甲状腺微小乳头状癌手术方式对肿瘤复发影响的meta分析
2017-06-05伊丹丹黄韬宋鹏桑剑锋
伊丹丹,黄韬,宋鹏,桑剑锋
(1.南京医科大学鼓楼临床医学院 普通外科 江苏 南京 210008;2.南京大学医学院附属南京鼓楼医院 普通外科 江苏 南京 210008)
·论 著·
甲状腺微小乳头状癌手术方式对肿瘤复发影响的meta分析
伊丹丹1,黄韬1,宋鹏2,桑剑锋2
(1.南京医科大学鼓楼临床医学院 普通外科 江苏 南京 210008;2.南京大学医学院附属南京鼓楼医院 普通外科 江苏 南京 210008)
目的:评估不同手术方式对甲状腺微小乳头状癌术后复发的影响。方法:搜索PubMed、中国知网中关于甲状腺微小乳头状癌手术方式及复发情况的相关文献,使用Stata12.0软件进行meta分析。结果:甲状腺全叶切除术与甲状腺非全叶切除术的患者术后复发差异无统计学意义,行颈部淋巴结清扫者较未清扫者术后更易复发。结论:甲状腺微小乳头状癌患者行甲状腺非全叶切除术也是不错的选择。
甲状腺微小乳头状癌;手术方式;复发;meta-分析
甲状腺微小乳头状癌(papillary thyroid microcarcinoma (PTMC))WHO定义是指肿瘤直径≤1cm的甲状腺乳头状癌[1],其发生率逐年递增,2008年达到总人群11.8%[2]。许多文献都报道了PTMC的良好预后[2-5]。目前对PTMC的手术方式存在争议:有些学者认为,尽管PTMC预后良好,但仍有复发、转移和死亡的风险,应行甲状腺全叶切除甚至必要时加作中央区淋巴结清扫[6-8];有些学者则认为,PTMC患者行甲状腺全叶切除实属过度治疗[9],全叶切除并不能降低复发和死亡风险,甲状腺次全甚至腺叶切除即能达到治疗效果[10-12],且能减少甲状腺全叶切除的并发症的发生[13]。此外,Ito等[14]认为,可对于PTMC患者进行观察,若出现疾病进展,再行手术切除。本研究就PTMC的手术方式对肿瘤复发的影响进行meta分析,现报道如下。
1 资料与方法
1.1 文献来源和研究选择
在PubMed数据库中使用检索式“papillary thyroid microcarcinoma and recurrence”、“PMC and recurrence”、“PTMC and recurrence”、“papillary thyroid microcarcinoma and prognosis”、“PMC and prognosis”、“PTMC and prognosis”,在中国知网中使用检索式“甲状腺微小乳头状癌”,检索2016年5月18日以前的英文文献和中文文献。对搜索到所有文献的题目、摘要、关键词进行阅读。纳入标准:(1)已发表的文献,不包括综述;(2)研究对象是PTMC患者;(3)所有研究均有甲状腺全叶切除及非全叶切除手术方式及对应的复发情况数据;(4)研究样本>50人,且均进行了术后的随访,P值均设定为0.05。其中甲状腺全叶切除术包括单纯甲状腺全叶切除或甲状腺全叶切除+颈部淋巴结清扫术,即不管是否行淋巴结清扫,只要甲状腺仍有残留均纳入甲状腺非全叶切除组。
1.2 数据提取
包括研究作者、论文发表时间、样本量、甲状腺全叶切除后发生或未发生复发的事件数,甲状腺非全叶切除后发生或未发生复发的事件数。
1.3 资料分析
使用Stata12.0软件进行meta分析,在综合研究之前先对异质性进行研究。如果异质性大于50%应用随机效应模型;如果异质性≤50%应用固定效应模型。应用比值比(odds ratio,OR)作为衡量标准,P<0.05为差异有统计学意义。
2 结 果
Pubmed中检索了525篇文献,中国知网中检索了1229篇文献,除去与PTMC无关、不包含甲状腺手术方式及对应复发情况数据的文献,共筛选出28个研究,其中2个研究将甲状腺全叶切除术定义为甲状腺全叶切除术和近全叶切除术,有4个研究无复发事件发生,1个研究数据与入组的英文研究相同,均予以剔除后,最终纳入meta分析的共21个研究(表1)。文献发表时间从2002年到2016年,总样本量为7 592例。
表1 21个研究中PTMC患者手术方式和复发情况
Fig 1 Surgical operations and recurrence of PTMC in the 21 studies
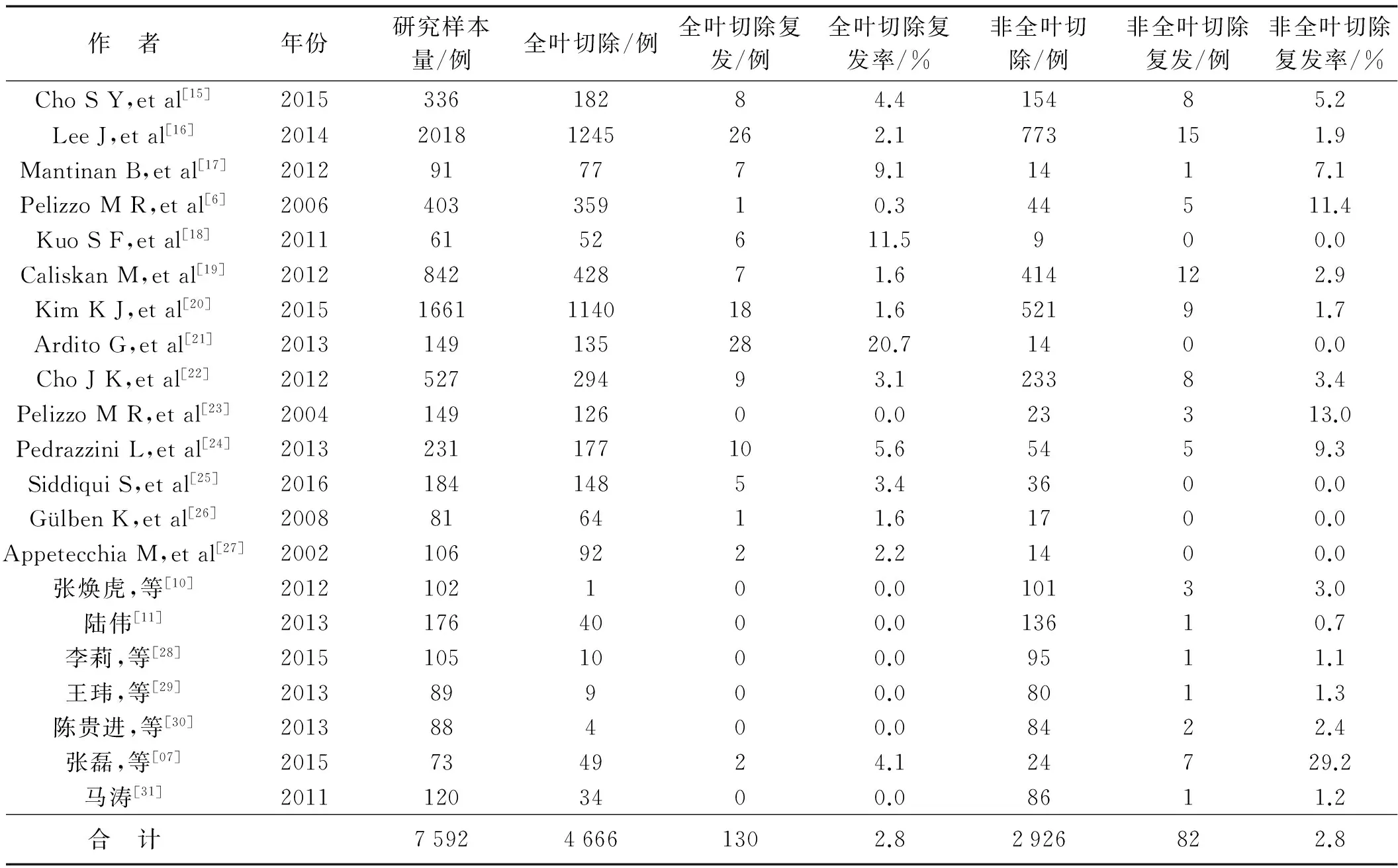
作 者年份研究样本量/例全叶切除/例全叶切除复发/例全叶切除复发率/%非全叶切除/例非全叶切除复发/例非全叶切除复发率/%ChoSY,etal[15]201533618284.415485.2LeeJ,etal[16]201420181245262.1773151.9MantinanB,etal[17]2012917779.11417.1PelizzoMR,etal[6]200640335910.344511.4KuoSF,etal[18]20116152611.5900.0CaliskanM,etal[19]201284242871.6414122.9KimKJ,etal[20]201516611140181.652191.7ArditoG,etal[21]20131491352820.71400.0ChoJK,etal[22]201252729493.123383.4PelizzoMR,etal[23]200414912600.023313.0PedrazziniL,etal[24]2013231177105.65459.3SiddiquiS,etal[25]201618414853.43600.0GülbenK,etal[26]2008816411.61700.0AppetecchiaM,etal[27]20021069222.21400.0张焕虎,等[10]2012102100.010133.0陆伟[11]20131764000.013610.7李莉,等[28]20151051000.09511.1王玮,等[29]201389900.08011.3陈贵进,等[30]201388400.08422.4张磊,等[07]2015734924.124729.2马涛[31]20111203400.08611.2合 计759246661302.82926822.8
对这21个研究进行固定效应模型研究,发现PTMC患者行甲状腺全叶切除术和甲状腺非全叶切除术术后复发差异无统计学意义(P=0.081,图1);同时对这些研究行发表偏倚Begg法检测,差异无统计学意义(Pr>|Z|=0.398,图2)。进而对行甲状腺非全叶切除术患者进行meta分析发现,行患侧甲状腺腺叶+峡部切除术组与行患侧甲状腺腺叶+对侧次全切除术组术后复发率分别为2.05%(4/195)和1.23%(1/81),差异无统计学意义(P>0.05,表2)。我们又研究了颈部淋巴结清扫与否对复发的影响,结果表明,行颈部淋巴结清扫组(中央区淋巴结清扫和或颈侧区淋巴结清扫)与不清扫组患者术后复发情况比较,差异有统计学意义(表2),行颈部淋巴结清扫术的患者更易复发;行中央区淋巴结清扫与不清扫组相比、行中央区淋巴结清扫与行中央区+颈侧区淋巴结清扫患者相比,差异均无统计学意义(表2)。

图1 甲状腺全叶切除术与非全叶切除术对复发影响的固定效应模型meta分析
Tab 1 Fixed-effects meta-analysis of recurrence between total thyroidectomy group and non-total thyroidectomy group for papillary thyroid microcarcinoma
表2 PTMC手术方式对复发影响的meta分析
Fig 2 Meta analysis of operation types and recurrence in patients with PTMC

手术方式研究个数OR值I2值95%CIP值患侧甲状腺腺叶+峡部切除组vs.患侧甲状腺腺叶+对侧次全切除组31.0650.0%0.201~5.6360.941颈部淋巴结清扫组vs.不清扫组35.22643.2%2.176~12.5490.000中央区淋巴结清扫组vs.不清扫组36.27967.7%0.321~122.9840.226中央区淋巴结清扫组vs.中央区+颈侧区淋巴结清扫组30.59282.6%0.005~76.2240.832

图2 甲状腺全叶切除术与非全叶切除术发表偏倚
Tab 2 Publication bias between total thyroidectomy group and non-total thyroidectomy group
3 讨 论
本研究结果显示:PTMC患者行颈部淋巴结清扫组比不行淋巴结清扫组术后更易复发;此外,行全叶切除术和非全叶切除术、患侧腺叶+峡部术和患侧腺叶+对侧次全切除术,术中行中央区淋巴结清扫术与未行淋巴结清扫、中央区淋巴结清扫术组与中央区淋巴结清扫术+颈侧区淋巴结清扫术之间比较,对术后复发的影响差异均无统计学意义。说明扩大PTMC的手术切除范围并不能降低复发事件的发生,甲状腺非全叶切除术也是不错的选择,而且还可减少术后并发症的发生[13]。虽然本研究显示行颈部淋巴结清扫组比不清扫组更易复发,但这并不能说明行颈部淋巴结清扫术没有意义,这看似矛盾的结果可能与以下因素有关:首先样本量较少,仅入组3个研究;其次有淋巴结转移患者相比于无淋巴结转移患者复发率高[32],有淋巴结转移是影响患者预后的独立因素[33],而入组的3个研究,行颈部淋巴结清扫者均是临床怀疑或者确诊有淋巴结转移,即这些行颈部淋巴结清扫的患者本身就容易复发;我们的研究结果提示,对于临床怀疑或者确诊淋巴结转移的患者,即使行颈部淋巴结清扫术,术后仍更易复发,这也间接反映出临床怀疑或确诊淋巴结转移的患者是复发的高危人群。因此,我们与Gschwandtner等[2]研究认知一致,主张对可疑淋巴结转移患者行淋巴结清扫术。
我们的研究还有很多缺陷。首先由于原始资料的缺乏,不能就甲状腺全叶切除对术后复发影响进行分层分析,只能对各种手术方式进行单因素分析,而单因素分析仅针对此21项研究,可能不具有普遍性和科学性。其次入组资料是回顾性研究,有其固有的缺陷比如选择偏倚、不精确或缺失数据。最后我们主要研究了甲状腺全叶切除与术后复发的关系,关于具体的手术方式如甲状腺全叶切除、甲状腺近全叶切除、甲状腺双叶次全叶切除、单纯甲状腺腺叶切除等手术方式对复发影响的研究还未涉及,所以,仍需要更多的探索。
[1] HAUGEN B R,ALEXANDER E K,BIBLE K C,et al.2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer:The American Thyroid Association Guidelines Task Force on Thyroid Nodulesand Differentiated Thyroid Cancer[J].Thyroid,2016,26(1):1-133.
[2] GSCHWANDTNER E,KLATTE T,SWIETEK N,et al.Increase of papillary thyroid microcarcinoma and a plea for restrictive treatment: A retrospective study of 1,391 prospective documented patients[J].Surg,2015,159(2):503-511.
[3] YU X M,WAN Y,SIPPEL R S,et al.Should all papillary thyroid microcarcinomas be aggressively treated:An analysis of 18,445 cases[J].Ann Surg,2011,254(4):653-660
[4] LANG B H,CHAN D T,WONG K P,et al.Predictive factors and pattern of locoregional recurrence after prophylactic central neck dissection in papillary thyroid carcinoma[J].Ann Surg Oncol,2014,21(13):4181-4187.
[5] ARDITO G,AVENIA N,GIUSTOZZI E,et al.Papillary thyroid microcarcinoma: proposal of treatment based on histological prognostic factors evaluation[J].Ann Ital Chir,2014,85(85):1-5.
[6] PELIZZO M R,BOSCHIN I M,TONIATO A,et al.Papillary thyroid microcarcinoma (PTMC): Prognostic factors,management and outcome in 403 patients[J].Eur J Surg Oncol,2006,32(10):1144-1148.
[7] 张磊,赵中美.甲状腺微小乳头状癌的手术治疗及预后分析[J].中国现代普通外科进展,2015,18(12):993-994.
[8] CREACH K M,SIEGEL B A,NUSSENBAUM B,et al.Radioactive iodine therapy decreases recurrence in thyroid papillary microcarcinoma[J].ISRN Endocrinol,2012,2012:816386-816391.
[9] WANG T S,GOFFREDO P,SOSA J A,et al.Papillary thyroid microcarcinoma:an over-treated malignancy [J].World J Surg,2014,38(9):2297-2303.
[10] 张焕虎,苏超,周海蒙,等.102例甲状腺微小乳头状癌的诊治分析[J].中国肿瘤临床,2012,39(1):49-51.
[11] 陆伟.甲状腺微小乳头状癌手术方式探讨(附176例临床分析)[J].浙江中医药大学学报,2013(10):1204-1205.
[12] LEE J,PARK J H,LEE C R,et al.Long-term outcomes of total thyroidectomy versus thyroid lobectomy for papillary thyroid microcarcinoma:comparative analysis after propensity score matching[J].Thyroid,2013,23(11):1408-1415.
[13] DONATINI G,CASTAGNET M,DESURMONT T,et al.Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated?[J].World J Surg,2016,40(3):510-515.
[14] ITO Y,MIYAUCHI A,KIHARA M,et al.Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation[J].Thyroid,2014,24(1):27-34.
[15] CHO S Y,LEE T H,KU Y H,et al.Central lymph node metastasis in papillary thyroid microcarcinoma can be stratified according to the number,the size of metastatic foci,and the presence of desmoplasia[J].Surg,2015,157(1):111-118.
[16] LEE J,SONG Y,SOH E Y.Central lymph node metastasis is an important prognostic factor in patients with papillary thyroid microcarcinoma[J].J Korean Med Sci,2014,29(1):48-52.
[17] MANTINAN B,REGO-IRAETA A,LARRAAGA A,et al.Factors influencing the outcome of patients with incidental papillary thyroid microcarcinoma[J].J Thyroid Res,2012,2012:469397-469401
[18] KUO S F,CHAO T C,CHANG H Y,et al.Prognostic evaluation of patients with multicentric papillary thyroid microcarcinoma[J].J Formos Med Assoc,2011,110(8):511-517.
[19] CALISKAN M,PARK J H,JEONG J S,et al.Role of prophylactic ipsilateral central compartment lymph node dissection in papillary thyroid microcarcinoma[J].Endocr J,2012,59(4):305-311.
[20] KIM K J,KIM S M,LEE Y S,et al.Prognostic significance of tumor multifocality in papillary thyroid carcinoma and its relationship with primary tumor size: a retrospective study of 2,309 consecutive patients[J].Ann Surg Oncol,2015,22(1):125-131.
[21] ARDITO G,REVELLI L,GIUSTOZZI E,et al.Aggressive papillary thyroid microcarcinoma: prognostic factors and therapeutic strategy[J].Clin Nucl Med,2013,38(1):25-28.
[22] CHO JK,KIM J Y,JEONG C Y,et al.Clinical features and prognostic factors in papillary thyroid microcarcinoma depends
on age[J].J Korean Surg Soc,2012,82(5):281-287.
[23] PELIZZO M R,BOSCHIN I M,TONIATO A,et al.Natural history,diagnosis,treatment and outcome of papillary thyroid microcarcinoma (PTMC): a mono-institutional 12-year experience[J].Nucl Med Commun,2004,25(6):547-552.
[24] PEDRAZZINI L,BAROLI A,MARZOLI L,et al.Cancer recurrence in papillary thyroid microcarcinoma: a multivariate analysis on 231 patients with a 12-year follow-up[J].Minerva Endocrinol,2013,38(3):269-279.
[25] SIDDIQUI S,WHITE M G,ANTIC T,et al.Clinical and pathologic predictors of lymph node metastasis and recurrence in papillary thyroid microcarcinoma[J].Thyroid,2016,26(6):807-815.

[27] APPETECCHIA M,SCARCELLO G,PUCCI E,et al.Outcome after treatment of papillary thyroid microcarcinoma[J].J Exp Clin Cancer Res,2002,21(2):159-164.
[28] 李莉,刘晖,高卫峰,等.甲状腺微小乳头状癌105例诊治分析[J].中国城乡企业卫生,2015(1):86-87.
[29] 王玮,张静潭,宋永蔚,等.甲状腺微小乳头状癌89例诊治体会[J].中国临床研究,2013,26(3):248-249.
[30] 陈贵进,王春喜,李胜君.88例甲状腺微小乳头状癌诊治分析[J].军医进修学院学报,2013(5):449-451.
[31] 马涛.PTMC行中央区淋巴结清扫的临床应用研究[D].银川:宁夏医科大学,2011.
[32] BESIC N,ZGAJNAR J,HOCEVAR M,et al.Extent of thyroidectomy and lymphadenectomy in 254 patients with papillary thyroid microcarcinoma:a single-institution experience[J].Ann Surg Oncol,2009,16(4):920-928.
[33] USLUOGULLAR C A,ONAL E D,OZDEMIR E,et al.A retrospective analysis of prognostic factors predictive of lymph node metastasis and recurrence in thyroid papillary microcarcinoma[J].Minerva Endocrinol,2015,40(1):15-22.
Recurrence effect of differert surgical operations types on papillary thyroid microcarcinoma: a meta-analysis
YI Dan-dan1,HUANG Tao1,SONG Peng2,SANG Jian-feng2
(1.DepartmentofGeneralSurgery,DrumTowerClinicalMedicalCollege,NanjingMedicalUniversity,Nanjing210008,China;2.DepartmentofGeneralSurgery,DrumTowerHospitalofNanjing,AffiliatedtoNanjingUniversityMedicalSchool,Nanjing210008,China)
Objective:To evaluate the recurrence effect of different surgical operation types on papillary thyroid microcarcinoma.Method:Relevant studies concerning operation types and recurrence in PubMed and National Knowledge Infrastructure(CNKI) were retrieved.Meta-analysis was performed by Stata 12.0 software.Results:There was no difference of recurrence between total thyroidectomy group and non-total thyroidectomy group,but those with cervical lymph node dissection were more likely to recur than those who didn′t.Conclusion:Non-total thyroidectomy may be a good choice for papillary thyroid microcarcinoma.
papillary thyroid microcarcinoma;recurrence;meta-analysis
2016-08-01
2016-08-26
南京市医学科技发展项目(YKK15082)
伊丹丹(1991-),女,江苏徐州人,在读硕士研究生。E-mail:yidandan133@126.com
桑剑锋 E-mail: drsangjianfeng@163.com
伊丹丹,黄韬,宋鹏,等.甲状腺微小乳头状癌手术方式对肿瘤复发影响的meta分析[J].东南大学学报:医学版,2017,36(1):48-52.
R653
A
1671-6264(2017)01-0048-05
10.3969/j.issn.1671-6264.2017.01.012
