激素辅助治疗对隐睾儿童睾丸生精功能影响的系统评价和Meta分析
2015-05-04付生军
张 驌 王 诚 付生军 杨 立
·论著·
激素辅助治疗对隐睾儿童睾丸生精功能影响的系统评价和Meta分析
张 驌 王 诚 付生军 杨 立
目的 评价激素辅助治疗对于隐睾儿童睾丸生精功能的影响。方法 计算机检索PubMed、EMBASE、The Cochrane Library、中国生物医学文献数据库、中国知网、万方数据库和维普数据库,获得激素对隐睾儿童睾丸生精功能影响的干预性研究,检索时限均从建库至2015年9月30日。由2名研究者独立行文献筛选、资料提取,并评价纳入研究的偏倚风险。以睾丸固定术中睾丸活检每曲细精管横断面精原细胞数(S/T)为近期指标,以均数差(MD)及其95%CI作为效应指标;以成年后患者精子密度正常比例为远期指标,以相对危险度(RR)及其95%CI作为效应指标。采用RevMan 5.3软件行Meta分析,根据异质性检验结果选择相应的效应模型合并效应量。结果 8篇文献进入Meta分析,4篇为RCT,4篇为NRCT。8篇文献的偏倚风险均较大。3篇文献报道了绒毛膜促性腺激素(hCG)+手术和单纯手术睾丸活检S/T水平,文献间具同质性,Meta分析结果显示,hCG+手术S/T水平显著低于单纯手术, MD=-0.08,95%CI:-0.13~-0.03,P=0.002。4篇文献汇总的随机效应模型Meta分析结果显示,促黄体生成素释放激素(LHRH)+手术S/T显著高于单纯手术,差异有统计学意义,MD=0.34,95%CI:0.04~0.64,P=0.03;按部位行亚组分析显示,单侧或双侧隐睾LHRH+手术均较单纯手术S/T显著增加。2篇文献汇总的随机效应模型Meta分析结果显示, hCG+LHRH+手术与单纯手术比较,成年后精子密度正常比例差异无统计学意义,RR=1.46,95%CI:0.24~9.06,P=0.68。 结论 hCG辅助治疗对短期睾丸生精功能有损伤;LHRH辅助治疗可改善短期睾丸生精功能;而hCG+LHRH对于远期生精功能无显著影响。考虑纳入文献数量较少且偏倚风险高,仍有待更多的研究。
隐睾; 绒毛膜促性腺激素; 促黄体生成素释放激素; 生精功能; Meta分析 系统评价
隐睾病因尚不清楚,其远期预后主要包括生育能力和睾丸恶变,故早期如何进行有效的治疗是临床关注的热点。有研究显示隐睾手术治疗成功率约为70%,且并发症少,而激素辅助治疗的成功率约为20%,且不良事件发生率较高[1, 2]。2014年美国泌尿外科指南推荐首选手术治疗隐睾,不推荐激素治疗,主要考虑激素治疗的睾丸下降率低,且有较多不良反应,尤其可引起精原细胞损伤[3]。北欧国家也不建议激素治疗,推荐在6~12月龄行手术干预[4]。但早期手术干预并未明显改善生育能力及睾丸恶变率[5]。激素辅助治疗包括睾丸固定术前或术后应用绒毛膜促性腺激素(hCG)或促黄体激素释放激素(LHRH)。研究显示hCG可增加睾丸体积,促进睾丸血供,舒张提睾肌;但有研究显示hCG可损害睾丸组织[6,7]。近期有前瞻性研究显示LHRH辅助治疗可促进睾丸发育及生精功能,如增加睾丸活检每曲细精管横断面精原细胞数(S/T),且不良反应小[8, 9]。而S/T与成年后生育能力呈显著正相关[10]。2014版的欧洲泌尿外科指南并不反对激素辅助治疗,并指出现有对于激素治疗隐睾的反对意见主要来自hCG可能损伤睾丸生精功能的相关研究,并非针对LHRH。为此本研究检索相关文献,对不同激素辅助疗法对隐睾患儿睾丸生精功能影响行定量评价,以期为激素辅助治疗隐睾提供依据。
1 方法
1.1 文献纳入标准 ①干预类研究,包括RCT和NRCT;②单侧及双侧隐睾,种族不限;③干预措施为激素(单用hCG、单用LHRH、hCG+LHRH)加手术治疗,对照为单纯手术治疗;④报道了本文设定的结局指标。
1.2 文献排除标准 ①回缩性隐睾;②合并疝气;③二次手术者;④睾丸缺如;⑤两性畸形或其他染色体疾病;⑥重复发表的文献;⑦原始研究结局数据报告不全,与作者联系后无法获得所需数据的文献。
1.3 结局指标 近期指标 :睾丸固定术中睾丸活检S/T。远期指标:成年后精子密度正常比例,参考WHO第4版《人类精液和精子-宫颈黏液相互作用实验室检验手册》,正常值>20×106·mL-1。
1.4 文献检索策略 计算机检索PubMed、EMBASE、The Cochrane Library、中国生物医学文献数据库、中国知网、万方数据库和维普数据库,检索时限均从建库至2015年9月30日。
英文检索词:Cryptorchidism、Undescended testis、Gonadotropin releasing hormone、Luteinizing hormone-releasing hormone、GnRH、LHRH、Chorionic gonadotropin、Human chorionic gonadotropin、hCG。
以PubMed数据库为例,其具体检索策略如下。
#1 "Cryptorchidism"[MeSH Terms] OR "Undescended testis"[Title/Abstract] OR "Undescended testes"[Title/Abstract] OR Cryptorchidism[Title/Abstract] OR Cryptorchism[Title/Abstract]
#2 "Gonadotropin-releasing hormone"[MeSH Terms] OR "Gonadotropin releasing hormone"[Title/Abstract] OR GnRH[Title/Abstract]) OR Buserelin[Title/Abstract]) OR LHRH[Title/Abstract] OR Gonadotropin-releasing hormone[Title/Abstract]
#3 "Chorionic gonadotropin"[MeSH Terms] OR Choriogonadotropin[Title/Abstract]) OR Choriogonin[Title/Abstract] OR Pregnyl[Title/Abstract] OR Chorulon[Title/Abstract] OR Gonabion[Title/Abstract] OR "Human chorionic gonadotropin"[Title/Abstract] OR "Chorionic gonadotropin, Human"[Title/Abstract]) OR HCG[Title/Abstract]) OR hCG[Title/Abstract] OR "Chorionic gonadotropin"[Title/Abstract]
#4 #1 AND ( #2 OR #3)
中文检索词:隐睾、未下降睾丸、HCG、激素、LHRH、促性腺激素释放激素、人绒毛膜促性腺激、GnRH、促黄体激素释放激素。
1.5 文献筛选、资料提取和偏倚风险评价 由张驌与王诚独立进行,并交叉核对,如遇分歧,由付生军裁决。提取资料包括:①文献基本信息,第一作者、发表年份和国家;②研究对象基本特征:激素种类及用法、各组病例数、患者年龄和手术年龄;③RCT或NRCT及其偏倚风险评价内容;④结局指标。RCT文献的偏倚风险采用Cochrane系统评价员手册推荐的6条标准评价,以是、否和不清楚表示;NRCT的偏倚风险采用MINORS量表(Methodological index for non-randomized studies)评价,共包含12个条目。每个条目未报道赋0分,有报道但信息不充分赋1分,有报道且信息充分赋2分。
1.6 统计学方法 采用RevMan 5.3软件行Meta分析。计数资料以相对危险度(RR)、计量资料以均数差(MD)及其95%CI作为效应指标。 首先采用χ2检验行各研究结果间的异质性分析,若各文献间P>0.1,I2<50%,采用固定效应模型合并结果;若各文献间P<0.1,I2>50%,则进一步分析异质性来源,在排除明显临床异质性的影响后,采用随机效应模型行Meta分析。若各研究间存在明显临床异质性,采用亚组分析或敏感性分析。P<0.05 为差异有统计学意义。
2 结果
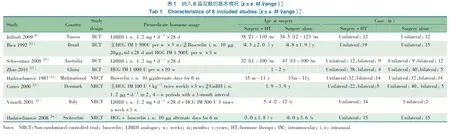
2.1 文献检索结果 初步检索共获得相关文献1 988篇, 8篇文献[9,11~17]进入Meta分析(图1),4篇RCT(n=187),4篇NRCT (n=248)。纳入文献的基本特征如表1所示。
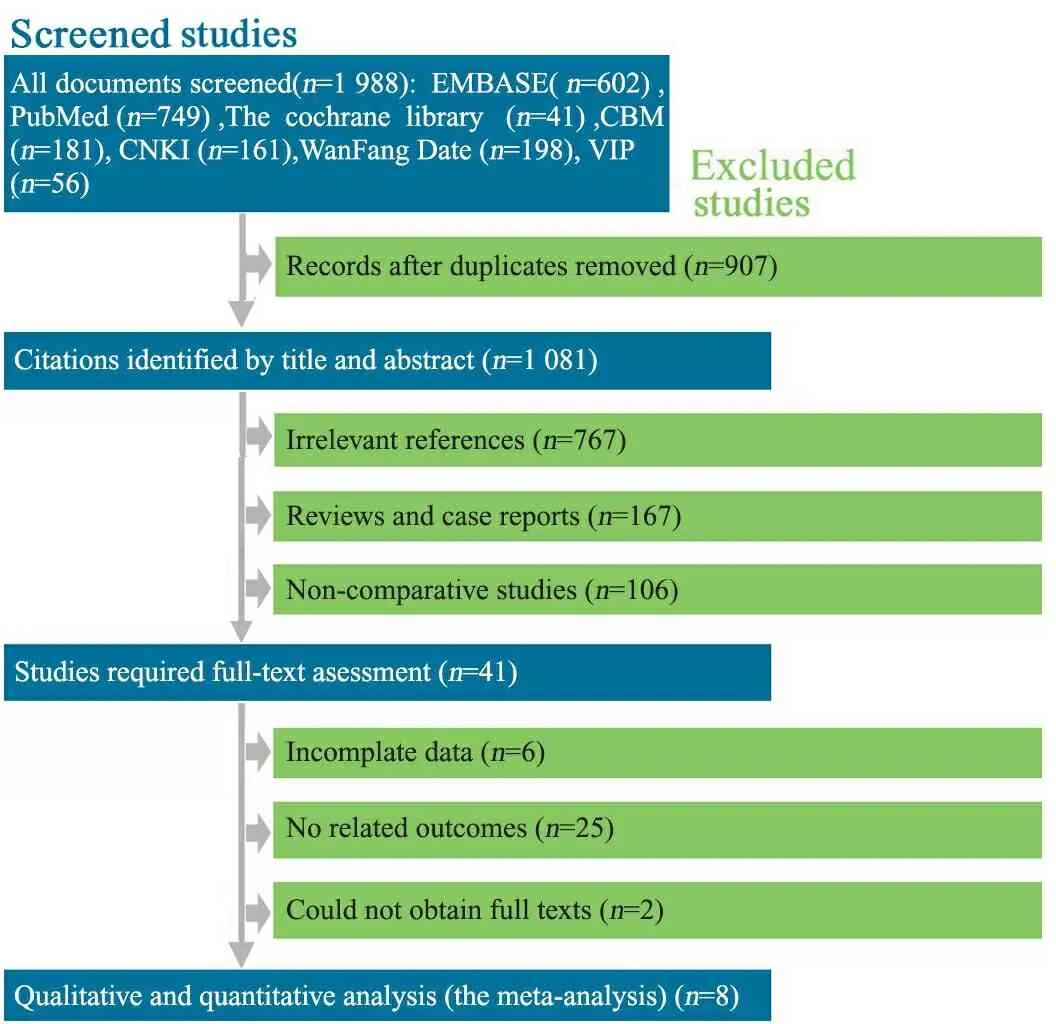
图1 文献筛选流程图
Fig 1 Flow chart of aricle screening and selection process
2.2 偏倚风险评价 4篇RCT文献[9,12,15,17]随机序列的产生和分配隐藏均不清楚,均未对受试者和研究者施盲,对结局测量均采用盲法,均未选择性报告研究结果,结果数据均具完整性,其他偏倚来源为不清楚。4篇NRCT文献[11,13,14,16]均报道了研究目的、数据收集、终点指标的选择与评价、失访率、对照组的选择、组间基线可比性与统计分析,且信息充分;文献[11,13]报道了纳入病例的连续性,但信息不充分,文献[14,16]未报道;文献[11,13]报道了随访时间且信息充分,文献[14,16]未报道;文献[11]报道了对照组与试验组同期进行的同步性且信息充分,文献[13]提供的信息不充分,文献[14,16]未报道;4篇文献均未报道样本量的估算。文献[11]评为20分,文献[13,14,16]评为18分。
2.3 Meta分析结果
2.3.1 睾丸活检S/T 3篇文献比较了hCG+手术和单纯手术的睾丸活检S/T,共纳入175例患儿。文献间具同质性,固定效应模型Meta分析显示: hCG+手术的S/T低于单纯手术,差异有统计学意义,MD=-0.08,95%CI:-0.13~-0.03,P=0.002(图2)。
4篇文献比较了LHRH+手术和单纯手术的睾丸活检S/T,共纳入344例患儿。异质性检验I2=83%,P<0.000 1,采用随机效应模型进行合并,Meta分析显示,LHRH+手术睾丸活检S/T高于单纯手术,差异有统计学意义,MD=0.34,95%CI:0.04~0.64,P=0.03。按部位行亚组分析,单侧隐睾:LHRH+手术较单纯手术S/T增加,MD=0.43,95%CI:0.21~0.65,P=0.000 2;双侧隐睾,LHRH+手术较单纯手术S/T增加,MD=0.43,95%CI:0.17~0.68,P=0.001(图3)。
2.3.2 正常精子密度比例 文献[14,16]文献报道了成年后精液分析正常精子密度比例,文献间P<0.000 1,I2=94%,随机效应模型Meta分析显示:hCG+LHRH+手术和单纯手术成年后正常精子密度比例差异无统计学意义,RR=1.46, 95%CI:0.24~9.06,P=0.68(图4)。
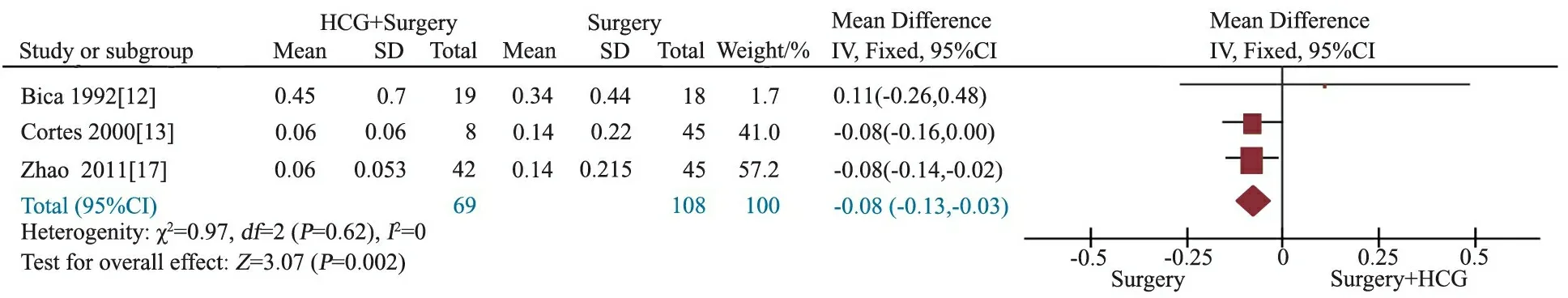
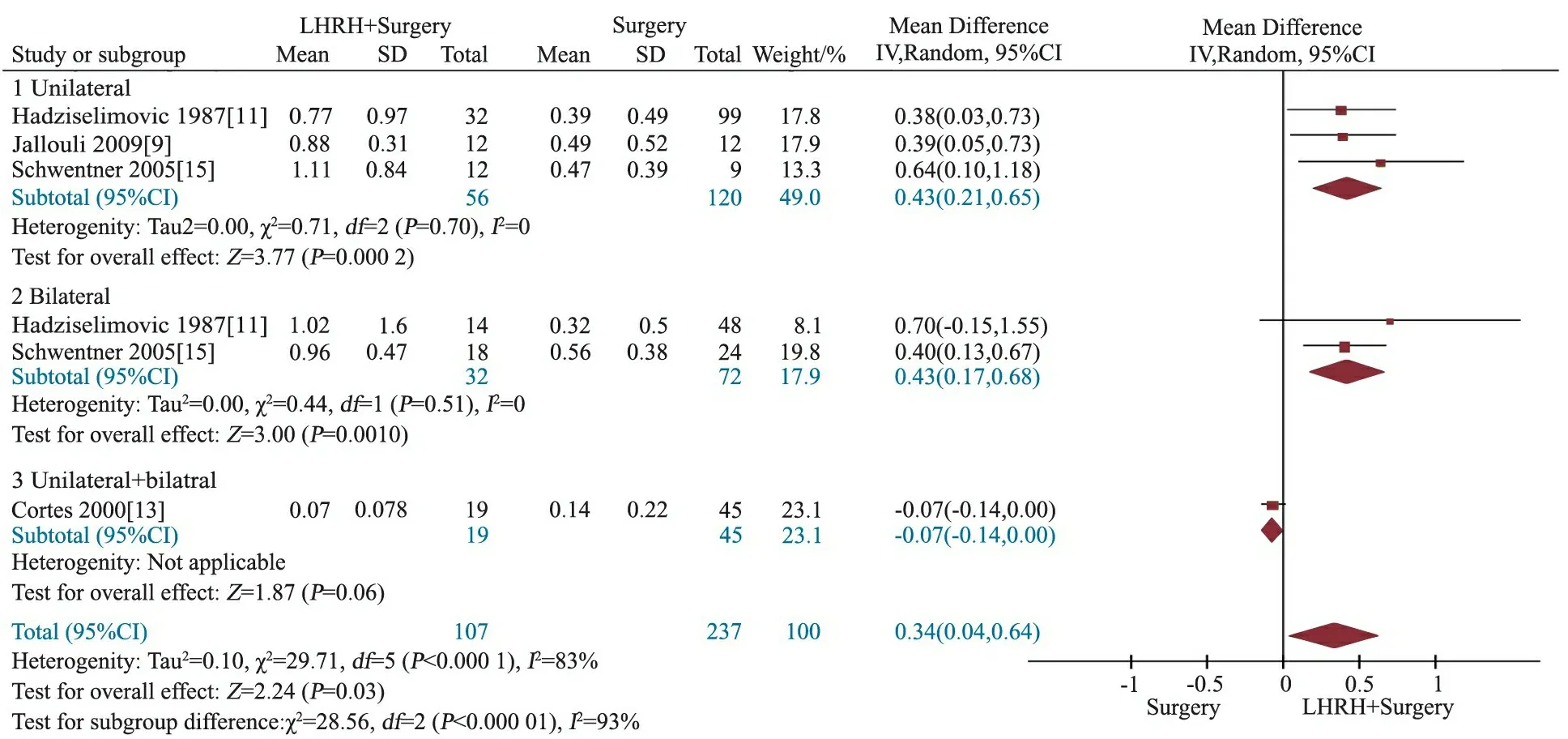
图2 HCG+手术和单纯手术睾丸活检S/T比较的Meta分析

图3 LHRH+手术和单纯手术睾丸活检S/T比较的Meta分析
图4 成年后精液分析正常精子密度比例的Meta分析
Fig 4 Meta-analysis of the rate of normal sperm concentration in adulthood
3 讨论
本系统评价共纳入8篇原始研究,其中包含4篇RCT与4篇NRCT。4篇RCT的随机序列产生和分配隐藏均不清楚,均未对受试者和研究者施盲,具有较高的偏倚风险;4篇NRCT文献MINORS得分在18~20分,虽无较高的偏倚风险,但对于干预性研究的论证强度较RCT低。本文Meta分析的证据强度较低。
hCG自从1930年应用于隐睾治疗,但治疗效果仍存在争议[18]。hCG治疗隐睾的理论基础是其可刺激睾丸间质细胞而增加睾酮的产生。hCG治疗隐睾有效率约25%[2]。术前应用hCG,可增加睾丸血流,减少术中睾丸缺血[19]。隐睾患儿予hCG治疗,成年后睾丸体积明显大于未用药组[6]。但hCG治疗可引起睾丸的相关损伤,可引起睾丸间质水肿、炎症反应、精原细胞凋亡、阴茎异常勃起以及远期抑制睾丸发育等[7, 13, 18, 20, 21]。本文Meta分析结果显示,hCG+手术组较单纯手术组S/T降低,提示hCG对睾丸生精功能造成了一定程度的损伤。
LHRH 及其类似物是下丘脑产生的促垂体分泌促黄体生成素的激素,可以增高血清中的促黄体生成激素水平,也可刺激睾丸间质细胞使局部产生高浓度睾酮,且无特殊不良反应,偶有阴茎异常勃起,但发生率明显低于hCG治疗组(5.1%vs74.1%)[18]。早期对照研究显示,对hCG治疗失败的患儿行睾丸固定术,术后辅助应用LHRH,成年后精液分析精子密度、活动力以及形态都明显优于早年单纯手术患儿[22]。近期RCT显示,睾丸固定术前和术后4周应用LHRH,随访5年,发现用药组睾丸体积明显大于未用药组[8]。本文Meta分析结果显示,LHRH+手术较单纯手术治疗,无论是单侧隐睾,抑或双侧隐睾,S/T均增高,提示对睾丸生精功能有促进作用。
本文Meta分析结果显示,与单纯手术相比,hCG+LHRH+手术未显著增加患者成年后正常精子密度比例。且文献[14] 与[16]分别显示精子活动力以及形态两组间也无差异。但无法鉴别是否hCG的应用降低了LHRH的促睾丸生精作用,还是两者对睾丸生精功能的影响只是短期效应,因有研究报道术前应用hCG,停药数周后行手术,未发现睾丸损伤[20,23]。
本研究的局限性:①纳入文献对于隐睾患儿手术治疗时间的把握不同,可能会对结局的评价带来影响;②各研究的药物用量及用法不一致。
当前证据显示, hCG辅助治疗对于短期睾丸生精功能有损害;LHRH辅助治疗可改善短期睾丸生精功能;而hCG+LHRH作为辅助疗法与单纯手术治疗隐睾对于远期生精功能无显著影响。考虑到纳入文献数量较少且偏倚风险较高,仍有待更多的研究。
[1]Penson D, Krishnaswami S, Jules A, et al. Effectiveness of hormonal and surgical therapies for cryptorchidism: a systematic review. Pediatrics, 2013, 131(6): 1897-1907
[2]Henna MR, Del Nero RG, Sampaio CZ, et al. Hormonal cryptorchidism therapy: systematic review with meta-analysis of randomized clinical trials. Pediatr Surg Int, 2004, 20(5): 357-359
[3]Kolon TF, Herndon CD, Baker LA, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol, 2014, 192(2): 337-345
[4]Ritzen EM, Bergh A, Bjerknes R, et al. Nordic consensus on treatment of undescended testes. Acta Paediatr, 2007, 96(5): 638-643
[5]Hutson JM, Balic A, Nation T, et al. Cryptorchidism. Semin Pediatr Surg, 2010, 19(3): 215-224
[6]Varela-Cives R, Mendez-Gallart R, Estevez-Martinez E, et al. A cross-sectional study of cryptorchidism in children: testicular volume and hormonal function at 18 years of age. Int Braz J Urol, 2015, 41(1): 57-66
[7]Dunkel L, Taskinen S, Hovatta O, et al. Germ cell apoptosis after treatment of cryptorchidism with human chorionic gonadotropin is associated with impaired reproductive function in the adult. J Clin Invest, 1997, 100(9): 2341-2346
[8]Spinelli C, Strambi S, Busetto M, et al. Effects on normalized testicular atrophy index (TAIn) in cryptorchid infants treated with GnRHa pre and post-operative vs surgery alone: a prospective randomized trial and long-term follow-up on 62 cases. Pediatr Surg Int, 2014, 30(10): 1061-1067
[9]Jallouli M, Rebai T, Abid N, et al. Neoadjuvant gonadotropin-releasing hormone therapy before surgery and effect on fertility index in unilateral undescended testes: a prospective randomized trial. Urology, 2009, 73(6): 1251-1254
[10]Hadziselimovic F, Herzog B. The importance of both an early orchidopexy and germ cell maturation for fertility. Lancet, 2001, 358(9288): 1156-1157
[11]Hadziselimovic F, Huff D, Duckett J, et al. Treatment of cryptorchidism with low doses of buserelin over a 6-months period. Eur J Pediatr, 1987, 146(S2):56-58
[12]Bica DT, Hadziselimovic F. Buserelin treatment of cryptorchidism: a randomized, double-blind, placebo-controlled study. J Urol, 1992, 148(2 Pt 2): 617-621
[13]Cortes D, Thorup J, Visfeldt J. Hormonal treatment may harm the germ cells in 1 to 3-year-old boys with cryptorchidism. J Urol, 2000, 163(4): 1290-1292
[14]Vinardi S, Magro P, Manenti M, et al. Testicular function in men treated in childhood for undescended testes. J Pediatr Surg, 2001, 36(2): 385-388
[15]Schwentner C, Oswald J, Kreczy A, et al. Neoadjuvant gonadotropin-releasing hormone therapy before surgery may improve the fertility index in undescended testes: a prospective randomized trial. J Urol, 2005, 173(3): 974-977
[16]Hadziselimovic F. Successful treatment of unilateral cryptorchid boys risking infertility with LH-RH analogue. Int Braz J Urol, 2008, 34(3): 319-326
[17]Zhao GJ(赵国进),Su XG,Wu DG. The effect of human chorionic gonadotropin on the germ cells in patients with cryptorchidism. Heibei Medicine(河北医学), 2011, 17(3): 319-321
[18]Bertelloni S, Baroncelli GI, Ghirri P, et al. Hormonal treatment for unilateral inguinal testis: comparison of four different treatments. Horm Res, 2001, 55(5): 236-239
[19]Geesaman B, Villanueva-Meyer J, Bluestein D, et al. Effects of multiple injections of HCG on testis blood flow. Urology, 1992, 40(1): 81-83
[20]Heiskanen P, Billig H, Toppari J, et al. Apoptotic cell death in the normal and cryptorchid human testis: the effect of human chorionic gonadotropin on testicular cell survival. Pediatr Res, 1996, 40(2): 351-356
[21]Taskinen S, Wikstrom S. Effect of age at operation, location of testis and preoperative hormonal treatment on testicular growth after cryptorchidism. J Urol, 1997, 158(2): 471-473
[22]Hadziselimovic F, Herzog B. Treatment with a luteinizing hormone-releasing hormone analogue after successful orchiopexy markedly improves the chance of fertility later in life. J Urol, 1997, 158(3 Pt 2): 1193-1195
[23]Demirbilek S, Atayurt HF, Celik N, et al. Does treatment with human chorionic gonadotropin induce reversible changes in undescended testes in boys? Pediatr Surg Int, 1997, 12(8): 591-594
(本文编辑:丁俊杰)
Impact of the adjunctive hormonal therapy on testicular spermatogenic function among cryptorchid: a systematic review and meta-analysis
ZHANGSu,WANGCheng,FUSheng-jun,YANGLi
(DepartmentofUrology,theSecondHospitalofLanzhouUniversity,InstituteofUrologyofLanzhouUniversity,KeyLaboratoryofDiseasesofUrologicalSysteminGansuProvince,GansuNephron-UrologicalClinicalCenter,Lanzhou730030,China)
YANG Li,E-mail:yuze250@163.com
ObjectiveTo systematically evaluate the effect of hormonal therapy on testicular spermatogenic function of children with cryptorchidism.MethodsPubMed, EMBASE, The cochrane library, CBM, CNKI, WanFang Date and VIP were searched to collect relevant studies investigating the impact of hormonal therapy in the testicular spermatogenic function among cryptorchid.Two reviewers independently screened literatures, extracted data, and assessed the risk bias of included studies. As the short-term indicator, the spermatogonia per tubule(S/T) was expressed as mean difference(MD) and its 95% confidence intervals(CI). For the long-term indicator, the proportion of cryptorchidism who will have a normal sperm concentration in adulthood was expressed as risk ratio(RR) with 95% CI.The meta-analysis was performed using RevMan 5.3 software.A fixed-effect model or a random-effect model would be used acording to the heterogeneity.ResultsA total of 4 RCTs(n=168) and 4 Non-randomized controlled trials(NRCT) (n=248) were included. All of these studies had high risk of bias.Among them,3 studies reported the S/T of HCG+surgery group and surgery alone group,the fixed-effect model showed that hCG had decreased the S/T, MD=-0.08,95%CI: -0.13 to -0.03),P=0.002. Four studies was pooled in the meta-analysis using random-effect model. It showed that compared with surgery alone group, LHRH+surgery group had increased S/T, MD=0.34, 95%CI: 0.04 to 0.64,P=0.03, and subgroup analysis indicated the same effect in unilateral or bilateral cryptorchid. Compared with cryptorchid treated by surgery alone, the hCG+LHRH+surgery group did not increase the rate of sperm concentration with the normal range among patients who had history of cryptorchidism, RR=1.46,95%CI:0.24 to 9.06,P=0.68. ConclusionCryptorchid boys treated with hCG show damage in short-term testicular spermatogenic function, and LHRH would improve it. There is no evidence that combined usage of HCG ad LHRH will benefit long-term sperm concentration. Due to the limited quality and quantity of the included studies, more high quality studies are needed to verify the above conclusion.
Cryptorchidism; Human chorionic gonadotropin; Luteinizing hormone releasing hormone; Spermatogenic function; Meta-analysis; Systematic review
兰州大学泌尿外科研究所,兰州大学第二医院泌尿外科 甘肃省泌尿系统疾病临床医学中心,甘肃省泌尿系统疾病研究重点实验室 兰州,730030
杨立,E-mail:yuze250@163.com
10.3969/j.issn.1673-5501.2015.06.008
2015-09-17
2015-12-03)
