甲强龙和地塞米松预防剖宫产术后恶心呕吐的疗效对比分析
2017-07-31李棽丽段力仁朱美琳董有静
李棽丽,段力仁,李 洋,朱美琳,董有静*
甲强龙和地塞米松预防剖宫产术后恶心呕吐的疗效对比分析
李棽丽1,段力仁2,李 洋1,朱美琳1,董有静1*
目的 比较甲强龙和地塞米松预防剖宫产术后恶心呕吐的临床疗效。方法 择期剖宫产手术患者135例,按照随机数字表将患者随机分为3组,每组45例。M组:术毕静注甲强龙40 mg(2 mL);D组:术毕静注地塞米松8 mg(2 mL);N组:术毕静注生理盐水(2 mL)。观察术后24 h内恶心呕吐及救援止吐的情况。结果 术后24 h内M组、D组、N组的PONV发生率分别为30.2%、34.9%、61.4%,M组、D组明显低于N组(P<0.05),但M组与D组之间差异无统计学意义(P>0.05),M组、D组、N组术后救援止吐率分别为9.3%、11.6%、34.1%,M组、D组明显低于N组(P<0.05),但M组与D组之间差异无统计学意义(P>0.05)。结论 甲强龙、地塞米松单独使用均能有效预防剖宫产术后恶心呕吐的发生率,降低术后救援止吐率。
甲强龙;地塞米松;恶心;呕吐;剖宫产
0 引言
术后恶心呕吐(Postoperative nausea and vomiting,PONV)是术后最常见的并发症之一,在住院手术患者中的发生率约为20%~37%,产妇发生PONV的风险高达60%[1]。恶心呕吐不仅可以导致患者身体不适,严重时还可以引起伤口裂开,影响患者术后恢复,延长住院时间,如何减少PONV的发生率是麻醉医师研究的重点。
有研究显示,地塞米松可以有效预防PONV的发生[2],如给予腹腔镜切除胆囊患者单次静注8 mg可明显减少恶心呕吐的发生。甲强龙作为人工合成的糖皮质激素,代谢较快,对肾上腺功能影响较小,但是目前关于甲强龙预防PONV的报道较少。本研究旨在比较甲强龙与地塞米松预防PONV的作用,为临床预防PONV提供参考。
1 材料与方法
1.1 一般资料 本研究已获得中国医科大学附属盛京医院伦理委员会批准(伦理编号:2016PS282K),并与患者或家属签署知情同意书。选择我院2015年12月至2016年6月择期行剖宫产手术患者135例,ASA Ⅰ或Ⅱ级,年龄20~35岁,体重65~90 kg,排除标准:严重高血压病史,心、肺、肝、肾、胃肠道病史,有引起恶心呕吐的基础疾病病史,糖尿病病史,自身免疫性疾病病史及糖皮质激素应用史,麻醉药物过敏史,吸烟史。按照随机数表法将135例患者随机分为3组,每组45例。随机数字放置于密封的信封中,在手术当天连续打开信封,实验药物配制由独立的麻醉医师制备,所有液体均透明且外观相同,对各实验组注射器外部进行掩蔽,患者与手术麻醉医师均不清楚参与组别,实验结果由独立护士收集。
1.2 研究方法 所有患者均术前禁食水8 h,不使用术前药物。患者入手术室后,监测ECG、NBP、HR、SpO2,建立静脉通路,于麻醉开始前静脉预输注乳酸林格氏液500 mL。行腰硬联合麻醉,穿刺部位选择L3-4间隙,蛛网膜下腔注入0.5%布比卡因1.1~1.5 mL,向头侧置管3 cm,麻醉平面控制在T4。胎儿娩出后,静脉输注缩宫素20 U。当术中血压下降超过基础值的20%时,静注10 mg麻黄碱予以纠正。术中全程2 L/min低流量吸氧。关闭腹膜时,患者均硬膜外给予吗啡2 mg。术毕,M组患者静注甲强龙40 mg(2 mL),D组患者静注地塞米松8 mg(2 mL),N组患者静注2 mL生理盐水,其中M组术后随访退出2例,D组随访退出2例,N组随访退出1例,最后各组纳入研究的患者为43例、43例、44例。
1.3 观察指标 记录麻醉诱导后1、5、10 min及手术结束时的BP、HR、SpO2;记录手术时间;记录术后24 h内恶心呕吐的发生及其分级情况(0级:无恶心呕吐;Ⅰ级:有恶心,无呕吐;Ⅱ级:恶心伴有1~2次呕吐;Ⅲ级:3次以上恶心呕吐),记录术后止吐救援的情况以及皮肤瘙痒情况。

2 结果
2.1 三组患者一般情况比较 三组患者年龄、体重、手术时间、麻醉时间和术中出血量比较,差异无统计学意义(P>0.05),见表1。

表1 三组患者一般情况比较
2.2 三组患者术后24 h恶心呕吐及救援止吐情况比较 术后24 h内,M组、D组发生PONV例数明显少于N组,差异有统计学意义(P<0.05),但M组与D组之间差异无统计学意义(P>0.05)。M组、D组需要救援止吐例数明显少于N组(P<0.05),但M组与D组之间差异无统计学意义(P>0.05)。见表2。
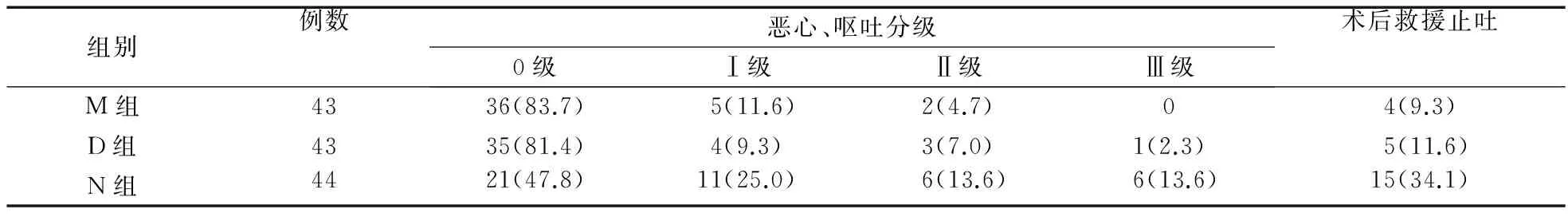
表2 三组患者术后24 h恶心呕吐及救援止吐情况比较(例,%)
2.3 三组患者术后24 h内皮肤瘙痒情况比较 术后24 h内M组、D组、N组分别有6例(14.0%)、7例(16.3%)、9例(20.4%)发生皮肤瘙痒,三组之间比较差异无统计学意义(P>0.05)。三组患者均无其他相关不良反应发生。
3 讨论
PONV是手术和麻醉后常见的并发症之一,主要发生于术后24~48 h内,术后长时间或者严重的PONV不仅引起患者身体不适,还会造成患者水电解质紊乱、切口裂开及切口疝形成、吸入性肺炎,延长患者住院时间,增加患者经济负担。产妇作为高危人群,其PONV发生率高达60%[1],因此,如何减少剖宫产术后产妇的恶心呕吐,具有非常重要的临床意义。
PONV的危险因素较多,包括女性、不吸烟、PONV史或者晕动史、术后阿片类药物应用,高风险患者术后发生率为70%~80%。PONV的神经中枢位于延髓的网状结构和孤束核,外界因素通过5羟色胺(5-HT)、P物质、多巴胺、乙酰胆碱等递质刺激外周感受器和呕吐中枢引起恶心呕吐,其中5-HT是PONV中最重要的递质[3-4]。在剖宫产手术中,产妇取仰卧位造成回心血流量减少,血压下降,手术牵拉刺激引起胃十二指肠肌肉收缩,食管下括约肌松弛,胃内容物反流至口腔,另外,阿片类药物的应用也使产妇更易发生PONV。吗啡是缓解术后疼痛的常用阿片类药物,其易引起PONV的机制可能为直接作用于中枢催吐化学感受区,兴奋延髓呕吐中枢,同时促进组胺释放,降低血容量,降低呼吸中枢对二氧化碳的敏感性,从而抑制呼吸,另外,减慢胃肠蠕动、延缓排空也诱发呕吐,吗啡的多重作用引起患者PONV,甚至嗜睡、呼吸抑制[5]。
临床上采用多巴胺受体拮抗剂、抗胆碱药、抗组胺药物预防PONV,但是引起的锥体外系反应、心律失常、低血压等不良反应限制了其临床应用。最近研究发现,围手术期应用地塞米松可以预防PONV[6-7],但其作用机制尚不清楚,可能是通过抑制中枢和外周5-HT3的产生与释放,降低中枢神经系统中5-HT3的浓度,同时阻止外周的5-HT3与受体结合,拮抗前列腺素,释放内啡肽,从而发挥抗恶心呕吐的作用[8]。此外,也可以通过敏化止吐药受体来增强止吐药作用[9]。也有研究发现,术后疼痛程度与PONV发生相关,糖皮质激素通过促进缓激肽降解[10],降低疼痛介质产生,从而发挥镇痛作用,降低PONV的发生,同时,应用糖皮质激素可以减少阿片类药物用量,降低阿片类药物引起的PONV[11-13]。
甲强龙,又称甲泼尼龙琥珀酸钠,是一种人工合成的中效糖皮质激素。甲强龙的药代动力学呈线性,不受给药途径的影响,其亲脂性强,可快速到达靶部位,达到平均峰血药浓度[14-16]。甲强龙与地塞米松的效价比为4∶0.75,0.75 mg地塞米松的药效相当于4 mg甲强龙,即本实验中40 mg甲强龙约与8 mg地塞米松效能相当[17]。本研究表明,与对照组相比,术毕单次静脉注射甲强龙40 mg或者地塞米松8 mg,均可有效降低剖宫产术后产妇的恶心呕吐,M组与D组术后恶心呕吐发生率比较差异无统计学意义。与对照组相比,应用地塞米松或甲强龙可以减少术后救援止吐药的应用。关于应用地塞米松可以降低PONV发生率已有相关报道[18-21],但因其会导致术后继发性肾上腺功能不足,使其应用的安全性受到质疑[22]。与地塞米松相比,甲强龙渗透性更强,半衰期短,对肌肉及下丘脑-垂体-肾上腺轴的抑制作用小于地塞米松[23],具有更高的安全性。
综上所述,本研究表明,围手术期应用甲强龙代替地塞米松可以降低PONV的发生率,提高患者围术期安全性及术后的舒适度,是一种更安全有效的方法。但关于甲强龙预防PONV的最适剂量与时机需要进一步临床试验验证。
[1] Jain R,Sharma R.A comparative study of effects of glycopyrrolate and ondansetron on nausea and vomiting in cesarean section under spinal anesthesia[J].Anesth Essays Res,2015,9(3):348-352.
[2] Viriyaroj V,Boonsinsukh T,Rookkachart T,et al.The effects of single-dose preoperative intravenous dexamethasone on clinical outcome after laparoscopic cholecystectomy[J].J Med Assoc Thai,2015,98(Suppl 10):S112-S117.
[3] Wakasugi M,Tori M,Shimizu J,et al.Efficacy of preoperative dexamethasone for postoperative nausea and vomiting after laparoscopic cholecystectomy:a large-scale,multicenter,randomized,double-blind,placebo-controlled trial in Japan[J].J Hepatobiliary Pancreat Sci,2015,22(11):802-809.
[4] Sinha R,Shende D,Maitra S,et al.Granisetron versus granisetron-dexamethasone for prevention of postoperative nausea and vomiting in pediatric strabismus surgery:a randomized double-blind trial[J].Anesthesiol Res Pract,2016,2016:4281719.
[5] Dale R,Edwards J,Ballantyne J.Opioid risk assessment in palliative medicine[J].J Community Support Oncol,2016,14(3):94-100.
[6] Yang XY,Xiao J,Chen YH,et al.Dexamethasone alone vs in combination with transcutaneous electrical acupoint stimulation or tropisetron for prevention of postoperative nausea and vomiting in gynaecological patients undergoing laparoscopic surgery[J].Br J Anaesth,2015,115(6):883-889.
[7] Sharma AN,Shankaranarayana P.Postoperative nausea and vomiting:palonosetron with dexamethasone vs.ondansetron with dexamethasone in laparoscopic hysterectomies[J].Oman Med J,2015,30(4):252-256.
[8] Sun S,Schaller J,Placek J,et al.Compatibility of intravenous fosaprepitant with intravenous 5-HT3 antagonists and corticosteroids[J].Cancer Chemother Pharmacol,2013,72(3):509-513.
[9] Steward DL,Grisel J,Meinzen-Derr J.Steroids for improving recovery following tonsillectomy in children[J].Cochrane Database Syst Rev,2011,(8):CD003997.
[10]Kim DR,Won H,Uhm JS,et al.Comparison of two different doses of single bolus steroid injection to prevent atrial fibrillation recurrence after radiofrequency catheter ablation[J].Yonsei Med J,2015,56(2):324-331.
[11]Lunn TH,Kristensen BB,Andersen L,et al.Effect of high-dose preoperative methylprednisolone on pain and recovery after total knee arthroplasty:a randomized,placebo-controlled trial[J].Br J Anaesth,2011,106(2):230-238.
[12]Vyas N,Agarwal S,Shah N,et al.Effect of single dose intramuscular methylprednisolone injection into the masseter muscle on the surgical extraction of impacted lower third molars:a randomized controlled trial[J].Kathmandu Univ Med J (KUMJ),2014,12(45):4-8.
[13]Christensen J,Matzen LH,Vaeth M,et al.Efficiency of bupivacaine versus lidocaine and methylprednisolone versus placebo to reduce postoperative pain and swelling after surgical removal of mandibular third molars:a randomized,double-blind,crossover clinical trial[J].J Oral Maxillofac Surg,2013,71(9):1490-1499.
[14]De la Motte L,Kehlet H,Vogt K,et al.Preoperative methylprednisolone enhances recovery after endovascular aortic repair:a randomized,double-blind,placebo-controlled clinical trial[J].Ann Surg,2014,260(3):540-549.
[15]Theroux MC,Fisher AO,Rodriguez ME,et al.Prophylactic methylprednisolone to reduce inflammation and improve outcomes from one lung ventilation in children:a randomized clinical trial[J].Paediatr Anaesth,2015,25:587-594.
[16]Gautam S,Agarwal A,Das PK,et al.Evaluation of the efficacy of methylprednisolone,etoricoxib and a combination of the two substances to attenuate postoperative pain and PONV in patients undergoing laparoscopic cholecystectomy:a prospective,randomized,Placebo-controlled trial[J].Korean J Pain,2014,27(3):278-284.
[17]Weren M,Demeere JL.Methylprednisolone vs.dexamethasone in the prevention of postoperative nausea and vomiting:a prospective,randomised,double-blind,placebo-controlled trial[J].Acta Anaesthesiol Belg,2008,59(1):1-5.
[18]Sayed JA,F Riad MA,M Ali MO.Comparison of dexamethasone or intravenous fluids or combination of both on postoperative nausea,vomiting and pain in pediatric strabismus surgery[J].J Clin Anesth,2016,34:136-142.
[19]嵇晓阳,瞿慧,鲁刚,等.甲强龙联合格拉司琼预防乳房肿块切除术后恶心呕吐[J].临床麻醉学杂志,2015,31(12):1196-1198.
[20]王武,吴多志.氟哌利多或托烷司琼复合地塞米松预防妇科腹腔镜术后恶心呕吐临床疗效[J].临床军医杂志,2016,44(7):752-753.
[21]郝帅,伍佳,罗超,等.帕洛诺司琼联合地塞米松对妇科腹腔镜手术术后恶心呕吐的预防效果[J].中国医药,2016,11(12):1828-1832.
[22]Bataille A,Letourneulx JF,Charmeau A,et al.Impact of a prophylactic combination of dexamethasone-ondansetron on postoperative nausea and vomiting in obese adult patients undergoing laparoscopic sleeve gastrectomy during closed-loop propofol-remifentanil anaesthesia:a randomised double-blind placebo-controlled study[J].Eur J Anaesthesiol,2016,33(12):898-905.
[23]Yu Q,Gao L,Gu MH,et al.Antiemetic effects of combined methylprednisolone and tropisetron in mastectomy[J].Minerva Anestesiol,2013,79(2):130-136.
Prophylactic effect of methylprednisolone and dexamethasone on postoperative nausea and vomiting after cesarean section
LI Shen-li1,DUAN Li-ren2,LI Yang1,ZHU Mei-lin1,DONG You-jing1*
(1.Department of Anesthesiology,Shengjing Hospital of China Medical University,Shenyang 110004,China;2. Department of Vascular Surgery,the First Affliated Hospital of China Medical University,Shenyang 110001,China)
Objective To compare the clinical efficacy of methylprednisolone and dexamethasone in the prevention of nausea and vomiting after cesarean section.Methods One hundred and thirty-five patients scheduled for cesarean section were randomly divided into three groups with 45 cases in each group.Group M:post operation intravenous injection of methylprednisolone 40 mg (2 mL);group D:postoperative intravenous injection of dexamethasone 8 mg (2 mL);group N:intravenous injection of postoperative saline (2 mL).The incidence of PONV and rescue antiemetic requirement within 24 h after operation were observed.Results The PONV incidences of group M,group D,and group N were 30.2%,34.9%,and 61.4%,group M and group D being significantly lower than that of group N (P<0.05),but there was no significant difference between group M and group D (P>0.05).The rescue antiemetic rate of group M,group D,and group N was 9.3%,11.6%,and 34.1%,group M and group D being significantly lower than that of group N (P<0.05),but there was no significant difference between group M and group D (P>0.05).Conclusion Methylprednisolone and dexamethasone alone can effectively prevent the nausea and vomiting after cesarean section and reduce the rate of postoperative antiemetic rescue.
Methylprednisolone;Dexamethasone;Nausea;Vomiting;Cesarean section
2017-01-04
1.中国医科大学附属盛京医院麻醉科,沈阳 110004;2.中国医科大学附属第一医院血管外科,沈阳 110001
辽宁省自然科学基金(2014021023)
10.14053/j.cnki.ppcr.201707007
*通信作者