心血管整体评分评估胎儿心功能不全的价值
2016-11-12武超王玲红刘丽萍
武超,王玲红,刘丽萍
心血管整体评分评估胎儿心功能不全的价值
武超,王玲红,刘丽萍
目的:探讨心血管整体评分(CVPS)对胎儿心功能不全评估的价值。方法:对2013年1月—2016年1月来天津市中心妇产科医院超声中心就诊的孕妇行常规超声检查,检出其中有心功能异常表现(心脏增大、心肌收缩乏力)的胎儿,记录CVPS评分结果,同时行胎儿超声心动图检查,确定有无心内结构异常。依据追访结果,将病例分为2组:活产组和不良妊娠结局组。结果:共检出心功能不全胎儿38例,其中单胎35例,双胎3例。活产组12例,均为单胎,出生后体健10例,2例合并先心病:1例肺动脉瓣轻度狭窄,1例法乐四联症。不良妊娠结局组21例。单胎不良妊娠结局共18例,其中宫内死胎9例,死产2例,引产7例:CVPS持续降低心功能逐渐恶化直至心力衰竭5例,合并难治型先心病2例。双胎中2例为双胎输血综合征(TTTS)宫内死胎,1例为胎儿脑积水、颅内出血引产。失访5例。活产组胎儿CVPS的中位数(四分位数间距)[M(Q)]为7.62(7.00),不良妊娠结局组胎儿CVPS的M(Q)为5.67(3.50)。受试者工作特征(ROC)曲线分析,曲线下面积(AUC)0.823,Cut-off值为6.5,P=0.002,有统计学意义。活产组胎儿脐动脉频谱评分、静脉频谱评分和心脏瓣膜功能评分均高于不良妊娠结局组,差异有统计学意义(均P<0.05)。结论:随着胎儿心功能不全加重直至心力衰竭,CVPS逐渐降低,CVPS危险临界值为6.5,CVPS是连续动态评估胎儿心功能不全的有效指标。胎儿脐动脉频谱、静脉频谱及心脏瓣膜功能评分对预测不良妊娠结局具有一定价值。
超声检查,产前;超声检查,多普勒,彩色;胎儿心脏;心脏缺损,先天性;心血管整体评分
(J Int Obstet Gynecol,2016,43:315-317)
胎儿心功能不全占产前超声检查妊娠妇女总数的0.17%,占高危妊娠患者的2%[1],胎儿心功能不全是高危妊娠胎儿宫内死亡的重要原因之一,胎儿心力衰竭的常见原因有胎儿心律失常、贫血、先天性心脏病伴瓣膜返流、心外畸形(如先天性膈疝、畸胎瘤等)、胎儿系统性感染、双胎输血综合征(twin-to-twin transfusion syndrome,TTTS)中受血者的血容量及血压超负荷[2-3]。准确评估胎儿心脏功能对早期作出正确临床诊断、预测妊娠结局有很大帮助。心血管整体评分(cardiovascular profile score,CVPS)是胎儿心功能不全半定量评价指标,由胎儿水肿、心胸(C/T)比值、心脏瓣膜功能、脐静脉和静脉导管血流频谱(Doppler)以及脐动脉血流频谱组成。
1 对象与方法
1.1 研究对象2013年1月—2016年1月来天津市中心妇产科医院超声科常规超声检查的孕妇检出其中胎儿有心功能异常表现(心肌收缩乏力、心脏增大)者,行CVPS,记录评分值。同时行胎儿超声心动检查,以确定有无合并胎儿心内结构异常,同时记录胎儿心外结构异常。
1.2 仪器与方法应用GE voluson 730 EXPERT、E8全数字实时彩色超声诊断仪,经腹3.5~5.0 MHz探头,在胎儿矢状切面或横断面等多切面扫查,观察所有心功能异常的胎儿水肿、C/T比值、心脏瓣膜功能、脐静脉和静脉导管血流频谱以及脐动脉血流频谱。CVPS评分表,见表1,每个项目2分,总分10分。
将5项评分相加得到CVPS评分值。对所有心功能异常胎儿行超声心动检查,以确定有无胎儿心内结构异常。同时记录胎儿常规超声检查所发现的心外结构异常。CVPS持续降低心功能恶化直至心力衰竭的胎儿以及合并严重难治型心内、心外异常的胎儿,在胎儿家属充分知情同意并经医学伦理学委员会讨论通过基础上引产。根据追访结果,将病例分为2组:活产组和不良妊娠结局组。其中不良妊娠结局组包括死胎、死产、引产。
1.3 统计学方法应用SPSS 20.0软件进行统计分析,定量资料呈正态分布的数据用均数±标准差(±s)表示;非正态分布的数据用中位数(M)和四分位数间距(Q)表示,组间比较采用秩和检验;CVPS评分表效能检验采用非参数检验的受试者工作特征(ROC)曲线分析,P<0.05为差异有统计学意义。
2 结果
2.1 CVPS的ROC曲线分析共检出心功能不全胎儿38例,孕妇年龄22~40岁,平均(28.27±4.81)岁,孕18~40周。其中单胎35例,双胎3例。足月活产12例,均为单胎,出生后体健10例,2例合并先天性心脏病:1例肺动脉瓣轻度狭窄,1例法乐四联症,出生后手术治疗。单胎不良妊娠结局共18例:其中宫内死胎9例;死产2例;引产共7例(5例连续监测CVPS持续降低,心功能逐渐恶化直至心力衰竭,CVPS评分由最高7分降至最低2分,平均下降3.8分;2例合并先天性心脏病重度肺动脉狭窄、右心发育不良综合征)。双胎中2例为TTTS宫内死胎,1例为胎儿脑积水、颅内出血引产。失访5例。根据追访结果,将病例分为2组:活产组(12例)和不良妊娠结局组(21例)。活产组胎儿的CVPS为7.62 (7.00),不良妊娠结局组胎儿的CVPS为5.67 (3.50)。ROC曲线分析,曲线下面积(AUC)0.823,见图1,活产组与不良妊娠结局组之间Cut-off值为6.5,P=0.002,差异有统计学意义。敏感度:61.9%,特异度:91.7%。

图1 CVPS的ROC曲线分析
2.2 不良妊娠结局发生率本研究中出现脐动脉D波达基线6例、舒张期频谱反向2例均为死胎,不良妊娠结局发生率100%。出现胎儿脐静脉搏动共6例,1例复查时脐静脉搏动消失后足月活产出生后体健、4例死胎、1例TTTS宫内死胎引产,不良妊娠结局发生率83.3%。静脉导管a波反向者共11例,6例死胎,2例合并重度肺动脉狭窄、右心发育不良综合征引产,1例CVPS持续降低心功能恶化引产,1例合并肺动脉瓣重度狭窄死产,1例足月活产出生后体健,不良妊娠结局发生率90.9%。胎儿皮肤水肿3例,2例为死胎,1为双胎TTTS之一宫内死胎引产,不良妊娠结局发生率100%。胎儿心脏瓣膜功能异常(出现二尖瓣返流及心室单向充盈者)共6例,其中死胎5例、死产1例,不良妊娠结局发生率100%。
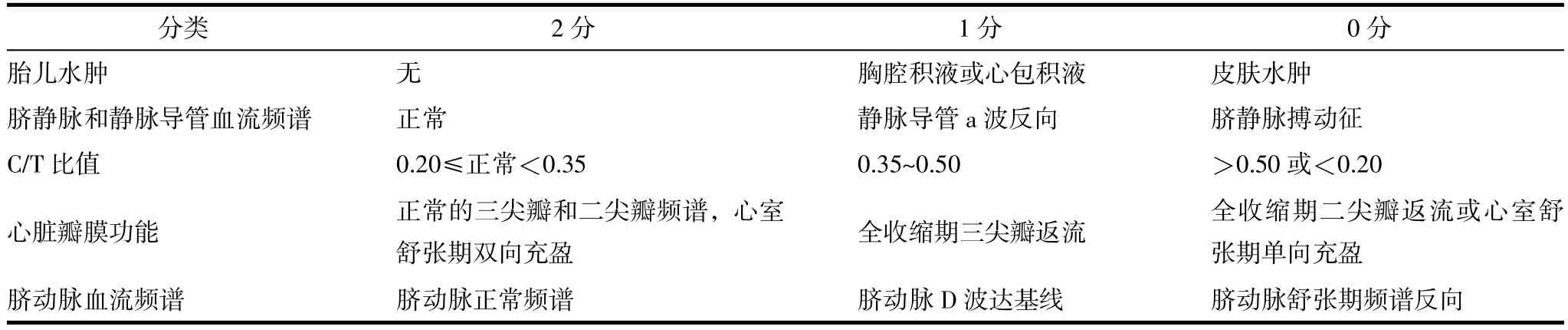
表1 CVPS评分表[4]
2.32 组CVPS评分值比较2组胎儿孕周、C/T比值评分和胎儿水肿评分比较差异无统计学意义(均P>0.05);胎儿脐动脉频谱评分、静脉频谱(包括静脉导管和脐静脉)评分和心脏瓣膜功能评分活产组均高于不良妊娠结局组,差异有统计学意义(均P<0.05),见表2。
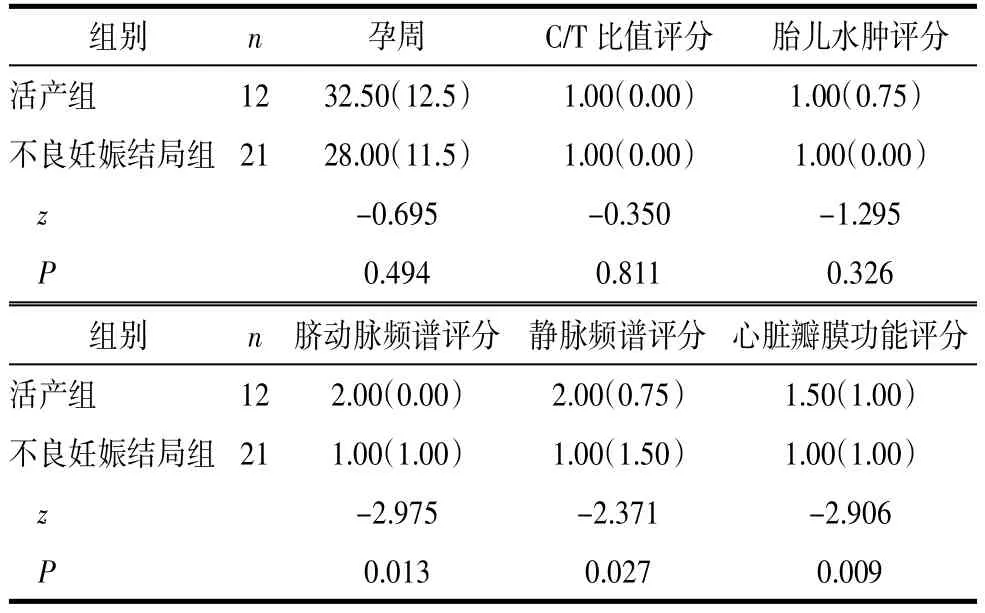
表2 2组孕周及CVPS评分值比较M(Q)
3 讨论
随着计算机和超声心动图技术的发展,胎儿心功能评价方法不断推陈出新。目前应用较多的主要包括通过M型超声心动图计算心室缩短分数(FS)、Tei指数,应用时间-空间相关成像技术(STIC)计算心室舒张末、收缩末容积从而计算出心功能相关数值等,但各种方法的参考值差别很大,有些测量耗时长、可重复性差,有些受孕周及胎儿心律影响,在孕周小、心律不齐时获得数据困难。在对胎儿心功能进行评定时往往有偏差,因此还不能单一用某个指标进行准确判断。CVPS是较为完善的胎儿心功能不全半定量评价指标,国外已有相关研究证明其是连续评价胎儿心功能的有效工具,低CVPS与胎儿不良妊娠结局相关,且此方法具有更容易操作、获得数据可靠等特点[5]。文献报道CVPS一旦降低提示胎儿心功能受损,应当给予干预,CVPS≤7分,应给予针对病因学的治疗[3-4,6-7]。本研究表明胎儿心功能恶化直至心力衰竭,CVPS持续降低。胎儿CVPS危险临界值为6.5。不良妊娠结局组胎儿静脉频谱评分、脐动脉频谱评分和心脏瓣膜功能低于活产组,对预测不良妊娠结局具有一定价值,与文献报道一致[4]。由于本研究中皮肤水肿仅出现3例,故此因素与不良妊娠结局的相关性尚待积累病例进一步总结。
目前CVPS对小孕周胎儿心功能不全的评估尚无定论[8]。本研究中胎儿心功能不全出现最早时间为孕18周,对中孕早期(早于孕18周)的病例CVPS的诊断价值尚需继续积累病例。综上所述,CVPS可以全面、动态评估胎儿心功能不全的持续时间、严重程度,为临床早期诊断、动态监测、结局预测提供可靠依据。
[1]陈欣林,陈常佩,易志环.应用彩色多普勒超声产前诊断胎儿心功能不全的研究[J].中华妇产科杂志,2000,35(8):470-472.
[2]Huhta JC.Guidelines for the evaluation of heart failure in the fetus with or without hydrops[J].Pediatr Cardiol,2004,25(3):274-286.
[3]Ojala TH,Hornberger LK.Fetal heart failure[J].Front Biosci(Schol Ed),2010,2:891-906.
[4]Huhta JC.Fetal congestive heart failure[J].Semin Fetal Neonatal Med,2005,10(6):542-552.
[5]Statile CJ,Cnota JF,Gomien S,et al.Estimated cardiac output and cardiovascular profile score in fetuses with high cardiac output lesions[J].Ultrasound Obstet Gynecol,2013,41(1):54-58.
[6]McElhinney DB,Tworetzky W,Lock JE.Current status of fetal cardiac intervention[J].Circulation,2010,121(10):1256-1263.
[7]Huhta J,Quintero RA,Suh E,et al.Advances in fetal cardiac intervention[J].Curr Opin Pediatr,2004,16(5):487-493.
[8]周开宇,李一飞,谢亮,等.经胎盘转运地高辛治疗胎儿心力衰竭的非随机对照研究[J].中国循证儿科杂志,2013,8(1):15-21.
The Value of Cardiovascular Profile Score to Assess Fetal Cardiac Insufficiency
WU Chao,WANG Ling-hong,LIU Li-ping.Department of Ultrasound,Tianjin Central Hospital of Gynecology Obstetrics,Tianjin 300100,China
Objective:To explore the value of cadiovascular profile score(CVPS)to estimate fetal cadiac insufficiency. Methods:All pregnant women in ultrasound department,Tianjin Central Hospital of Gynecology Obstetrics proceeded routine examinations between Jan.2013 and Jan.2016.Fetal cardiac insufficiency(enlarged heart and myocardial contraction fatigue)were found out.CVPS were recorded.Meanwhile fetal cadiography were performed to define if congenital heart disease were accompanied.All cases divided in two groups based on the follow up results:live birth group and adverse pregnancy outcome group.Results:38 cases of fetal cardiac insufficiency were found out.35 cases were singleton pregnancy.3 cases were twins pregnancy.12 cases were in live birth group(all of them were singleton pregnancy),10 cases were healthy children,2 cases were accompanied by congenital heart disease:1 case was mild pulmonicstenosis,1 case was tetralogy of Fallot.21 cases were in adverse pregnancy outcome group.18 cases were singleton pregnancies:9 cases were intrauterine fetal demise,2 cases were stillbirth,7 cases were induced labour:5 cases progressed to heart failure because of CVPS declined continuously and fetal cadiac insufficiency worsen,2 cases were accompanied by fatal congenital heart disease.2 cases of twins pregnancy were intrauterine fetal demise because of twin to twin transfusion syndrome(TTTS).1 case of twins pregnancy was induced labour because of hydrocephaly and intracranial hemorrhage.5 cases were loss to follow up.CVPS of live birth was 7.62(7.00)and CVPS of adverse pregnancy outcomes was 5.67(3.50).Statistics analysis:ROC curve analysis,area under ROC:0.823,cut off value was 6.5,P=0.002,difference was statistically significant.The score of umbilical artery doppler spectrum,vein doppler spectrum and cardiac valve function in two groups were significant difference(P<0.05).Conclusions:CVPS declined when fetal cardiac insufficiency worse,dangerous cut off value of CVPS was 6.5,CVPS is an effective index for continuous dynamic assessment of fetal cardiac insufficiency.The score of umbilical artery doppler spectrum,vein doppler spectrum and cardiac valve function were valuable to predict adverse pregnancy outcomes.
Ultrasonography,prenatal;Ultrasonography,Doppler,color;Fetal heart;Heart defects,congenital;Cadivascular profile score
2016-04-29)
[本文编辑 王琳]
妇科肿瘤研究
300100天津市中心妇产科医院超声科
