应用罗哌卡因减轻腹腔镜阑尾切除术后疼痛临床分析
2020-07-04鞠雷
鞠雷
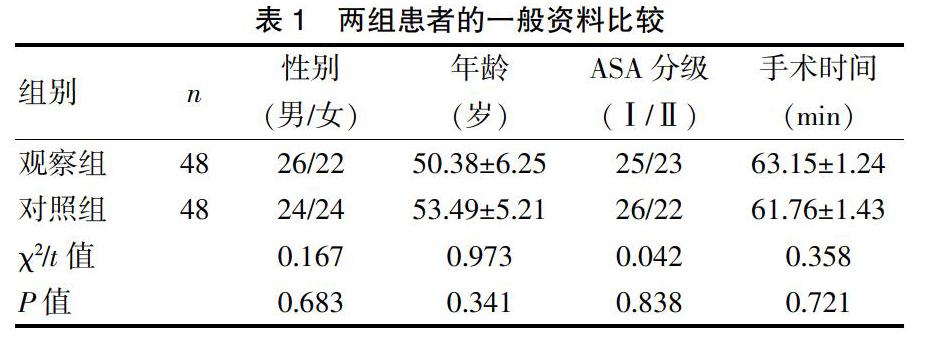


[摘要] 目的 探討在腹腔镜阑尾切除术中罗哌卡因局部麻醉对减轻术后疼痛的应用。 方法 于2017年3月~2018年9月在盘锦市中心医院行腹腔镜阑尾切除手术患者96例,随机分成对照组和观察组,对照组未做任何止痛处理,观察组应用罗哌卡因注射液于切口下局部麻醉,比较两组术后切口的疼痛情况、下床活动情况、不良反应等。 结果 观察组在术后6、12、24h的疼痛评分分别为(4.3±1.0)分、(3.5±1.2)分、(3.0±1.5)分,对照组在术后6、12、24 h的疼痛评分分别为(5.2±1.1)分、(6.3±2.1)分、(6.0±1.8)分,观察组明显低于对照组,差异有统计学意义(P<0.05)。观察组术后下床活动时间(8.7±2.3)h、排气时间(10.7±2.1)h,对照组术后下床活动时间(11.3±2.1)h、排气时间(12.7±2.3)h,差异有统计学意义(P<0.05)。在术后不良反应上,观察组中出现胃肠功能障碍3例,联合止痛药物治疗2例,对照组中出现胃肠功能障碍10例,联合止痛药物治疗9例,差异有统计学意义(P<0.05)。 结论 利用罗哌卡因在切口下局部麻醉可以减轻腹腔镜阑尾切除术后切口疼痛。
[关键词] 急性阑尾炎;腹腔镜阑尾切除;罗哌卡因;术后切口疼痛
[中图分类号] R656.8 [文献标识码] B [文章编号] 1673-9701(2020)12-0057-04
[Abstract] Objective To investigate the application of ropivacaine for local anesthesia during laparoscopic appendectomy to relieve postoperative pain. Methods 96 cases of laparoscopic appendectomy were performed at Panjin Central Hospital from March 2017 to September 2018. They were randomly divided into control group and observation group. The control group was not given any analgesic treatment, and the observation group was given ropivacaine injection under local anesthesia under the incision. Postoperative incision pain, off-bed activity, and adverse reactions were compared between the two groups. Results The pain scores in the observation group at 6 hours, 12 hours, and 24 hours after surgery were (4.3±1.0) points, (3.5±1.2) points, and (3.0±1.5) points. The pain scores in the control group at 6 hours, 12 hours, and 24 hours after surgery were (5.2±1.1) points, (6.3±2.1) points, and (6.0±1.8) points. The observation group was significantly lower than that in the control group, and the difference was statistically significant(P<0.05). In the observation group, the off-bed activity time was(8.7±2.3) hours, and the exhaust time was(10.7±2.1) hours. The off-bed activity time in the control group was (11.3±2.1) hours and the exhaust time was (12.7±2.3) hours. The differences were statistically significant(P<0.05). In terms of postoperative adverse reactions, there were 3 cases of gastrointestinal dysfunction and 2 cases of combined analgesic medication in the observation group, and there were 10 cases of gastrointestinal dysfunction and 9 cases of analgesic medication in the control group. The differences were statistically significant(P<0.05). Conclusion Local anesthesia with ropivacaine under the incision can reduce incision pain after laparoscopic appendectomy.
近些年来,围手术期疼痛管理的目标始终是围绕减轻患者痛苦,使其在术后能够尽早活动,减少住院时长,让患者满意。围手术期疼痛的主要原因是组织创伤(如手术切开、分离、烧灼)所导致的炎症或直接的神经损伤(如神经的离断、牵拉或受压)。当组织受到创伤后,就会在局部释放许多炎症介质,而这些炎性介质会提高损伤周围区域对疼痛刺激的敏感性(痛觉过敏),也可以对非伤害性刺激错误地产生疼痛感(触诱发痛)。导致上述这些痛觉过敏和触诱发痛的其他机制还包括:外周疼痛感受器的敏化(原发性痛觉过敏)以及中枢神经系统神经元兴奋性增高(继发性痛觉过敏)。通过这个疼痛传导通路使患者感受疼痛,而临床上各种类型的镇痛药物均是该通路的靶点。近些年随着术后快速康复(ERAS)理念的提出,许多临床医生都对围手术期的疼痛管理进行了广泛研究[8]。比如术后应用止痛泵,即静脉自控镇痛,虽可以减轻一定程度的疼痛,但恶心、呕吐、嗜睡等不良反应的发生率较高,且电子镇痛装置及配伍药物费用均较高,无形中增加了医疗成本。近年也有主张围手术期应用加巴喷丁和普瑞巴林等药物进行镇痛,这些药物作用于神经递质的活性,可以抑制或增加它们的活性,但是在这些药物使用后有显著的镇静和头晕发生率,并且有益程度不同[9],尤其老年人联合应用镇痛药可能会出现呼吸抑制[10],并且像加巴喷丁类药物也存在滥用可能性[11]。另外针对特定患者(如儿童和难以建立静脉通路的患者),通过鼻腔和口服氯胺酮可能会有效缓解急性疼痛[12-13],但在预防术后慢性疼痛综合征方面没有确切有效的给药方案和给药时机。临床局麻药直接浸润皮下组织层,可有效阻断从表皮和真皮层游离神经纤维冲动的传导,以减少或消除感觉。因此人们想到了应用利多卡因注射液局麻药来对切口进行局部浸润麻醉,但通过临床观察,利多卡因注射液虽然起效很快,一般施用1~3 min后即可生效,但镇痛效果一般只能维持1~3 h,这离人们期待的术后止痛的理想效果还相差的很远。因此找到一种既有效镇痛又费用较低的方法成为各位临床医生关注的焦点。而新型长效麻醉药的出现,似乎可以成为有效的解决办法。罗哌卡因就是其中的典型代表药物,它可以对人体的感觉和运动起到有效的抑制作用[14],能起到5.5个药物半衰期的镇痛作用,对于缓解术后疼痛效果明显。罗哌卡因是一种纯左旋对映异构体的酰胺类局麻药,通过升高神经动作电位的阈值,延缓神经冲动的扩布,降低动作电位升高的速度,发挥阻断神经冲动的产生和传导的作用,具有运动与感觉神经分离阻滞以及收缩血管等特点。麻醉作用的产生与神经纤维的轴径、髓鞘形成和传导速度有关,对心脏毒性作用低,且局部麻醉浸润的不良反应极少[15-16]。局部浸润罗哌卡因不但可以减轻术后的急性疼痛,而且也可以大大緩解术后慢性疼痛,尤其是开刀前进行局部浸润,更可以明显提高术后镇痛效果[17]。本研究表明,在切皮前以及关腹缝合前,分别应用1%罗哌卡因注射液在腹腔镜下阑尾切除手术的戳孔处局部浸润,分析患者在术后6 h、12 h、24 h疼痛情况,可见观察组的疼痛评分明显低于对照组,有显著差异。而在术后1 h两组的疼痛评分无明显差异,考虑与全麻术后时间较短,患者在全麻清醒恢复过程中对疼痛刺激反应不敏感有关。而在患者术后下床活动时间及术后排气时间,观察组明显早于对照组,有显著差异。在术后出现胃肠功能障碍及追加止痛药的例数,观察组明显少于对照组,有显著差异。在术后切口感染的发生,两组无明显差异。
综上所述,利用罗哌卡因在腹壁戳孔下局部浸润,对腹腔镜阑尾切除的术后镇痛效果显著,方法简单,安全性高,且费用低,值得临床推广。
[参考文献]
[1] Salminen P,Paajanen H,Rautio T,et al.Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis the APPAC randomized clinical trial[J]. JAMA,2015,313(23):2340-2348.
[2] 胡三元,展翰翔.腹腔镜手术并发症的预防与处理[J].国际外科学杂志,2017,44(4):272-274.
[3] 尹鹭华.超声引导下TAP阻滞在腹腔镜手术患者术后镇痛的应用观察[J].中外医学研究,2018,16(24):156-158.
[4] Raghvendra KP,Thapa D,Mitra S,et al.Postoperative pain relief following hysterectomy:A randomized controlled trial[J].Midlife Health,2016,7(2):65-68.
[5] Berrios-Torres SI,'Umscheid CA,Bratzler DW,et al.Centers for disease control and prevention guideline for the preventio of surgical site infection[J].JAMA,2017,152(8):784-791.
[6] 吴迅,刘春,钱皓,等,腹腔镜阑尾切除术与开腹阑尾切除术在阑尾炎治疗中的应用效果比较[J].现代生物医学进展,2016,(29):5742-5745.
[7] 姜景卫,鲁华荣,周召文,等.地佐辛联合罗哌卡因局部麻醉预处理对腹腔镜下胆囊切除术男性患者苏醒期躁动的影响[J].中国医药导报,2016,13(7):72-75.
[8] 戴瑜,孙雪冬,刘敬臣.腹横肌平面阻滞与胸椎硬膜外阻滞对腹腔镜结直肠手术后镇痛效果的对比研究[J].广西医科大学学报,2017,34(8):1213-1216.
[9] Fabritius ML,Strom C,Koyuncu S,et al.Benefit and harm of pregabalin in acute pain treatment:A systematic review with meta-analyses and trial sequential analyses[J].British Journal of Anaesthesia,2017,119(4):775-791.
[10] Cavalcante AN,Sprung J,Schroeder DR,et al.Multimodal analgesic therapy with gabapentin and its association with postoperative respiratory depression[J].Anesthesia and Analgesia,2017,125(1):141-146.
[11] Evoy KE,Morrison MD,Saklad SR.Abuse and misuse of pregabalin and gabapentin[J].Drugs,2017,77(4):403-426.
[12] Yenigun A,Yilmaz S,Dogan R,et al.Demonstration of analgesic effect of intranasal ketamine and intranasal fentanyl for postoperative pain after pediatric tonsillectomy[J].International Journal of Pediatric Otorhinolaryngology,2018,104:182-185.
[13] Schwenk ES,Viscusi ER,Buvanendran A,et al.Consensus guidelines on the use of intravenous ketamine infusions for acute pain management from the American society of regional anesthesia and pain medicine,the American academy of pain medicine,and the American society of anesthesiologists[J].Regional Anesthesia and Pain Me-dicine,2018,43(5):456-466.
[14] De Oliveira GS,Castro-Alves LJ,Nader A,et al.Transversus abdominis plane block to ameliorate postoperative pain outcomes after laproscopic surgery:A meta-analysis of randomized controlled trials[J].Anesthesia and Analgesia,2014,118(2):454-463.
[15] 李秋紅,徐铭军.妇科手术患者围手术期镇痛药物及方法的应用进展[J].山东医药,2017,57(3):104-106.
[16] Ollier E,Heritier F,Bonnet C,et al.Population pharmacokinetic model of free and total ropivacaine after transversus abdominis plane nerve block in patients undergoing liver re-section[J].British Journal of Clinical Pharmacology,2015,80(1):67-74.
[17] Bindra TK,Kumar P,Rani P,et al.Preemptive analgedia by intraperitoneal instillation of ropivacaine in laparoscopic cholecys-tectomy[J].Anesth Essays Res,2017,11(3):740-744.
(收稿日期:2020-01-02)
