皮肤微针联合外用5-氟尿嘧啶诱导白癜风复色疗效观察
2021-12-17廖蕾雷铁池廖志锴
廖蕾 雷铁池 廖志锴
[摘要]目的:观察皮肤微针联合5-氟尿嘧啶(5-FU)诱导白癜风复色的疗效。方法:选择稳定期非节段型白癜风15例,共30片白斑皮损。随机分为两组:联合组:15片皮损,给予1.0mm的皮肤微针针刺皮肤联合外涂2.5% 5-FU溶液,局部封包,每2周1次,共6次;对照组:15片皮损,仅予1.0mm微针针刺皮肤,每2周1次,共6次。每次治疗前用透明薄膜描记点计数法(Point counting method)测量白斑面积。结果:两组白癜风皮损经3个月治疗后,联合组总有效率66.7%,明显优于单用微针组的20.0%,两组比较差异具有统计学意义(P<0.05)。结论:皮肤微针联合外用5-FU可诱导白癜风复色,是一种安全有效的治疗方法。
[关键词]微针;5-氟尿嘧啶;复色;白癜风
[中图分类号]R758.4+1 [文献标志码]B [文章编号]1008-6455(2021)11-0054-03
Induction of Vitiligo Repigmentation by Skin Microneedling Combined with Topical 5-Fluorouracil
LIAO Lei, LEI Tie-chi, LIAO Zhi-kai
(Department of Dermatology and Venereology, Renmin Hospital of Wuhan University, Wuhan 430060, Hubei,China)
Abstract: Objective To evaluate the effect of skin microneedling combined with topical 5-fluorouracil in the induction of vitiligo repigmentation. Methods 15 stable non-segmental vitiligo patients with 30 vitiliginous patches were recruited in this study. The 15 vitiliginous patches of combined treatment group were treated with 1.0-mm-depth microneedling and then topically applied with 2.5% 5-fluorouracial solution under occlusive dressing, while the other 15 vitiliginous patches were only treated with 1.0-mm-depth microneedling. This procedure was repeated every 2 weeks for 6 sessions. The area of vitiliginous patches were measured by point counting method before each session. Results After 3 months of treatment, the effective rate was significantly better in combined treatment group (66.7%) compared with microneedling only group (20.0%) (P<0.05). Conclusion Skin microneedling combined with 5-FU is a safe and effective treatment for inducing repigmentation in vitiligo.
Key words: microneedling; 5-fluorouracil; repigmentation; vitiligo
白癜风是一种临床常见的慢性获得性色素脱失性皮肤病,其确切的发病机制并不十分清楚。选择性自身免疫性黑素细胞破坏被认为是导致皮肤斑片状色素脱失的主要病因[1-2]。白癜风发病常见于年轻人,给患者带来沉重的精神负担且导致其生活质量下降[1]。目前临床缺乏单一有效的治疗方法。311nm NB-UVB和308nm准分子光照射等光疗是诱导白癜风复色(Repigmentation)的一线治疗选择[3-4]。然而,有部分白癜风皮损对光疗产生抵抗,又被称之为难治性白癜风(Refractory vitiligo)[5]。近年来,也有报道用点阵CO2激光[6]、磨皮术[7]和微针[8]等手段可诱导这些难治性白癜风成功复色。本研究初步观察了1.0mm皮肤微针联合外用5-氟尿嘧啶(5-FU)治疗白癜风的临床疗效,现将结果报道如下。
1 资料和方法
1.1 一般资料:选择2018年10月-2019年10月在武汉大学人民医院皮肤科门诊就诊的15例稳定期白癜风患者为研究对象,其中男10例,女5例。年龄19~48岁,平均33.93岁,病程0.5~7年,平均3.33年。皮损分布:躯干6例,颈项4例,前臂2例,手背指背3例。纳入标准:①年龄18~60岁;②非节段型白癜风,病情稳定至少3个月;③最近1个月内无系统治疗及外用药物治疗史;④至少2片对称分布的皮损;⑤既往糖皮质激素或光疗治疗反应差。排除標准:①儿童,年龄<10岁;②有其他皮肤疾病或高血压、心脏病等系统性疾病者;③妊娠或哺乳期女性;④过敏体质者,尤其是对本研究已知药物成分过敏者;⑤瘢痕体质者;⑥有精神心理障碍者。所有患者入组前均签署知情同意书。
1.2 治疗方法:选取对称分布的2片皮损为靶皮损,采用计算机随机数字法分为两组。其中,联合治疗组(结合微针+5-Fu治疗)为随机数字中奇数患者的左侧皮损和偶数患者的右侧皮损,而对照组(仅接受微针治疗)为奇数患者的右侧皮损和偶数患者的左侧皮损。联合治疗组:皮损部位用利多卡因软膏(同方药业集团有限公司产)封包1h,0.5%活力碘消毒,1.0mm微针(滚轮表面含有540个长度1.0mm的不锈钢针,广州领美美容美体器材有限公司)针刺皮肤,在水平和垂直方向往返5次,以均匀力度缓慢针刺皮肤至点状出血。随后,将2.5% 5-FU溶液(南通精华制药有限公司产)均匀滴加在针刺伤口表面,透明敷料局部封包30min,外用莫匹罗星(百多邦)软膏预防感染。针刺区外用2.5% 5-FU溶液,每天1次,共2周。每2周为1个疗程,共治疗3个月。对照组微针治疗同联合治疗组。
1.3 疗效评价:治疗前用伍德灯和数码相机拍照。参照文献[9]用透明薄膜描记/点计数法(Point counting method)测量白斑面积。复色率为治疗结束时复色面积占原皮损面积的百分比,分为四个等级:无效:复色率<25%;有效:复色率25%~49%;显效:复色率50%~74%;痊愈:复色率≥75%[10]。治疗成功的标准为复色率≥50%,总有效率=(痊愈+显效)例数/总例数×100%[10]。观察不良反应包括疼痛、瘙痒、红斑、毛细血管扩张及瘢痕等。
1.4 统计学分析:采用SPSS 22.0软件进行数据分析,等级资料采用例数表示,组间比较采用Wilcoxon秩和检验,计数资料用[例(%)]表示,组间比较采用χ2检验,P<0.05为差异具有统计学意义。
2 结果
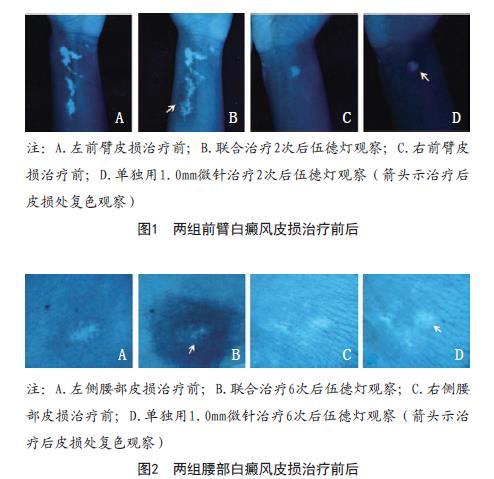
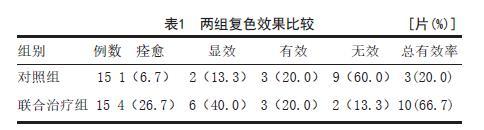
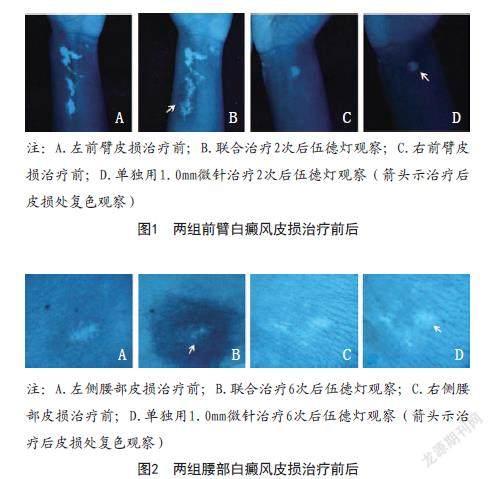
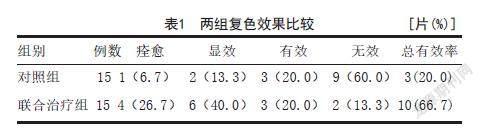
2.1 复色疗效:15例白癜风患者,共30片皮损,治疗3个月后观察复色效果。联合治疗组总有效率为66.7%(10/15),对照组总有效率为20.0%(3/15),联合治疗组的总有效率明顯优于对照组,差异有统计学意义(Z=-2.767,P=0.007),见表1。典型病例见图1~2。
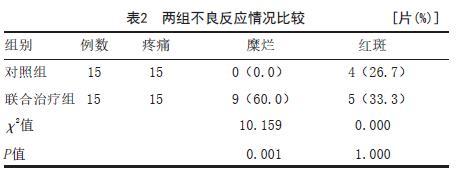
2.2 不良反应情况:微针针刺皮肤后,15例白癜风患者的30片针刺区均出现了可忍受的疼痛,治疗后数小时内疼痛均可缓解。联合治疗组9片(60.0%)白斑部位出现局部轻度糜烂,外涂莫匹罗星软膏,2个月后皮肤均恢复正常,而对照组未发生糜烂,两组糜烂发生率比较差异具有统计学意义(P<0.05),两组红斑发生率比较差异无统计学意义(P>0.05)。见表2。

3 讨论
除了用311nm NB-UVB和308nm准分子光照射等光疗诱导白癜风复色外,近年还发现对一些光疗抵抗的难治性白癜风,如:磨皮术、微针和点阵CO2激光等以及化学性创伤(Chemical trauma),可通过诱导皮肤物理性创伤(Physical trauma),如:外涂5-FU和三氯醋酸等有效激发白癜风皮损出现复色[11-12]。尽管已有临床报道显示外用5-FU治疗白癜风有效[13-14],但对其作用机制仍缺乏足够的认识。一般认为5-FU是一种广谱抗肿瘤药物,其分子结构为天然尿嘧啶5位上的氢被氟取代。当这种尿嘧啶类似物进入人表皮细胞后,被快速转变为5-氟尿嘧啶脱氧核苷酸,进而抑制胸腺嘧啶核苷酸合成酶(Thymidylate synthetase)活性,使脱氧尿嘧啶核苷酸不能转化为胸腺嘧啶核苷酸,抑制了DNA合成[13]。在临床上,外用5-FU主要被用于治疗一些以高有丝分裂率为特征的皮肤病,如:非黑素瘤皮肤癌、日光性角化病、甲银屑病和病毒疣等[13]。对日光性角化病和其他具有角质形成细胞癌危险因素的患者,面部、头皮和耳部局部使用5%的5-FU,降低了进展为鳞状细胞癌的风险[15-16]。局部外用5-FU治疗过程中观察到皮肤刺激、糜烂和水疱等不良反应,大部分短暂且可耐受,主要取决于剂量浓度和用药时间[13,17]。药代动力学评价表明,5%和0.5%氟尿嘧啶乳膏的系统性吸收分别为2.4%和0.55%,24h后的皮肤残留量分别为54%和86%~92%,低浓度的氟尿嘧啶不良反应发生的风险小[18-19]。本研究将2.5% 5-FU溶液应用于微针治疗的皮肤伤口,60.0%皮损局部糜烂,外用莫匹罗星软膏后均好转。此外,部分患者局部出现明显的色素沉着[17]。一种解释是5-FU对表皮细胞产生的选择性细胞毒性,很可能表皮内快速增殖的角质形成细胞较增殖相对缓慢的黑素细胞对5-FU更为敏感[20]。
由于皮肤角质层所形成的屏障,绝大多数药物无法以治疗速度穿过皮肤,从而严重限制了经皮给药的疗效。5-FU是亲水性药物,不易渗透角质层屏障[21]。本研究采用1.00mm微针造成表皮创伤,联合局部外用5-FU增加药物的渗透和吸收。至于创伤诱导皮肤色素沉着的机制仍不完全清楚,有人推测可能是创伤激发了表皮的炎症反应,使表皮环境中的生长因子、基质金属蛋白酶9(MMP9)以及细胞外基质成分上调,借此刺激了黑素生成、黑素细胞增殖和迁移[11]。也有人推测皮肤创伤可能动员了毛囊隆突区处于休眠状态的黑素细胞干细胞(Melanocyte stem cell,MSC),被激活的黑素细胞发生增殖、移行进入了表皮[12]。笔者推测,由于5-FU的选择性和差异性的细胞毒性,应用于伤口将抑制伤口上皮化,为黑素细胞再生提供时间和空间条件。
人表皮黑素細胞通过其树突与周围约36个角质形成细胞形成表皮黑素单元(Epidermal melanin unit,EMU)。角质形成细胞对皮肤色素沉着有明显的调节作用。黑素细胞产生含有黑色素的黑素小体并转移到角质形成细胞,角质形成细胞分泌细胞因子促进黑素合成和黑素小体运输[22-23]。当遭到微小创伤时,皮肤立即启动伤口愈合(Wound-healing)机制进行创伤修复[23]。伤口床的炎症细胞(主要是巨噬细胞)释放大量的促炎因子或生长因子刺激位于表皮基底层和毛囊隆突区或皮脂腺等部位的表皮干细胞活化、增殖,产生大量新生角质形成细胞。新生的角质形成细胞通过桥粒重塑(Desmosomal remodeling)等表型改变与周围的角质形成细胞解离,移行至伤口床以填补缺失的表皮细胞,这一过程又被称为再上皮化(Re-epithelialisation)[23]。活化的角质形成细胞与表皮中的黑素细胞及其他细胞相互作用,细胞增殖分化,形成复层上皮,恢复皮肤屏障功能。本研究用1.0mm微针针刺皮肤联合外涂2.5% 5-FU溶液诱导白癜风复色,是一种安全、有效的疗法。
[参考文献]
[1]Rodrigues M,Ezzedine K,Hamzavi I,et al.New discoveries in the pathogenesis and classification of vitiligo[J].J Am Acad Dermatol,2017, 77(1):1-13.
[2]Iannella G,Greco A,Didona D,et al.Vitiligo:pathogenesis,clinical variants and treatment approaches[J].Autoimmun Rev,2016,15(4):335-343.
[3]Zubair R,Hamzavi IH.Phototherapy for vitiligo[J].Dermotol Clin, 2020, 38(1):55-62.
[4]Mohammad TF,Al-Jamal M,Hamzavi IH,et al.The vitiligo working group recommendations for narrowband ultraviolet B light phototherapy treatment of vitiligo[J].J Am Acad Dermatol,2017,76(5):879-888.
[5]Fenniche S,Zaouak A,Tanfous AB,et al.Successful treatment of refractory vitiligo with a combination of khellin and 308-nm excimer lamp:an open-label, 1-year prospective study[J].Dermatol Ther(Heidelb),2018, 8(1):127-135.
[6]Kim HJ,Hong ES,Cho SH,et al.Fractional carbon dioxide laser as an "add-on" treatment for vitiligo:a Meta-analysis with systematic review[J].Acta Derm Venereol,2018,98(2):180-184.
[7]Bayoumi W,Fontas E,Sillard L,et al.Effect of a preceding laser dermabrasion on the outcome of combined therapy with narrowband ultraviolet B and potent topical steroids for treating nonsegmental vitiligo in resistant localizations[J].Br J Dermatol,2012, 166(1):208-211.
[8]Attwa EM,Khashaba SA,Ezzat NA.Evaluation of the additional effect of topical 5-fluorouracil to needling in the treatment of localized vitiligo[J].J Cosmet Dermatol,2019,19(6):1473-1478.
[9]Aydin F,Senturk N,Sahin B,et al.A practical method for the estimation of vitiligo surface area: a comparison between the point counting and digital planimetry techniques[J].Eur J Dermatol,2007,17(1):30-32.
[10]Mohamed HA,Mohammed GF,Gomaa AH,et al.Carbon dioxide Laser plus topical 5-fluorouracil: a new combination therapeutic modality for acral vitiligo[J].J Cosmet Laser Ther,2015,17(4):216-223.
[11]El Mofty M,Esmat S,Hunter N,et al.Effect of different types of therapeutic trauma on vitiligo lesions[J].Dermatol Ther,2017, 30(2):e12447.
[12]Awad SS.Dermabrasion may repigment vitiligo through stimulation of melanocyte precursors and elimination of hyperkeratosis[J].J Cosmet Dermatol,2012,11(4):318-322.
[13]Moore AY.Clinical applications for topical 5-fluorouracil in the treatment of dermatological disorders[J].J Dermatol Treat,2009, 20(6):328-335.
[14]Abdelwahab M,Salah M,Samy N,et al.Effect of topical 5-fluorouracil alone versus its combination with Erbium:YAG (2 940nm) laser in treatment of vitiligo[J].Clin Cosmet Investig Dermatol,2020,13:77-85.
[15]Weinstock MA,Thwin SS, Siegel JA, et al.Chemoprevention of basal and squamous cell carcinoma with a single course of fluorouracil, 5%, cream:a randomized clinical trial[J].JAMA Dermatol,2018,154(2):167-174.
[16]Rosenberg AR,Tabacchi M,Ngo KH,et al.Skin cancer precursor immunotherapy for squamous cell carcinoma prevention[J].JCI Insight,2019,4(6):e125476.
[17]Dodds A,Chia A,Shumack S.Actinic keratosis:rationale and management[J].Dermatol Ther (Heidelb),2014,4(1):11-31.
[18]Levy S,Furst K,Chern W. A pharmacokinetic evaluation of 0.5% and 5% fluorouracil topical cream in patients with actinic keratosis[J].Clin Ther,2001,23(6):908-920.
[19]Levy S,Furst K,Chern W.A comparison of the skin permeation of three topical 0.5% Fluorouracil formulations with that of a 5% formulation[J].Clin Ther,2001,23(6):901-907.
[20]Longley DB,Harkin DP,Johnston PG.5-Fluorouracil: mechanisms of action and clinical strategies[J].Nat Rev Cancer,2003,3(5):330-338.
[21]Ran W,Zhimin W,Shufang Y,et al. A molecular interpretation on the different penetration enhancement effect of borneol and menthol towards 5-fluorouracil[J].Int J Molecul Sci,2017,18(12):2747.
[22]Vandamme N,Berx G.From neural crest cells to melanocytes: cellular plasticity during development and beyond[J].Cell Mol Life Sci,2019,76(10):1919-1934.
[23]Horst BT,Chouhan G,Moiemen NS,et al.Advances in keratinocyte delivery in burn wound care[J].Adv Drug Deliv Rev,2018,123:18-32.
[收稿日期]2020-06-11
本文引用格式:廖蕾,雷鐵池,廖志锴.皮肤微针联合外用5-氟尿嘧啶诱导白癜风复色疗效观察[J].中国美容医学,2021,30(11):54-57.
