链脲佐菌素糖尿病小鼠睾丸内生精细胞减少与PCNA和K i67表达降低
2017-07-31樊芙蓉张夔鸣唐兆生朱珍华燕菲肖天羽汪琳
樊芙蓉,张夔鸣,唐兆生,朱珍,华燕菲,肖天羽,汪琳
(上海市东方医院1整形外科,2神经外科,3内分泌科,4病理科, 上海 200120;5武汉大学基础医学院组织学与胚胎学教研室,武汉 430071)
链脲佐菌素糖尿病小鼠睾丸内生精细胞减少与PCNA和K i67表达降低
樊芙蓉1,张夔鸣2,唐兆生3,朱珍4,华燕菲4,肖天羽4,汪琳5*
(上海市东方医院1整形外科,2神经外科,3内分泌科,4病理科, 上海 200120;5武汉大学基础医学院组织学与胚胎学教研室,武汉 430071)
目的通过检测增殖细胞核抗原(proliferating cell nuclear antigen, PCNA)及Ki67在正常及糖尿病小鼠睾丸组织中表达的差异,探讨糖尿病对生精细胞增殖的影响。方法30只正常雄性C57BL/6小鼠,随机分为对照组(10只)和糖尿病组(20只)。采用腹腔注射链脲佐菌素的方法建立糖尿病小鼠模型,对照组注射相同体积的柠檬酸—柠檬酸钠缓冲液。造模成功3周后处死动物,取睾丸组织,常规固定、石蜡包埋、切片HE染色观察睾丸组织的形态学变化;免疫组织化学SP法检测PCNA及Ki67在睾丸组织中的表达;图像分析技术分析组织中PCNA及Ki67免疫组织化学表达水平。结果HE染色显示,糖尿病小鼠睾丸内处于精子发生前半期的生精小管内生精细胞排列疏松,细胞层数偏少,附睾管内精子密度相对较低;免疫组织化学染色显示,PCNA和Ki67在糖尿病小鼠睾丸生精小管中的表达均明显降低。结论高糖可能通过降低生精细胞的增殖进而影响睾丸精子的发生。
生精细胞;增殖细胞核抗原;Ki67;糖尿病
糖尿病(diabetes mellitus,DM)是一种由于胰岛素分泌缺陷或胰岛素作用障碍所致的、以高血糖为特征的代谢性疾病。持续高血糖与长期代谢紊乱等可导致全身组织器官,特别是眼、肾、心血管及神经系统的损害及其功能障碍和衰竭。随着DM患病率的逐年升高及发病年轻化,其对生殖功能的影响受到了越来越多的关注,包括对生殖器官的结构、性激素的合成和分泌、生殖细胞发生、性功能及子代健康等方面的影响[1,2]。近年来,对睾丸生精细胞的凋亡及糖尿病基因的筛选有较多的报道[1,3],但对高糖状态是否影响睾丸生精细胞增殖能力的研究资料较为缺乏,因此,本文采用腹腔注射链脲佐菌素的方法建立糖尿病小鼠模型,探讨高糖对睾丸生精细胞增殖能力的影响,以期为DM对雄性生殖功能的影响提供重要的实验依据。
材料与方法
1 糖尿病模型建立
将30只9~10周龄SPF级雄性C57BL/6小鼠 (由本校动物实验室提供)随机分为对照组(n=10)和糖尿病组(n=20),均在本校动物实验室(SPF级)喂养。适应性喂养一周后,糖尿病组小鼠腹腔内注射链脲佐菌素(STZ,Sigma 公司)溶液40mg/kg,对照组注射相同体积的柠檬酸—柠檬酸钠缓冲液(pH值4.2),喂以普通饲料。STZ注射后3周,用微血糖测量仪(ONE TOUCH Sure Step,美国强生)检测空腹血糖。
2 标本制备与染色
造模成功后,用颈椎脱臼法处死两组小鼠,取出双侧的睾丸及附睾,立即放入4%多聚甲醛液中固定,梯度酒精脱水、苯甲酸甲酯透明、石蜡包埋后切片(片厚5μm)。部分切片进行常规HE染色,另一部分采用链霉素亲生物素-过氧化物酶法(SP法)进行PCNA和Ki67免疫组织化学染色。免疫组织化学染色基本步骤如下:①切片脱蜡水化,柠檬酸缓冲液浸泡、微波处理10m in,进行抗原修复;②滴加3%H2O2水溶液,室温放置10m in,蒸馏水洗2m in×2次,PBS洗2m in×3次;③加正常羊血清封闭,37℃孵育10m in;④甩去多余正常血清,加兔抗鼠增殖细胞核抗原(proliferating cell nuclear antigen,PCNA)(1:100,北京博奥森生物技术有限公司)或Ki67(1:100,艾菲生物技术有限公司)多克隆抗体,4℃孵育过夜,PBS冲洗3m in×3次;⑤滴加生物素标记羊抗兔IgG(1:50,Abcam),37℃孵育10m in,PBS冲洗3m in×3次;⑥滴加过氧化物酶标记的链酶素亲和素,37℃孵育10m in,PBS冲洗3m in×3次;⑦滴加新鲜配制的DAB(DAB显色试剂盒,DAKO公司)显色液显色,光镜下控制时间,充分水洗;⑧苏木素复染,常规脱水、透明、封片。阴性对照采用PBS液代替一抗,其余步骤及试剂不变;阳性对照采用自身对照,阴性对照细胞及组织无染色,阳性反应为棕黄色。结果采用HPIAS-1000高清晰度彩色病理图文报告管理系统检测阳性反应颗粒的平均光密度。
3 统计学处理
结 果
1 动物一般情况
对照组小鼠生长情况良好,皮毛光亮,进食进水正常;实验组小鼠随造模时间的延长,动物体重逐渐减轻,活动减少,进食进水量及尿量均明显高于对照组。观察期间对照组和实验组分别死亡0只和2只。实验组小鼠中3只空腹血糖升高不明显(<10mmol/L),余15只均纳入本研究。
2 糖尿病小鼠睾丸内生精细胞减少
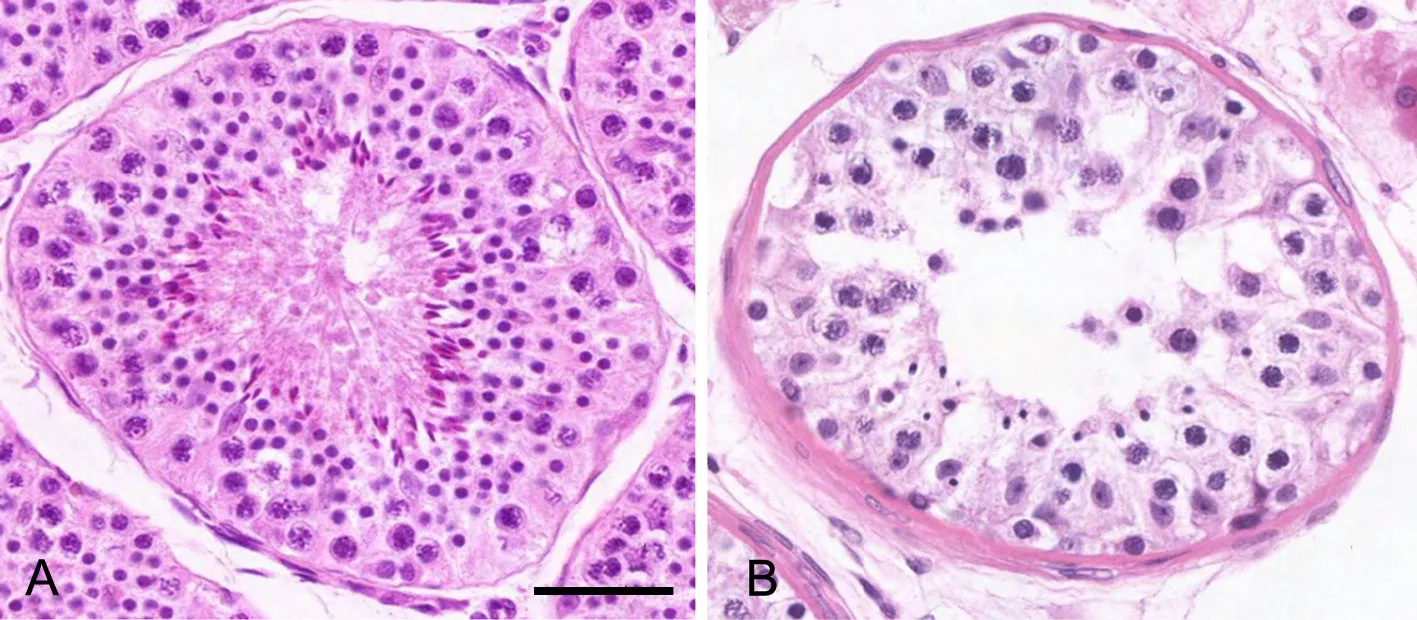
图1 糖尿病小鼠睾丸组织HE染色检测。A,对照组;B,糖尿病组;比例尺,50μmFig. 1 HE staining of the testis tissue of diabetic m ice. A, control group; B, diabetic group; scale bar, 50μm
肉眼观察可见糖尿病小鼠的睾丸及附睾体积偏小。HE染色标本显示,两组小鼠睾丸的精子发生均活跃,生精小管内均可见各级生精细胞(图1A,图1B)。糖尿病小鼠睾丸生精小管内未见生精细胞大量脱落,但少数切片可于精子发生前半期的生精小管内生精细胞排列疏松,细胞层数偏少(图1B),对照组小鼠睾丸切片未见异常(图1A)。此外,糖尿病小鼠睾丸间质萎缩明显,间质中的Leydig细胞形态大小及数量相对较少。
3 糖尿病小鼠生精小管内PCNA与Ki67免疫反应性降低
免疫组织化学染色显示,PCNA及Ki67免疫反应产物均定位于细胞核中,为棕褐色颗粒状;与对照组比较,糖尿病小鼠生精小管中,PCNA及Ki67免疫反应性明显减弱(图2,表1)。
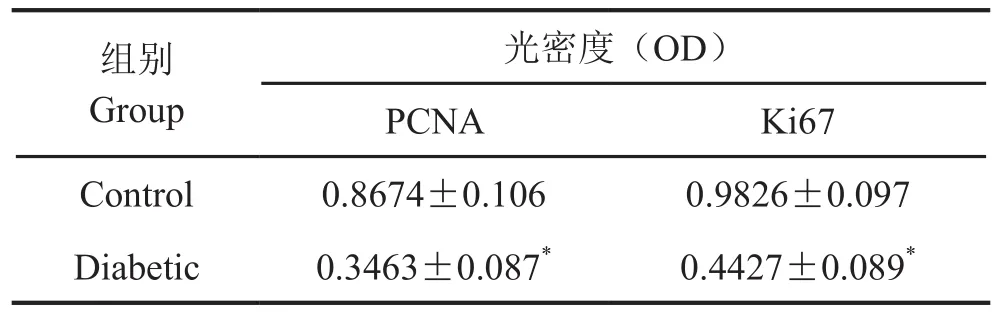
表1 PCNA及Ki67蛋白在正常及糖尿病小鼠睾丸组织中表达水平统计分析Tab. 1 Statistical analysis of the levels of PCNA and Ki67 in the testis tissue of norm al and diabetic m ice
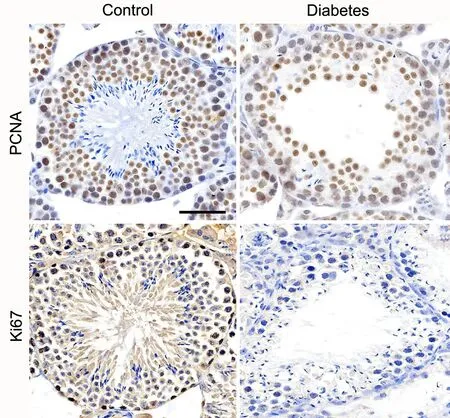
图2 糖尿病小鼠睾丸组织内PCNA和Ki67表达的免疫组织化学检测。比例尺,50μmFig. 2 Immunohistochem ical detection of the expression of PCNA and Ki67 in the testis tissue of diabetic m ice. Scale bar, 50μm
讨 论
糖尿病的慢性高血糖状态对精子的发生有明显影响,但其确切的分子机制至今尚未明了[4-7]。PCNA由M iyachi等于1978年在SLE(系统性红斑狼疮)患者的血清中首次发现,因其只存在于正常增殖细胞及肿瘤细胞内而得名。PCNA是一种分子量为36KD的蛋白质,在细胞核内合成,并存在于细胞核内,为DNA聚合酶δ的辅助蛋白,与细胞DNA合成关系密切[8,9]。在细胞核内存在可溶性与不溶性两种PCNA,可溶性PCNA在细胞周期各期中均有表达,其量在DNA合成过程中不发生明显变化;不溶性PCNA较稳定,在G0~G1期细胞中无明显表达,G1晚期,其表达大幅度增加,S期达到高峰,G2~M期明显下降,其量的变化与DNA合成一致。Ki67也是一种增殖细胞相关的核抗原,其功能与有丝分裂密切相关。Ki67表达范围覆盖除G0期以外的各增殖周期细胞[10]。因此,PCNA和Ki67所携带的增殖信息并非完全一致,两者具有一定的互补性。因此,同时检测PCNA和Ki67的表达更能全面、客观地评价不同功能状态下细胞或组织的增殖活性[11,12]。本文首先建立糖尿病小鼠模型,HE染色标本观察显示两组小鼠睾丸内均可见各级生精细胞,与对照小鼠相比,糖尿病小鼠睾丸内处于精子发生前半期的生精小管内生精细胞排列疏松,细胞层数偏少,附睾管内精子密度相对较低,提示高糖可以影响精子的发生;免疫组织化学结果显示,PCNA及Ki67在糖尿病组小鼠睾丸生精小管中的表达均较正常组对照组明显降低,推测高糖可能通过降低生精细胞的增殖活性进而影响睾丸精子的发生,但其确切机制有待进一步探讨。
[1] Shi GJ, Li ZM, Zheng J, et al. Diabetes associated w ith male reproductive system damages: Onset of presentation, pathophysiological mechanisms and drug intervention. Biomed Pharmacother, 2017, 90: 562-574.
[2] Ding GL, Liu Y, Liu ME, et al. The ef ects of diabetes on male fertility and epigenetic regulation during spermatogenesis. Asian J Androl, 2015, 17(6): 948-953.
[3] Rizvi S, Raza ST, Rahman Q. Role of GNB3, NET, KCNJ11, TCF7L2 and GRL genes single nucleotide polymorphism in the risk prediction of type 2 diabetes mellitus. Biotech, 2016, 6(2): 255.
[4] Kettner LO, Matthiesen NB, Ram lau-Hansen CH, et al. Fertility treatment and childhood type 1 diabetes mellitus: a nationw ide cohort study of 565,116 live births. Fertil Steril, 2016, 106(7): 1751-1756.
[5] Abdelali A, A l-Bader M, Kilarkaje N. Ef ects of Trans-Resveratrol on hyperglycem ia-induced abnormal spermatogenesis, DNA damage and alterations in poly (ADP-ribose) polymerase signaling in rat testis. Toxicol Appl Pharm, 2016, 311: 61-73.
[6] Pergialiotis V, Prodromidou A, Frountzas M, et al. Diabetes mellitus and functional sperm characteristics: A meta-analysis of observational studies. J Diabetes Complicat, 2016, 30(6): 1167-1176.
[7] La Vignera S, Condorelli RA, Di Mauro M, et al. Reproductive function in male patients w ith type 1 diabetes mellitus. Andrology, 2015, 3(6): 1082-1087.
[8] Jo U, Cai W, Wang, JM, et al. PCNA-Dependent Cleavage and Degradation of SDE2 Regulates Response to Replication Stress. PloS Genet, 2016, 12(12): e1006465.
[9] Han X, Lu H, Li S, et al. Cell morphologic changes and PCNA expression w ithin craniofacial sutures during monkey Class III treatment. Orthod Craniofa Res, 2016, 19(4): 181–189.
[10] M in KW, Kim DH, Do SI, et al. High Ki67/BCL2 index is associated w ith worse outcome in early stage breast cancer. Postgrad Med J, 2016, 92 (1094): 707-714.
[11] Cosarca AS, Mocan SL, Pacurar M, et al.The evaluation of Ki67, p53, MCM 3 and PCNA immunoexpressions at the level of the dental follicle of impacted teeth, dentigerous cysts and keratocystic odontogenic tumors. Rom J Morphol Embryol, 2016, 57(2): 407-412.
[12] Jurikova M, Danihel L, Polák Š, et al. Ki67, PCNA, and MCM proteins: Markers of proliferation in the diagnosis of breast cancer. Acta Histochem, 2016, 118(5): 544-552.
Decreased spermatogenic cell number and expression of PCNA and K i67 in streptozotocin-induced diabetic m ice
Fan Furong1, Zhang Kuim ing2, Tang Zhaosheng3, Zhu Zhen4, Hua Yanfei4, Xiao Tianyu4, Wang Lin5*
(1Department of Plastic Surgery,2Department of Neurosurgery,3Department of Endocrinology,4Department of Pathology, Shanghai Dongfang Hospital, Shanghai 200120;5Department of Histology and Embryology, School of Basic Medical Sciences, Wuhan University, Wuhan 430071, China)
ObjectiveTo investigate the expression of proliferating cell nuclear antigen (PCNA) and Ki67 in the testis of normal and diabetic mice so as to study the ef ect of diabetes on the proliferation of spermatogenic cells.M ethodsThirty normal male C57BL/6 m ice were random ly divided into a control group (n=10) and a DM group (n=20). The diabetic model was established by intraperitoneal injection of streptozotocin into C57BL/6 mouse, while the same volume of citric acid-sodium citrate buf er was injected in the control group m ice. The m ice were killed three weeks after model establishment, the testes and epididymes were sampled, f xed, then embedded in paraf n, sectioned, stained by HE, and the morphological changes were observed under microscope. The immunohistochem ical SP method and image analysis technique were employed to detect and analyze the expression of PCNA and Ki67 in the testis tissue.ResultsHE staining showed that in the diabetic group, the germ cells at the earlier stage of the spermatogenic cycle were loosely arranged in the sem iniferous tubule, the number of cell layers was decreased, and the sperm density in the ductus epididym idis was relatively low. Immunohistochemical staining results showed that the expression of PCNA and Ki67 was signif cantly lower in the diabetic group than in the normal group (P<0.01).ConclusionHigh glucose concentration may impact spermatogenesis by inhibiting the proliferation of spermatogenic cells.
Spermatogenic cell; proliferating cell nuclear antigen; Ki67; diabetes mellitus
R329.1
ADOI:10.16705/ j. cnki. 1004-1850.2017.03.002
2017-03-10
2017-06-13
樊芙蓉,女(1972年),汉族,主治医师
*通讯作者(To whom correspondence should be addressed):lin.wang@whu.edu.cn
