丙泊酚及不同剂量瑞马唑仑对舒芬太尼抑制老年患者气管插管反应半数有效剂量的影响
2024-04-01徐海朱婷婷周红梅
徐海 朱婷婷 周红梅

[摘要] 目的 應用序贯法探讨丙泊酚或不同剂量瑞马唑仑对舒芬太尼抑制老年患者气管插管反应的半数有效剂量(50% effective dose,ED50)的影响。方法 选择2022年10至12月在气管插管全身麻醉下接受择期手术的老年患者,美国麻醉医师协会(American Society of Anesthesiologists,ASA)分级Ⅰ、Ⅱ级,年龄65~80岁,将患者采用随机数字表法分为4组:丙泊酚组(P组,诱导时给予丙泊酚2mg/kg)和瑞马唑仑组(R1、R2、R3组,诱导时分别静脉注射瑞马唑仑0.2、0.3、0.4mg/kg)。麻醉诱导时给予Dixon序贯法设定剂量的舒芬太尼后,静脉注射丙泊酚或相应剂量瑞马唑仑及顺式阿曲库铵0.15mg/kg,待4个成串刺激(train of four,TOF)计数为0时行气管插管。若气管插管反应阳性,则下一例患者舒芬太尼剂量提高1个浓度梯度,否则降低1个浓度梯度,各相邻浓度之间的比为1∶1.1,直至出现7个转折点终止研究。采用Probit回归分析计算舒芬太尼抑制老年患者气管插管反应ED50和95%有效剂量(95% effective dose,ED95)以及相应的95%置信区间(confidence interval,CI)。记录所有患者低血压、心动过缓、注射痛等不良反应的发生情况。结果 本研究共纳入老年患者113例,P、R1、R2、R3组分别24、28、30、31例。丙泊酚2mg/kg或0.2、0.3、0.4mg/kg瑞马唑仑时舒芬太尼抑制老年患者气管插管反应的ED50和ED95及相应95%CI分别为:P组ED50为0.236μg/kg(95%CI:0.218~0.256),ED95为0.266μg/kg(95%CI:0.250~0.398);R1组ED50为0.284μg/kg(95%CI:0.265~0.309),ED95为0.329μg/kg(95%CI:0.306~0.478);R2组ED50为0.239μg/kg(95%CI:0.221~0.260),ED95为0.282μg/kg(95%CI:0.261~0.415);R3组ED50为0.198μg/kg(95%CI:0.182~0.211),ED95为0.231μg/kg(95%CI:0.216~0.303)。与P组相比,R1、R2、R3组低血压、心动过缓、注射痛发生率较低(P<0.05)。R2组舒芬太尼ED50与P组相类似,但低血压、注射痛发生率与P组相比较低。结论 随着瑞马唑仑剂量的增加,舒芬太尼抑制老年患者气管插管反应的ED50逐渐降低;在ED50相近的情况下,瑞马唑仑相较于丙泊酚诱导的低血压、心动过缓、注射痛发生率更低,因而在老年患者气管插管全身麻醉中,使用瑞马唑仑诱导更具有优势。
[关键词] 瑞马唑仑;舒芬太尼;老年患者;心血管反应;半数有效剂量
[中图分类号] R614 [文献标识码] A [DOI] 10.3969/j.issn.1673-9701.2024.08.018
Effect of propofol or different doses of remimazolam on median effective dose of sufentanil for suppressing tracheal intubation response in elderly patients
XU Hai, ZHU Tingting, ZHOU Hongmei
Department of Anesthesiology, the Second Hospital of Jiaxing, Jiaxing 314000, Zhejiang, China
[Abstract] Objective To investigate the effect of propofol or different doses of remimazolam on effective dose (ED50) of sufentanil in elderly patients with tracheal intubation response by sequential method. Methods Elderly patients, American Society of Anesthesiologists (ASA) Ⅰ and Ⅱ, aged 65-80 years, undergoing elective surgery under general anesthesia with endotracheal intubation from October to December 2022 were selected and randomly divided into 4 groups: Group P (propofol 2mg/kg) and group R1, R2 and R3 (remimazolam 0.2, 0.3 and 0.4mg/kg) were administered intravenously. During anesthesia induction, sufentanil was given with the dose set by Dixon sequential method, followed by intravenous injection of propofol or corresponding dose of remimazolam and cisatracurium 0.15mg/kg. Tracheal intubation was performed when train of four (TOF) count was 0. If the tracheal intubation response is positive, the sufentanil dose of the next patient is increased by 1 concentration gradient, otherwise, the sufentanil dose is decreased by 1 concentration gradient, and the ratio between adjacent concentrations is 1∶1.1, until 7 turning points appear and the study is terminated. Probit regression analysis was used to calculate the median ED50 and 95% effective dose (ED95) of sufentanil for suppressing tracheal intubation response in elderly patients, and the corresponding 95% CI. The incidence of hypotension, bradycardia, injection pain and other adverse reactions were recorded. Results A total of 113 elderly patients were included in this study, including 24, 28, 30 and 31 patients in P, R1, R2 and R3 groups, respectively. The ED50 and ED95 and corresponding 95% CI of sufentanil for suppressing tracheal intubation response in elderly patients with propofol 2 mg/kg or remimazolam 0.2, 0.3, 0.4mg/kg were: The ED50 and ED95 of group P were 0.236μg/kg (95%CI:0.218–0.256) and 0.266μg/kg (95%CI:0.250–0.398), respectively. The ED50 and ED95 of group R1 were 0.284μg/kg (95%CI:0.265–0.309) and 0.329μg/kg (95%CI:0.306–0.478), respectively. The ED50 and ED95 of R2 group were 0.239μg/kg (95%CI:0.221–0.260) and 0.282μg/kg (95%CI:0.261–0.415), respectively. The ED50 and ED95 of R3 group were 0.198μg/kg (95%CI:0.182–0.211) and 0.231μg/kg (95% CI:0.216–0.303), respectively. The incidence of hypotension, bradycardia and injection pain in R1, R2 and R3 groups were lower than those in P group (P<0.05). The ED50 of sufentanil in group R2 was similar to that in group P, but the incidence of hypotension and injection pain in group R2 was lower than that in group P. Conclusion With the increase of the dose of remimazolam, the ED50 of sufentanil to inhibit tracheal intubation reaction in elderly patients gradually decreased, and in the case of similar ED50, the incidence of hypotension, bradycardia and injection pain induced by remimazolam was lower than that induced by propofol, so remimazolam induction was more advantageous in general anesthesia for tracheal intubation in elderly patients.
[Key words] Remimazolam; Sufentanil; Elderly patients; Cardiovascular response; Median effective dose
在全球老龄化趋势的背景下,越来越多的老年患者在全身麻醉下进行外科手术治疗。此类患者常合并多种疾病,在进行气管插管等刺激性较强的操作时血流动力学的波动较大从而增加心血管系统并发症的风险[1-3]。丙泊酚作为经典的麻醉药物,具有起效快和代谢迅速等优点,在过去的30年中广泛应用于全身麻醉的诱导和维持[4-5]。瑞马唑仑是一种起效迅速、作用时间短的新型苯二氮?类药物,作用于γ-氨基丁酸受体,可通过组织中的非特异性酯酶快速代谢成非活性代谢物,并且可以被氟马西尼快速逆转[6-7]。目前关于丙泊酚或不同剂量瑞马唑仑对舒芬太尼抑制老年患者气管插管反应的半数有效剂量50% effective dose影响的研究少有报道。本研究拟采用改良序贯法探讨丙泊酚或不同剂量瑞马唑仑对舒芬太尼抑制老年患者气管插管反应的ED50的影响,为临床用药提供参考。
1 对象与方法
1.1 研究对象
选择2022年10至12月在气管插管全身麻醉下接受择期手术的老年患者,性别不限,年龄65~80岁,体质量指数(body mass index,BMI)18.5~28kg/m2,美国麻醉医师协会(American Society of Anesthesiologists,ASA)Ⅰ或Ⅱ级,MallampatiⅠ或Ⅱ级,采用随机数字表法分为4组。排除标准:对相关麻醉药物过敏,重要脏器功能损害及精神状态严重异常;剔除标准:插管前出现严重低血压(收缩压<80mmHg,1mmHg=0.133kpa)或严重心动过缓(心率<45次/分),插管时间>30s或插管次数>1次,插管后出现严重高血压(收缩压>180mmHg)或严重心动过速(心率>120次/分),诱导期间新发心律失常。本研究经笔者医院伦理委员会批准(伦理审批号:JXEY- 2022ZFYJ205),患者及家属签署知情同意书。
1.2 麻醉方法
患者无术前用药,常规禁食8h,禁饮2h,入室后常规开放上肢静脉通道,超声引导下桡动脉穿刺置管,鼻导管吸氧2L/min,监测心率(heart rate, HR)、血壓(blood pressure, BP)、血氧饱和度(blood oxygen saturation of pulse, SpO2)、脑电双频指数(bispectral index,BIS)及肌松监测。采用改良序贯试验等比法进行试验,根据预实验结果及相关研究确定舒芬太尼起始剂量为0.25μg/kg,相邻两位患者用药剂量的梯度比为1∶1∶1,静脉注射舒芬太尼(注射时间为60s),1min后静脉注射丙泊酚或瑞马唑仑(P组静脉注射丙泊酚2mg/kg,R1、R2、R3组分别静脉注射瑞马唑仑0.2、0.3、0.4mg/kg,注射时间60s),待BIS≤60后静脉注射顺式阿曲库铵0.15mg/kg(注射时间30s)。充分给氧去氮,待4个成串刺激(train of four,TOF)计数为0时行气管插管。麻醉诱导及气管插管均由经验丰富的麻醉医师完成。若上一位患者出现气管插管反应阳性(以TOF计数为0时的平均动脉压(mean arterial pressure, MAP)和HR为基线值,在气管插管后2min内MAP或HR变化超过基线值的20%),则下一例患者舒芬太尼剂量提高1个浓度梯度,否则降低1个浓度梯度,各相邻浓度之间的比为1∶1.1,直至出现7个转折点。患者气管插管前收缩压(systolic blood pressure,SBP)<80mmHg时静脉注射麻黄碱6mg;HR≤45次/分,静脉注射阿托品0.5mg。
1.3 观察指标
记录低血压、心动过缓、注射痛等不良反应的发生情况。低血压定义为诱导开始时至气管插管前MAP低于基线值的80%;心动过缓定义为心率≤50次/分;注射痛定义为静脉注射丙泊酚或瑞马唑仑后同侧上肢出现逃避动作或患者主诉注射部位疼痛。
1.4 统计学方法
采用SPSS 26.0统计学软件对数据进行处理分析,正态分布计量资料以均数±标准差(![]() )表示,组间比较采用成组t检验,计数资料采用卡方检验。采用Probit回归分析法计算舒芬太尼的ED50、95%有效剂量(95% effective dose,ED95)及95%CI。采用GraphPad Prism 9软件绘制序贯试验图和剂量-效应关系曲线图。P<0.05为差异有统计学意义。
)表示,组间比较采用成组t检验,计数资料采用卡方检验。采用Probit回归分析法计算舒芬太尼的ED50、95%有效剂量(95% effective dose,ED95)及95%CI。采用GraphPad Prism 9软件绘制序贯试验图和剂量-效应关系曲线图。P<0.05为差异有统计学意义。
2 结果
2.1 一般资料比较
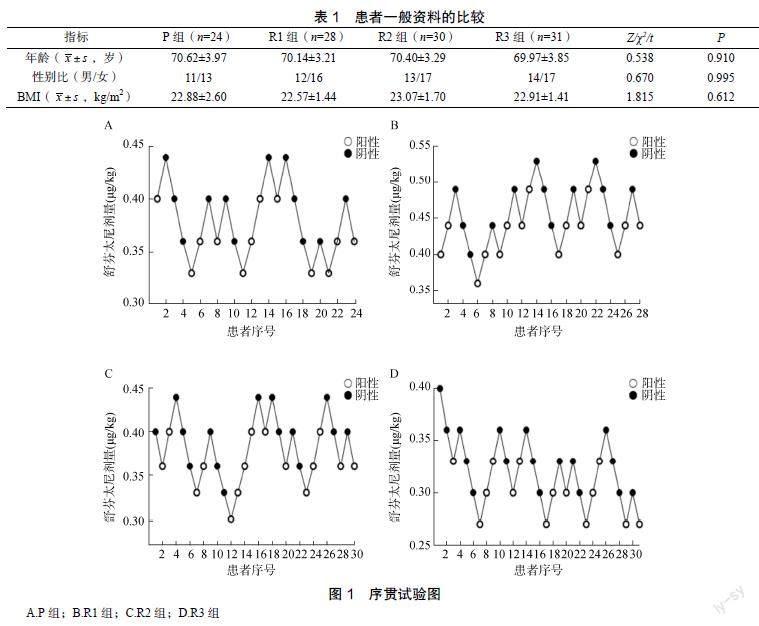
本研究共纳入接受气管插管全身麻醉的老年患者113例,P、R1、R2、R3组各24、28、30、31例。P、R1、R2、R3组男性患者各11、12、13、14例,女性患者各13、16、17、17例,P、R1、R2、R3组的年龄分别为(70.62±3.97)岁、(70.14±3.21)岁、(70.40±3.29)岁、(69.97±3.85)岁,BMI分别为(22.88±2.60)kg/m2、(22.57±1.44)kg/m2、(23.07±1.70)kg/m2、(22.91±1.41)kg/m2。各组基线资料比较差异无统计学意义(P>0.05),见表1。
2.2 ED50、ED95以及相应的95%CI
P、R1、R2、R3组气管插管反应阳性患者分别为12、15、15、14例,阴性患者分别为12、13、15、17例。各组舒芬太尼抑制老年患者气管插管反应剂量见序贯试验见图1,各组舒芬太尼抑制老年患者气管插管反应的ED50分别为:P组ED50为0.236μg/kg(95%CI:0.218~0.256),ED95为0.266μg/kg(95%CI:0.250~0.398);R1组ED50为0.284μg/kg(95%CI:0.265~0.309),ED95为0.329μg/kg(95%CI:0.306~ 0.478);R2组ED50为0.239μg/kg(95%CI:0.221~ 0.260),ED95为0.282μg/kg(95%CI:0.261~0.415);R3组ED50为0.198μg/kg(95%CI:0.182~0.211),ED95为0.231μg/kg(95%CI:0.216~0.303)。见图1。
2.3 不良反应发生率比较
P组低血压、心动过缓及注射痛发生率均高于R1、R2、R3组,差异有统计学意义(P<0.05)
3 讨论
随着我国社会老龄化的加剧,接受气管插管全身麻醉外科治疗的老年患者日益增多。老年患者器官功能储备低下,在全身麻醉诱导期相较于一般患者存在更多风险,尤其是血流动力学的不稳定,不利于患者术后康复。舒芬太尼是一种强效阿片类镇痛药,广泛应用于全身麻醉的诱导中,与镇静药物的联合使用可有效抑制气管插管反应。丙泊酚具有较高的脂溶性,可在短时间内穿过血-脑脊液屏障从而达到深度镇静的作用,但其同时可诱发多种心肺并发症,例如低氧血症、低血压、心律失常和呼吸抑制等,尤其是对于脏器功能储备较差的老年患者的使用存在局限性[8-10]。瑞马唑仑作为超短效苯二氮?类药物,对循环、呼吸抑制较轻,主要通过组织酯酶代谢,对肝肾功能影响较小,因而理论上是老年患者全身麻醉诱导理想的镇静药物[11-12]。
瑞马唑仑在麻醉诱导中常用的剂量为0.2~0.4mg/kg或6~12mg/(kg·h)持续泵注[13-14]。因而根据预实验和相关研究,设置瑞马唑仑0.2、0.3和0.4mg/kg与丙泊酚进行比较,以探究在不同剂量瑞马唑仑镇静的情况下舒芬太尼的半数有效剂量。序贯法是计算半数有效剂量的经典方法,能够在小样本量的情况下得出较为精确的数据,在临床上广为应用[15]。因此本研究采用序贯法研究丙泊酚或不同剂量瑞马唑仑对舒芬太尼抑制老年患者气管插管反应的量效关系。本研究结果显示,随着瑞马唑仑剂量的增加,舒芬太尼抑制老年患者气管插管反应的ED50及ED95降低,同时,在舒芬太尼抑制老年患者气管插管反应的ED50相似的情况下,与R2组相比,丙泊酚组低血压、心动过缓、注射痛等不良反应发生率更高。
既往研究表明,与丙泊酚相比,瑞马唑仑用于老年患者无痛胃镜诊疗时低血压、呼吸抑制及注射痛等不良反应的发生率明显降低,心血管抑制作用轻微,在稳定血流动力学指标方面更具优势[16]。同样,在气管插管全身麻醉的诱导中,与丙泊酚相比,瑞马唑仑同样显示出血流动力学稳定方面的优势,减少低血压、心动过缓的发生率及血管活性药物的使用[17]。此外,在R1、R2、R3组中均未观察到注射痛,这与既往研究结果相一致[18-20]。
本研究的不足之处在于未关注患者术后恢复质量指标,包括术后谵妄等。未纳入ASA分级Ⅱ级以上的危重症老年患者以探究丙泊酚或不同剂量瑞马唑仑的量效关系及不良反应的发生。另外,需要进行进一步的研究以探明性别的影响。
利益冲突:所有作者均声明不存在利益冲突。
[参考文献]
[1] AURINI L, WHITE P F. Anesthesia for the elderly outpatient[J]. Curr Opin Anaesthesiol, 2014, 27(6): 563–575.
[2] BROWN E N, PURDON P L. The aging brain and anesthesia[J]. Curr Opin Anaesthesiol, 2013, 26(4): 414–419.
[3] 喬迎帅, 冯爱敏, 张震, 等. 联合舒芬太尼时瑞马唑仑抑制气管插管心血管反应的半数有效剂量[J]. 临床麻醉学杂志, 2021, 37(10): 1034–1037.
[4] SAHINOVIC M M, STRUYS M, Absalom A R. Clinical pharmacokinetics and pharmacodynamics of propofol[J]. Clin Pharmacokinet, 2018, 57(12): 1539–1558.
[5] KIVLEHAN F, CHAUM E, Lindner E. Propofol detection and quantification in human blood: The promise of feedback controlled, closed-loop anesthesia[J]. Analyst, 2015, 140(1): 98–106.
[6] SHENG X Y, LIANG Y, YANG X Y, et al. Safety, pharmacokinetic and pharmacodynamic properties of single ascending dose and continuous infusion of remimazolam besylate in healthy Chinese volunteers[J]. Eur J Clin Pharmacol, 2020, 76(3): 383–391.
[7] KIM K M. Remimazolam: Pharmacological characteristics and clinical applications in anesthesiology[J]. Anesth Pain Med (Seoul), 2022, 17(1): 1–11.
[8] 樊迪, 紀木火, 杨建军. 衰弱患者术前评估及围术期管理的研究进展[J]. 中华麻醉学杂志, 2021, 41(3): 381–384.
[9] NAZIR M, SALIM B, KHAN F A. Pharmacological agents for reducing the haemodynamic response to tracheal intubation in paediatric patients: A systematic review[J]. Anaesth Intensive Care, 2016, 44(6): 681–691.
[10] OGAWA T, TOMODA T, KATO H, et al. Propofol sedation with a target-controlled infusion pump in elderly patients undergoing ERCP[J]. Gastrointest Endosc, 2020, 92(2): 301–307.
[11] SNEYD J R, RIGBY A E. Remimazolam for anaesthesia or sedation[J]. Curr Opin Anaesthesiol, 2020, 33(4): 506-511.