宫颈疾病行手术治疗后继发阴道上皮内肿瘤的临床特征及结局分析
2020-01-11邱建黄筱竑
邱建 黄筱竑
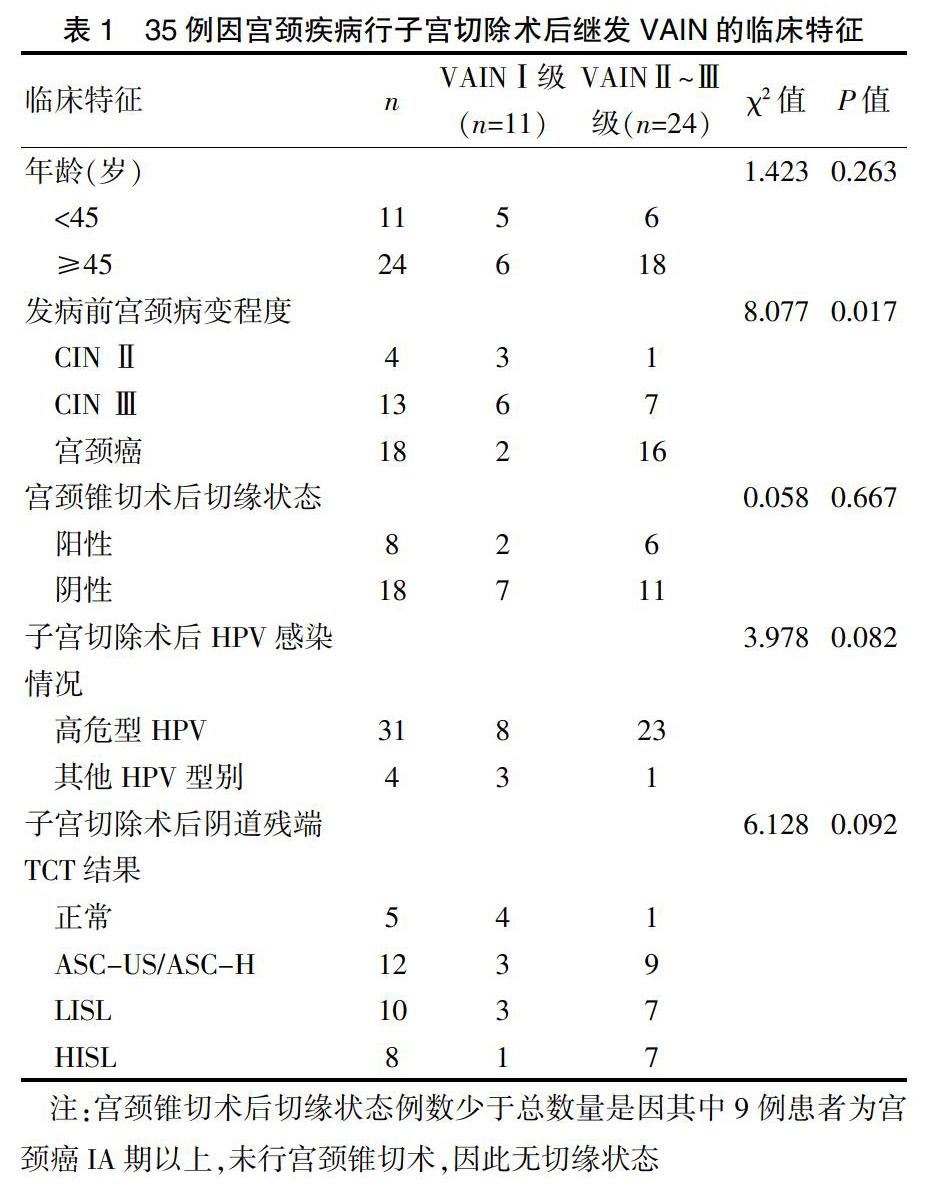
[摘要] 目的 探討因宫颈疾病行手术治疗后继发阴道上皮内肿瘤(Vaginal intraepithelial neoplasia,VAIN)的临床特征及相关风险因素。 方法 选取2010年1月~2018年12月间因宫颈疾病行手术治疗后继发VAIN的患者共35例,分析VAIN的发生与患者年龄、宫颈病变严重程度、宫颈锥切术后切缘情况、子宫切除术后HPV感染情况及TCT结果的相关性,并观察VAIN的发生时间及预后结局。 结果 随着宫颈疾病严重程度的升高,VAIN的发生率明显升高,且VAINⅡ~Ⅲ级患者既往宫颈病变的严重程度高于VAINⅠ级患者,差异有统计学意义(P=0.017)。VAIN患者人乳头瘤病毒(Human papillomavirus,HPV)感染发生率为100.0%,其中高危型HPV感染率为88.6%;且VAINⅡ~Ⅲ级患者的高危型HPV感染率略高于VAINⅠ级患者的高危型HPV感染率,但差异无统计学意义(P=0.082)。VAIN大多发生在子宫切除术后5年内,占80%;VAINⅠ级患者治疗后有4例持续存在,其中1例进展为VAINⅡ~Ⅲ级;VAINⅡ~Ⅲ级患者治疗后有5例复发,其中2例进展为阴道鳞状上皮癌,复发及进展患者均存在高危型HPV持续感染。 结论 宫颈疾病行子宫切除术后继发VAIN的发病与HPV感染及宫颈病变程度密切相关,对存在以上因素的患者在行子宫切除术时应予以重视,建议术前阴道壁组织活检术明确,以切除病变阴道壁组织减少VAIN的发生,术后需密切随访监测以早期发现阴道病变并及时治疗。
[关键词] 阴道上皮内肿瘤;宫颈上皮内肿瘤;宫颈肿瘤;人乳头瘤病毒
[中图分类号] R737.3 [文献标识码] B [文章编号] 1673-9701(2020)31-0069-05
[Abstract] Objective To explore the clinical features and related risk factors of vaginal intraepithelial neoplasia (VAIN) secondary to cervical diseases after surgical treatment. Methods A total of 35 patients with VAIN secondary to cervical diseases after surgical were collected. The correlation between VAIN occurrence and patients′ age, severity of cervical lesions,cutting edge after cervical conization, Human papillomavirus(HPV) infection after hysterectomy and TCT results were analyzed, and the occurrence time and prognosis of VAIN were observed. Results With the increase of the severity of cervical diseases, the incidence of VAIN increased significantly, and the severity of previous cervical lesions in VAIN grade Ⅱ-Ⅲ patients was higher than that in VAIN grade I patients, with statistically significant difference(P=0.017). The incidence of HPV infection in VAIN patients was 100%,in which the infection rate of high-risk HPV was 88.6%. Furthermore, the high-risk HPV infection rate of VAIN grade Ⅱ-Ⅲ patients was slightly higher than that of VAIN grade I patients, but the difference was not statistically significant(P=0.082).VAIN mostly occurred within 5 years after hysterectomy, accounting for 80%. After treatment, 4 patients with VAIN grade I persisted, and 1 patient progressed to VAIN grade Ⅱ-Ⅲ. After treatment, 5 patients with VAIN grade Ⅱ-Ⅲ relapsed, among which 2 patients advanced to vaginal squamous cell carcinoma.Both relapsed and advanced patients had high-risk HPV persistent infection. Conclusion The incidence of VAIN secondary to cervical diseases after hysterectomy is closely related to HPV infection and the degree of cervical lesions. Attention should be paid to patients with the above factors when undergoing hysterectomy. It is suggested that biopsy of vaginal wall should be clear before operation so as to cut off the diseased vaginal wall tissue and reduce the occurrence of VAIN. Close follow-up monitoring after surgery is needed to find vaginal lesions early and treat them in time.
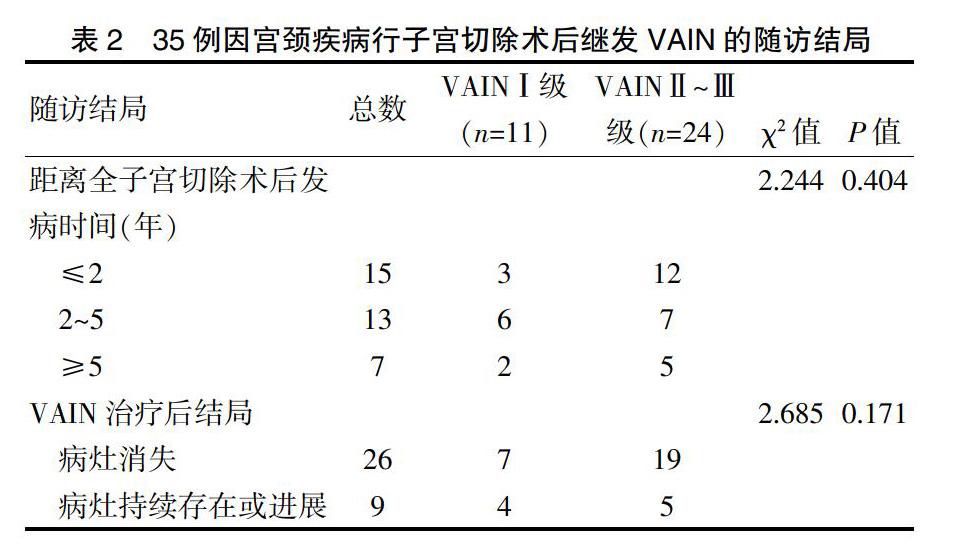
2.2 VAIN患者结局分析
从全子宫或广泛全子宫切除术至诊断为VAIN的时间为7~81个月不等,平均为28.00个月,大部分患者在术后的2年及2~5年發病,占80%,见表2。35例VAIN患者诊断后随访截止时间2019年12月31日,随访时间11~73个月,中位随访45个月,11例VAINⅠ级患者经过干扰素治疗后7例病灶消失,4例病灶持续存在,其中1例进展为VAINⅡ~Ⅲ级后行阴道局部病灶切除术后病灶消失,24例VAINⅡ~Ⅲ级有8例行激光治疗,其余16例行阴道病灶切除术,在随访过程中19例无再发VAIN,5例出现复发,其中2例进展为阴道鳞状上皮癌,见表2。同时发现在所有VAIN患者随访过程中,病灶持续存在或再发及进展的患者均存在高危型HPV阳性,其中主要以HPV16阳性为主,占75%。
3 讨论
近年来,由于宫颈病变的细胞学、病毒学及阴道镜检查等筛查手段的广泛应用,阴道上皮内瘤变的检出率也呈逐年上升趋势[8]。VAIN的发病原因目前认为与宫颈病变具有同源性,即与HPV感染有很大关系[9-10]。有关VAIN的起源有两种观点:其一,VAIN的发生独立于宫颈病变,VAIN往往呈多灶性,与宫颈不连续[11];其二,VAIN并非子宫切除术后新发残端VAIN所致,而是由于未引起临床重视,导致手术切除范围不足或病变迁延所致[12]。既往有CIN或浸润性宫颈癌病史被认为是VAIN发生的重要发病风险因素[13]。Vinokurova等[14]检测了既往患有CIN或宫颈癌的VAIN患者的HPV类型及整合位点,通过使用HPV DNA整合位点作为克隆性标记,结果显示VAIN患者的HPV类型及整合位点与既往CIN或宫颈癌的发病模式一致,推测这些病变可能是同一克隆起源而来[14],且研究显示,继发于宫颈病变的VAIN往往病灶主要位于阴道上段[13],因此,基于以上观点,有研究者提出在因宫颈病变行全子宫或广泛全子宫切除术前有必要对患者阴道壁进行充分评估,尤其是阴道上段,必要时需行阴道壁活检明确诊断。He等[15]的一项研究发现,随着子宫颈病变程度的增加(从子宫颈癌前病变到子宫颈癌),合并VAIN的比例及VAIN的级别均增高,且术前未行阴道镜阴道壁活检的患者发生VAIN的比例显著增高,因此建议对于Ⅰ期子宫颈癌或CINⅢ行子宫切除术的所有患者,术前均应常规进行阴道镜下全面阴道壁活检病理检查以明确阴道病变范围,尤其是阴道上段,从而更好地指导手术中阴道切除的范围,减少因手术范围不足导致VAIN的残留[15]。除了手术因素外,HPV感染尤其是高危型HPV持续感染被认为是宫颈疾病术后继发阴道及其他部位上皮内病变的重要因素,这些患者往往存在清除HPV感染的能力下降,因此术后长期处于持续HPV感染状态,从而继发其他部位HPV感染相关疾病的发生[16-17]。本研究中,所有VAIN患者均存在HPV感染,且大部分患者为高危型HPV持续感染,随着宫颈病变程度的增加,继发VAIN的发生比例显著升高,因此认为高危型HPV感染及子宫切除术前宫颈病变程度可能与VAIN的发病风险密切相关,对于存在以上高危因素的患者应引起重视,特别是在因CINⅡ~Ⅲ行锥切术后时隔1~3个月待宫旁炎性增生消退再行子宫切除术时,术前有必要再次对阴道壁情况进行评估,必要时进行醋酸及碘试验染色后阴道镜下全面阴道壁活检以明确诊断,如活检结果提示同时合并阴道壁病变应在全子宫或广泛全子宫切除术时注意阴道壁的切除范围,尽可能多切除一部分阴道壁,以减少VAIN的发生及残留。
鉴于宫颈疾病与VAIN发病的同源性,且术后持续高危型HPV感染被认为是VAIN的重要发病因素之一,术后密切随访在宫颈疾病行手术治疗后具有重要作用[18-19]。已有的文献报道,宫颈病变行子宫切除术后VAIN的发病大部分在子宫切除术后5年内,尤其是术后2年内最易发病[4,20]。本研究统计结果显示,42.9%的患者在子宫切除术后2年内诊断为VAIN病变,37.1%的患者在术后2~5年内诊断为VAIN病变,术后5年内发病占80%,因此,对于宫颈病变行子宫切除术后的患者,建议进行密切随访至5年,排除高危因素后再转为常规筛查。有研究通过多因素分析发现,HPV感染是VAIN发生和预后的独立危险因素[4,10],持续高危型HPV感染被认为是发展成高级别VAIN的必要条件。因此,有学者提出术后随访过程中高危型HPV检测的重要性,其对于残端VAIN的诊断及预测有指导意义[21],也可以验证TCT筛查的准确性,可与TCT联合作为残端VAIN筛查及诊断的手段,尤其是既往有高危型HPV感染患者,可提高筛查及诊断的敏感度和特异度。本研究结果显示,术后发生VAIN的患者HPV感染率为100%,且高危型HPV感染阳性率占88.6%,而TCT的检查异常率为85%,因此认为对于术后随访过程中存在HPV持续阳性尤其是高危型HPV持续阳性的患者无论TCT检测结果如何,建议尽早行阴道镜阴道壁组织活检以明确诊断,以利于早期发现VAIN并给予及时治疗。此外,本研究显示,在VAIN持续存在及进展的患者中,其HPV感染主要以高危型HPV16阳性多见,与Bertoli等[17]的报道基本一致,持续HPV16感染可能是VAIN预后不良的因素,后期有待于更大样本的数据做进一步研究证实。
综上所述,因宫颈病变行全子宫切除术后需警惕阴道上皮内瘤变的发生,对于宫颈病变程度越重及存在持续高危型HPV感染的患者应引起重视,在行子宫全切术前应仔细检查阴道壁有无病变,以减少因手术残留所致的VAIN的发生,术后需密切随访至5年,对于术后HPV持续阳性或TCT异常的患者及时行阴道镜下阴道壁全面活检明确以尽早发现病变并进行早期处理,降低漏诊率及恶变率,对于VINA患者持续存在高危型HPV感染尤其是HPV16型,应尽早明确诊断及治疗,减少疾病进展的发生。
[参考文献]
[1] Field A,Bhagat N,Clark S,et al. Vaginal intraepithelial neoplasia:A retrospective study of treatment and outcomes among a cohort of UK women[J].J Low Genit Tract Dis,2020,24(1):43-47.
[2] He Y,Zhao Q,Geng Y,et al. Clinical analysis of cervical intraepithelial neoplasia with vaginal intraepithelial neoplasia[J].Medicine,2017,96(17):e6700.
[3] Liang Y,Chen M,Qin L,et al. A meta-analysis of the relationship between vaginal microecology,human papillomavirus infection and cervical intraepithelial neoplasia[J].Infect Agent Cancer,2019,14:29.
[4] Alfonzo E,Holmberg E,Sparen P,et al. Risk of vaginal cancer among hysterectomised women with cervical intraepithelial neoplasia:A population-based national cohort study[J].BJOG,2020,127(4):448-454.
[5] Mclaren J,Naguib N,Babarinsa I,et al. Outcome of vaginal intraepithelial neoplasia following hysterectomy for cervical intraepithelial neoplasia-vaginal cancer is rare[J].Int J Gynecol Cancer,2015,251(9):1664.
[6] Wang Y,Kong W,Wu Y,et al. Therapeutic effect of laser vaporization for vaginal intraepithelial neoplasia following hysterectomy due to premalignant and malignant lesions[J].J Obstet Gynaecol Re,2014,40(6):1740-1747.
[7] Schockaert S,Poppe W,Arbyn M,et al. Incidence of vaginal intraepithelial neoplasia After hysterectomy for cervical intraepithelial neoplasia: A retrospective study[J].Obstet Gynecol Surv,2008,63(11):701-702.
[8] Chen L,Hu D,Xu S,et al. Clinical features,treatment and outcomes of vaginal intraepithelial neoplasia in a Chinese tertiary centre[J]. Irish J Med Sci,2016,185(1):111-114.
[9] Alemany L,Saunier M,Tinoco L,et al. Large contribution of human papillomavirus in vaginal neoplastic lesions:A worldwide study in 597 samples[J]. European Journal Of Cancer,2014,50(16):2846-2854.
[10] Ebisch R,Rutten D,Inthout J,et al. Long-lasting increased risk of human papillomavirus-related carcinomas and premalignancies after cervical intraepithelial neoplasia grade 3:A population-based cohort study[J]. J Clin Oncol, 2017, 35(22):2542-2550.
[11] Cong Q,Song Y,Wang Q,et al. A retrospective study of cytology,high-risk HPV, and colposcopy results of vaginal intraepithelial neoplasia patients[J]. Biomed Res Int,2018,2018:5 894 801.
[12] 叢青,汪清,高蜀君,等. 2013-2015年阴道镜下阴道上皮内瘤变检出率的变化趋势[J]. 中华妇产科杂志,2017, (4):239-243.
[13] Kim MK,Lee IH,Lee KH. Clinical outcomes and risk of recurrence among patients with vaginal intraepithelial neoplasia:A comprehensive analysis of 576 cases[J]. J Gynecol Oncol,2018,29(1):e6.
[14] Vinokurova S,Wentzensen N,Einenkel J,et al.Clonal history of papillomavirus-induced dysplasia in the female lower genital tract[J]. J Natl Cancer Inst,2005,97(24):1816-1821.
[15] He Y,Wu Y,Zhao Q,et al. Clinical analysis of patients underwent hysterectomy for stage I cervical cancer or high grade cervical intraepithelial neoplasia with vaginal intraepithelial neoplasia[J]. Zhonghua Fu Chan Ke Za Zhi,2015,50(7):516-521.
[16] Bogani G,Martinelli F,Ditto A,et al. Human papillomavirus (HPV) persistence and HPV 31 predict the risk of recurrence in high-grade vaginal intraepithelial neoplasia[J].Eur J Obstet Gynecol Reprod Biol,2017,210:157-165.
[17] Bertoli HK,Thomsen LT,Iftner T,et al. Risk of vulvar, vaginal and anal high-grade intraepithelial neoplasia and cancer according to cervical human papillomavirus (HPV) status:A population-based prospective cohort study[J].Gynecol Oncol,2020,157(2):456-462.
[18] Hodeib M,Cohen JG,Mehta S,et al. Recurrence and risk of progression to lower genital tract malignancy in women with high grade VAIN[J]. Gynecol Oncol,2016,141(3):507-510.
[19] Buchanan TR,Zamorano AS,Massad LS,et al. Risk of cervical and vaginal dysplasia after surgery for vulvar intraepithelial neoplasia or cancer:A 6 year follow-up study[J]. Gynecol Oncol,2019,155(1):88-92.
[20] Li H, Guo Y, Zhang J, et al. Risk factors for the development of vaginal intraepithelial neoplasia[J]. Chinese Medical Journal,2012,125(7):1219-1223.
[21] Bertoli HK, Rasmussen CL, Sand FL, et al. Human papillomavirus and p16 in squamous cell carcinoma and intraepithelial neoplasia of the vagina[J]. Int J Cancer,2019, 145(1):78-86.
(收稿日期:2020-05-11)
