症合并AKI的发生有关[4]。降钙素原(procalcitonin,PCT)是近年较常见的脓毒症诊断预测指标之一,研究证实其与脓毒症病情发展有关,且在肾损伤中过表达[5]。白细胞介素6(interleukin-6,IL-6)是一种多功能细胞因子,已被证实与多种炎症反应的发生有关,可反映炎症对肾功能的影响情况[6]。胱抑素(Cystatin C,CysC)仅通过肾小球被排出体外,其水平变化与肾小球滤过率相关[7]。目前关于PCT、IL-6、CysC联合用于脓毒症合并AKI的研究尚少见。鉴于此,本研究旨在探讨PCT、IL-6、CysC及三者联合检测对脓毒症合并AKI诊断及预后评估的价值,以期为临床诊断与治疗提供参考。
1对象与方法
1.1研究对象选择2021年8月—2023年12月我院收治的脓毒症患者100例,其中男68例,女32例,年龄20~100岁,平均(61.16±17.63)岁。根据AKI发生情况分为AKI组(n=56)和无AKI组(n=44)。诊断标准:(1)脓毒症。参考《第三版脓毒症与感染性休克定义的国际共识》[8],推荐对于基础器官功能障碍状态未知的患者,设定其基线序贯器官衰竭评估(sequential organ failure assessment score,SOFA)为0,感染后SOFA快速增加≥2分作为脓毒症器官功能障碍的临床判断标准。急诊通常使用快速序贯器官衰竭评估(quick SOFA,qSOFA)来快速判断脓毒症,包括意识状态改变、收缩压(SBP)≤100 mmHg(1 mmHg=0.133 kPa)和呼吸频率≥22次/min共3项,符合2项或以上,即qSOFA评分≥2分则诊断为脓毒症。(2)AKI。48 h内肾功能突然减退,血肌酐(serum creatinine,Scr)升高>25 mmol/L,或Scr较前升高>50%,或尿量减小(尿量<0.5 mL·kg-1·h-1且持续超过6 h)[9]。纳入标准:(1)年龄≥18岁。(2)病历资料完整。(3)发病前认知和语言表达正常,能够进行有效的交流。排除标准:(1)入组前3个月内接受过造影剂检查或服用过可能影响肾功能的药物。(2)其他器官功能障碍性疾病。(3)恶性肿瘤、急性心脑血管疾病、自身免疫性疾病。(4)既往有肾功能衰竭病史或需透析治疗者。(5)入院后24 h内死亡者。(6)肾移植手术史、独肾病史。患者入院时均签署医疗标本及数据使用知情同意书,本研究经医院伦理委员会批准(批件号:II2024-082-01)。
1.2研究方法
1.2.1资料收集于入院24 h内收集患者性别,年龄,体质量指数(BMI),感染部位(皮肤软组织、呼吸道、泌尿系统、腹腔),合并症[高血压、糖尿病、高血压合并糖尿病、其他(冠心病、高脂血症)],发病时间(出现发热、寒战、呼吸急促等脓毒症疑似症状至入院就诊的时间),机械通气,感染性休克等资料。
1.2.2心率、血压、尿量检测采用BeneVision N22生命监护仪(深圳迈瑞生物医疗电子股份有限公司)检测患者入院时心率;用无创袖带检测SBP、舒张压(DBP)并计算平均动脉压(mean arterial pressure,MAP);观察并记录患者入院后初始24 h的尿量。
1.2.3血清指标检测入院时采集患者肘静脉血5 mL,3 000 r/min离心10 min,用HISCL-5000型全自动化学发光免疫分析仪(希森美康)检测血清Scr、白细胞计数(WBC)水平;采用酶联免疫吸附试验(试剂盒购自上海纪宁实业)检测血清PCT、IL-6、CysC水平。
1.2.4量表评估采用急性生理功能和慢性健康状况评分(acute physiology and chronic health evaluation,APACHEⅡ)评估病情,评估项目包括急性生理学评分、慢性健康状况评分、年龄3部分,分别计0~60分、2~5分、0~6分,APACHEⅡ总分71分,分数越高,病情越严重。
1.2.5随访患者出院后对其预后情况进行3个月的随访,包括APACHEⅡ评分、肾功能恢复情况等。根据患者生存情况分为存活组(n=32)和死亡组(n=24)。
1.3统计学方法采用SPSS 25.0软件处理数据。计量资料以x±s表示,2组间比较采用独立样本t检验;计数资料以例或例(%)表示,组间比较采用χ2检验;采用受试者工作特征(ROC)曲线评估PCT、IL-6、CysC及三者联合对脓毒症合并AKI诊断及死亡的预测价值。P<0.05为差异有统计学意义。
2结果
2.1 2组一般资料及检查结果的比较2组患者BMI、感染部位、机械通气、感染性休克、心率、SBP、DBP、MAP、24 h尿量、WBC、死亡率差异均无统计学意义(P>0.05);AKI组男性比例、年龄、高血压合并糖尿病比例、APACHEⅡ评分、Scr、PCT、IL-6、CysC水平高于非AKI组,发病时间低于非AKI组(Plt;0.05),见表1。
2.2 PCT、IL-6、CysC对脓毒症合并AKI的诊断效能以脓毒症患者是否合并AKI为状态变量(未合并=0,合并=1),以PCT、IL-6、CysC水平为检验变量,并构建3项指标联合诊断时的联合变量(同时满足PCT≥20.00µg/L、IL-6≥150.00 ng/L、CysC≥2.00 mg/L),绘制ROC曲线,分析PCT、IL-6、CysC及3项指标联合在脓毒症合并AKI诊断中的应用价值。结果显示,PCT、IL-6、CysC联合诊断脓毒症合并AKI的效能优于单一指标,见表2、图1。
2.3 AKI组死亡与存活患者一般资料及检查结果的比较2组患者性别、年龄、BMI、感染部位、合并症、发病时间、机械通气、感染性休克、心率、SBP、DBP、MAP、24 h尿量、Scr、WBC差异均无统计学意义(P>0.05);死亡组APACHEⅡ评分、PCT、IL-6、CysC水平高于存活组(P<0.05),见表3。
2.4 PCT、IL-6、CysC对脓毒症合并AKI死亡的预测效能以脓毒症合并AKI患者的预后情况为状态变量(生存=0,死亡=1),以PCT、IL-6、CysC水平为检验变量,并构建3项指标联合诊断时的联合变量(同时满足PCT≥28.00µg/L、IL-6≥200.00 ng/L、CysC≥3.20 mg/L),绘制ROC曲线,分析PCT、IL-6、CysC及3项指标联合在脓毒症合并AKI预后预测中的应用价值。结果显示,PCT、IL-6、CysC联合预测脓毒症合并AKI患者死亡的效能优于单一指标(P<0.05),见表4、图2。
3讨论
脓毒症是指明确或可疑的感染引起的全身炎症反应综合征。有研究证实,随患者机体炎症反应的加重,可能增加多器官功能障碍综合征的发生风险,从而对各器官功能造成严重损害[10]。AKI的发生会加重患者病情,增加临床诊疗难度,致患者死亡率升高。研究报道,在重症患者中脓毒症合并AKI的发病率以每年0.3%趋势递增,总体病死率为26.5%~45.0%[11]。强化脓毒症合并AKI的早期诊断预测方式,为疾病的早期预防和治疗提供参考,对降低脓毒症合并AKI患者的病死率有重要意义。
PCT是机体出现全身炎症反应时释放的一种急性可溶性蛋白,属免疫活性蛋白,主要有调节免疫功能和血管收缩状态的作用。PCT作为降钙素的前体,当机体受到病原微生物感染和炎症刺激时,血浆中PCT水平显著升高。既往研究表明,在脓毒症诊断中PCT的AUC高于C反应蛋白,略低于IL-6和乳酸[12]。PCT对病原微生物感染敏感性较高,利于脓毒症的早期诊断及病情预测。一般情况下,PCT由甲状腺C细胞产生,并被特殊的酶分解,脓毒症发生后会对相关酶活性造成影响,使得PCT分解过程被抑制,大量PCT被释放进入血液循环。有研究证实,PCT在脓毒症诊断中有较高应用价值,利于脓毒症病情的诊断预测[13]。本研究结果显示,AKI组患者PCT高于非AKI组,且死亡组PCT高于存活组,与邓亮等[14-15]研究结论一致,提示脓毒症不同病情、不同预后者的PCT差异显著,即脓毒症所致炎症反应越严重,PCT呈现的水平越高,炎症反应对肾功能的损害越显著。沈侃等[16]研究亦表明,PCT是脓毒症持续性AKI早期诊断的独立预测因子,PCT进行性升高与确诊脓毒症后持续性AKI发病有关。同时,随肾功能损伤加重,肾小球滤过率下降,PCT经肾脏代谢、排出量减少,大量PCT蓄积在体内,血PCT相应升高[17]。
IL-6作为肝细胞刺激因子,在感染或外伤引起的急性炎症反应中诱导急性期反应蛋白的合成,其中以淀粉样蛋白a和C-反应蛋白增加尤为明显。Lukas等[18]研究显示,IL-6是脓毒症发生的危险因素,其与脓毒症的发生发展密切相关。本研究结果显示,AKI组患者IL-6高于非AKI组,且死亡组IL-6高于存活组,与金仁华等[19]发现的持续性脓毒症AKI患者的IL-6水平更高结论近似。苏秦等[20]指出,脓毒症伴肾损伤者的IL-6变化与机体免疫功能密切相关。IL-6作为常见的促炎因子,其水平升高多提示机体炎症反应加重,体液免疫功能下降,随病情发展可能会对肾实质造成持续性损伤;且严重炎症反应会影响肾脏及周围血液循环,导致肾脏出现缺血、缺氧,易形成恶性循环,进一步加重局部炎症,最终增加预后不良发生风险。若脓毒症患者IL-6水平显著升高,提示机体炎症较重,肾功能损伤风险较高,AKI发生风险及病死率显著上升。
CysC是一种小分子非糖化蛋白质,主要通过肾小球滤过。有研究证实CysC在肾功能诊断预测中有一定应用价值[21]。本研究结果显示,AKI组患者CysC高于非AKI组,死亡组高于存活组,与许慧慧等[22-23]研究中CysC在脓毒症合并AKI中高表达,脓毒症合并AKI死亡者的CysC高于存活者等结论一致,提示CysC水平变化可能与脓毒症患者的病情发展及AKI患者预后有密切联系。李晓玲等[24]研究显示,脓毒症合并AKI患者的CysC水平与凝血酶原时间、活化部分凝血酶时间呈正相关。脓毒症后凝血功能的变化是影响AKI发生的重要因素[25]。赵鹏等[26]研究表明,脓毒症AKI患者的CysC水平与肾动脉阻力指数呈正相关。炎症反应的加重可能引起急性肾小管坏死,进而影响机体凝血功能及肾脏血供情况,诱导肾小管上皮细胞发生不可逆性损伤,介导AKI的发生。若脓毒症患者CysC水平升高,提示机体凝血功能发生变化、肾动脉阻力指数升高,肾功能下降,肾脏损伤程度加重,AKI患病风险及病死率显著上升。
此外,本研究结果显示,PCT、IL-6、CysC联合诊断脓毒症合并AKI和预测脓毒症合并AKI患者死亡的应用价值均高于单一指标。PCT、IL-6能有效反映受检者机体炎症反应的严重程度,为脓毒症的严重程度和发展趋势提供重要参考;CysC能反映肾功能及肾脏损伤程度,利于医生诊断并预测脓毒症患者的肾损伤情况。适当考虑联合3项指标对脓毒症患者进行检查诊断,能为患者的AKI发生和死亡风险提供重要量化参考依据。
综上所述,PCT、CysC、IL-6均在脓毒症合并AKI及脓毒症合并AKI死亡者中高表达,能为脓毒症合并AKI诊断以及预后预测提供重要参考,且三项指标联合的诊断预测价值更高。本研究不足之处在于样本量较少,结果可能存在偏倚,后期希望能够扩大样本量,以期为AKI的实验室诊断、预后预测指标的选择提供更多参考。
参考文献
[1]JONATHAN S C,MIGUEL I E,ALEJANDRO M G,et al.Probiotics in septic acute kidney injury,adouble blind,randomized control trial[J].Ren Fail,2023,45(2):2260003.doi:10.1080/0886022X.
[2]肖涛,吴锡平,关云艳,等.脓毒症相关性急性肾损伤的危险因素分析[J].医学综述,2018,24(20):4133-4136.XIAO T,WU X P,GUAN Y Y,et al.Analysis of risk factors for sepsis-associated acute kidney injury[J].Med Rec,2018,24(20):4133-4136.doi:10.3969/j.issn.1006-2084.2018.20.033.
[3]王娜,李培兰.脓毒症合并急性肾损伤的危险因素及预后分析[J].内科急危重症杂志,2018,24(3):198-200,209.WANG N,LI P L.Risk factors and clinical prognosis in patients with septic AKI in emergency intensive care unit[J].Journal of Internal Intensive Medicine,2018,24(3):198-200,209.doi:10.11768/nkjwzzzz20180307.
[4]任广胜,胡善友,张和凤,等.血清胱抑素C联合血乳酸对脓毒症急性肾损伤早期诊断的价值[J].中国急救复苏与灾害医学杂志,2019,14(6):540-543.REN G S,HU S Y,ZHANG H F,et al.The value of combined cystatin C and lactic acid in early diagnosis of sepsis complicated with acute kidney injury[J].China Journal of Emergeney Resuscitation and Disaster Medicine,2019,14(6):540-543.doi:10.3969/j.issn.1673-6966.2019.06.013.
[5]SHANG Y X,ZHRNG Z,WANG M,et al.Diagnostic performance of Neutrophil CD64 index,procalcitonin,and C-reactive protein for early sepsis in hematological patients[J].World J Clin Cases,2022,10(7):2127-2137.doi:10.12998/wjcc.v10.i7.2127.
[6]FENG J Q,ZHANG S Y,AI T Y,et al.Effect of CRRT with oXiris filter on hemodynamic instability in surgical septic shock with AKI:a pilot randomized controlled trial[J].Int J Artif Organs,2022,45(10):801-808.doi:10.1177/03913988221107947.
[7]易雪琳,欧阳亮.血清CysC、UmAlb、Scr在脓毒症合并急性肾损伤患者中的表达及疾病预测价值[J].国际泌尿系统杂志,2022,42(1):72-76.YI X L,OUYANG L.Expression and predictive value of serum CysC,UmAlb and Scr in patients with sepsis and acute kidney injury[J].Int J Urol Nephro,2022,42(1):72-76.doi:10.3760/cma.j.cn431460-20210115-00018.
[8]SINGER M,DEUTSCHMAN C S,SEYMOUR C W,et al.The third international consensus definitions for sepsis and septic shock(Sepsis-3)[J].JAMA,2016,315(8):801-810.doi:10.1001/jama.2016.0287.
[9]中华医学会肾脏病学分会专家组.新型冠状病毒感染合并急性肾损伤诊治专家共识[J].中华肾脏病杂志,2020,36(3):242-246.Expert Group of the Nephrology Branch of the Chinese Medical Association.Expert consensus on diagnosis and treatment of 2019 novel coronavirus(2019-nCoV)infection with acute kidney injury[J].Chin J Neahrol,2020,36(3):242-246.doi:10.3760/cma.j.cn441217-20200222-00035.
[10]管光辉,浦秦华,钱何布.脓毒症并发急性肾损伤患者血清MMP-13、VASH-1水平与预后相关性[J].天津医药,2023,51(12):1360-1364.GUAN G H,PU Q H,QIAN H B.Correlation between serum levels of MMP-13,VASH-1 and prognosis in patients with sepsis complicated with acute kidney injury[J].Tianjin Med J,2023,51(12):1360-1264.doi:10.11958/20230928.
[11]徐丽,孙鹏.脓毒症相关性急性肾损伤的识别和管理[J].中华危重病急救医学,2023,35(2):221-224.XU L,SUN P.Identification and management of sepsis associated-acute kidney injury[J].Chin Crit Care Med,2023,35(2):221-224.doi:10.3760/cma.j.cn121430-20220808-00725.
[12]孙伟,何燕超,张山,等.血清降钙素原和常用炎症指标与老年脓毒症的相关性及结合重症评分对其预后的评价[J].老年医学与保健,2021,27(2):290-295.SUN W,HE Y C,ZHANG S,et al.The predict value of procalcitonin,common inflammatory indicators combined with critical illness score in diagnosis and prognosis of sepsis in the elderly patients[J].Geriatr Heal Care,2021,27(2):290-295.doi:10.3969/j.issn.1008-8296.2021.02.021.
[13]WALID A A,NAGLAA S B,AHMED A E,et al.A randomized trial to compare procalcitonin and C-reactive protein in assessing severity of sepsis and in guiding antibacterial therapy in Egyptian critically ill patients[J].Ir J Med Sci,2021,190(4):1487-1495.doi:10.1007/s11845-020-02494-y.
[14]邓亮,郭碧君,邹燕群,等.尿中性粒细胞明胶酶相关脂质运载蛋白、血降钙素原及全身免疫炎症指数在脓毒症继发急性肾损伤中表达的临床意义[J].实用医院临床杂志,2023,20(4):99-103.DENG L,GUO B J,ZOU Y Q,et al.Expression and clinical significance of urinary neutrophil gelatinase-associated lipocalin,pro-calcitonin combined with systemic immune inflammatory index in patients with acute kidney injury secondary to sepsis[J].Pra J Clin Med,2023,20(4):99-103.doi:10.3969/j.issn.1672-6170.2023.04.024.
[15]杨建海,张颖,张晓强.血清PCT、hs-CRP及Th17细胞对脓毒症相关急性肾损伤患者行连续肾脏替代治疗法结局的预测价值[J].东南大学学报(医学版),2023,42(4):572-577.YANG J H,ZHANG Y,ZHANG X Q.Predictive value of serum PCT,hs-CRP,and Th17 cell in the outcome of continuous renal replacement therapy in patients with acute renal injury caused by sepsis[J].Journal of Southeast University(Medical Science Edition),2023,42(4):572-577.doi:10.3969/j.issn.1671-6264.2023.04.013.
[16]沈侃,许东伟,李俊,等.动态监测降钙素原对脓毒症急性肾损伤近期恢复预测价值[J].医学综述,2022,28(11):2276-2282.SHEN K,XU D W,LI J,et al.Predictive value of dynamic monitoring of procalcitonin for short-term recovery of acute kidney injury in sepsis[J].Med Rec,2022,28(11):2276-2282.doi:10.3969/j.issn.1006-2084.2022.11.034.
[17]周双炉,常玲,邢芳芳.PCT、NLR、N/LPR对重症急性胰腺炎并发急性肾损伤的预测价值[J].新医学,2022,53(2):133-137.ZHOU S L,CHANG L,XING F F.Value of PCT,NLR and N/LPR in predicting acute kidney injury in patients with severe acute pancreatitis[J].New Med,2022,53(2):133-137.doi:10.3969/j.issn.0253-9802.2022.02.012.
[18]LUKAS Z,MELANIE K,ALEXANDER H,et al.Sepsis induces interleukin 6,gp130/JAK2/STAT3,and muscle wasting[J].J Cachexia Sarcopenia Muscle,2022,13(1):713-727.doi:10.1002/jcsm.12867.
[19]金仁华,李静,沈骁,等.肝素结合蛋白联合白介素-6对持续性脓毒症急性肾损伤的预测价值[J].临床急诊杂志,2023,24(3):119-125.JIN R H,LI J,SHEN X,et al.Predictive value ofheparin-binding protein combined with interleukin-6 in different subtypes of sepsis associated acute kidney injury[J].Journal of Clinical Emergency,2023,24(3):119-125.doi:10.13201/j.issn.1009-5918.2023.03.003.
[20]苏秦,高进,付俊鲜,等.血流动力学指标和IL-6在脓毒症肾损伤患儿中的表达及其与免疫指标的相关性[J].中国免疫学杂志,2020,36(10):1235-1239.SU Q,GAO J,FU J X,et al.Expression of hemodynamic parameters and interleukin-6 in children with septic renal injury and their correlation with immune parameters[J].Chinese Journal of Immunology,2020,36(10):1235-1239.doi:10.3969/j.issn.1000-484X.2020.10.016.
[21]YANG Y W,GE B,LIU Y,et al.The efficacy of biomarkers in the diagnosis of acute kidney injury secondary to liver cirrhosis[J].Medicine(Baltimore),2021,100(14):e25411.doi:10.1097/MD.0000000000025411.
[22]许慧慧,吴维雄,于航,等.老年脓毒症诱发急性肾损伤患者血清NGAL、CysC水平变化及诊断价值研究[J].中国实验诊断学,2020,24(7):1138-1140.XU H H,WU W X,YU H,et al.Changes and diagnostic value of serum NGAL and CysC levels in elderly patients with acute renal injury induced by sepsis[J].Chinese Journal of Laboratory Diagnosis,2020,24(7):1138-1140.doi:10.3969/j.issn.1007-4287.2020.07.022.
[23]HIBA S A,SHIMAA A,ZEINAB A K,et al.Potential value of TNF-α(-376 G/A)polymorphism and cystatin C(CysC)in the diagnosis of sepsis associated acute kidney injury(S-AK I)and prediction of mortality in critically Ill patients[J].Front Mol Biosci,2021,8(10):751299.doi:10.3389/fmolb.2021.751299.
[24]李晓玲,周文杰,邓伟,等.凝血指标联合血清胱抑素C对脓毒症急性肾损伤患者预后的预测价值[J].实用医学杂志,2023,39(1):81-85.LI X L,ZHOU W J,DENG W,et al.Prognostic value of coagulation function index combined with serum cystatin C in patients with septic acute kidney injury[J].J Pra Med,2023,39(1):81-85.doi:10.3969/j.issn.1006-5725.2023.01.014.
[25]张春芳,王慧娟.脓毒症继发急性肾损伤过程中的凝血变化[J].标记免疫分析与临床,2022,29(1):15-18.ZHANG C F,WANG H J.The coagulation of acute kidney injury of sepsis patients[J].Lab Immun Clin Med,2022,29(1):15-18.doi:10.11748/bjmy.issn.1006-1703.2022.01.004.
[26]赵鹏,赵娟,田静朴,等.脓毒症合并急性肾损伤患者生物学标志物检测及其与肾动脉阻力指数的关系[J].临床和实验医学杂志,2019,18(7):730-733.ZHAO P,ZHAO J,TIAN J P,et al.Detection of biomarkers in patients with sepsis complicated with acute kidney injury and its relationship with renal artery resistance index[J].Clin Exp Med,2019,18(7):730-733.doi:10.3969/j.issn.1671-4695.2019.07.018.
(2024-06-27收稿2024-10-17修回)
(本文编辑陈丽洁)
