高危儿听力筛查及随访研究①
2016-12-29吕攀攀董荣芝刘芳王娜娜徐冲锋邴卫卫耿立蒙
吕攀攀,董荣芝,刘芳,王娜娜,徐冲锋,邴卫卫,耿立蒙
高危儿听力筛查及随访研究①
吕攀攀,董荣芝,刘芳,王娜娜,徐冲锋,邴卫卫,耿立蒙
目的探索高危儿听力筛查情况及听力障碍的发生、变化及转归。方法2015年3月~2016年3月,采用耳声发射(OAE)、听性脑干反应(ABR)及脑干听觉诱发电位(BAEP)的方法,对336例高危儿分别于生后0~1、3、6、12个月进行听力监测。结果336例高危儿中,0~1个月内初检时29例未通过;3月龄复检时37例听力未通过;6月龄27例恢复正常;12月龄复检7例恢复正常,3例(0.89%)确诊耳聋。结论OAE、ABR结合BAEP检查高危儿听力损伤可获得较全面的诊断,连续听力监测可有效动态观察高危儿听力损伤的发生、变化及转归。
高危儿;听力筛查;耳声发射;听性脑干反应;脑干听觉诱发电位;随访
[本文著录格式]吕攀攀,董荣芝,刘芳,等.高危儿听力筛查及随访研究[J].中国康复理论与实践,2016,22(12):1459-1461.
CITED AS:LüPP,Dong RZ,Liu F,etal.Hearing screening and follow-up of high risk infant[J].Zhongguo Kangfu Lilun Yu Shijian, 2016,22(12):1459-1461.
新生儿及婴幼儿听力筛查在许多发达国家已成为常规制度[1-2],在我国发达地区也已列入常规。新生儿及婴幼儿听力筛查,特别是高危新生儿的听力追踪评估非常重要。国内外报道均显示,高危新生儿听力障碍的发生率为2%~4%,远高于正常新生儿,是听力损伤的高发人群[3-5]。高危儿听力障碍既可能是疾病本身所造成,也可能是由于出生后治疗引起。为探索本院就诊高危儿听力损伤情况,我们对2015年3月~2016年3月本院新生儿科及产科出院的高危新生儿进行连续听力监测,以进一步了解高危儿听力障碍的发生、变化及转归情况。
1 资料与方法
1.1 一般资料
收集本院新生儿科及产科2015年3月~2016年3月出院的新生儿,符合下列指征之一者均为监测对象:羊水异常;胎盘异常;妊娠期高血压;妊娠期糖尿病;足月小样儿;早产;低出生体质量;过期产;新生儿高胆红素血症;新生儿黄疸;新生儿缺氧缺血性脑病,符合韩玉昆等新生儿缺氧缺血性脑病诊断分度标准[6];新生儿肺炎。排除标准:先天性并发症;先天性畸形;其母孕期耳毒性药物使用史及肝肾疾病史;耳聋及其他遗传性疾病家庭史。符合指征作为检测对象的高危新生儿共336例。
1.2 方法
检查在听力筛查室由专门人员进行,采用耳声发射(otoacoustic em issions,OAE)、听性脑干反应(auditory brainstem response,AABR)及脑干听觉诱发电位(brainstem auditory evoked potential,BAEP)三种方法。OAE采用CD-RW Vser Cuide测定仪(丹麦),AABR使用MB11快速听性脑干反应测试仪(德国MAIKO)。BAEP使用丹迪全功能肌电诱发电位仪KEYPOINT(丹麦)。OAE用于出生后1个月内听力初筛,AABR用于复查,BAEP用于听力障碍患儿确诊。所有高危儿均在生后0~1、3、6、12个月各听力测查1次。
1.3 统计学分析
应用M icrosoft Excel2000进行数据录入和统计学分析。
2 结果
336例(672耳)1个月内筛查未通过者34耳,初筛未通过率5.06%,其中双耳未通过5例,未通过率1.49%。3个月AABR复查未通过者50耳,复查未通过率7.44%,其中双耳未通过13例,未通过率3.87%。6个月复查AABR和BAEP未通过者14耳,复查未通过率2.08%,其中双耳未通过4例,未通过率1.19%。12个月AABR和BAEP复查双耳未通过者3例,复查未通过率0.89%。说明本研究中听力损伤儿6个月后恢复正常,0.89%确诊耳聋患儿,转为耳鼻喉诊治。见表1。
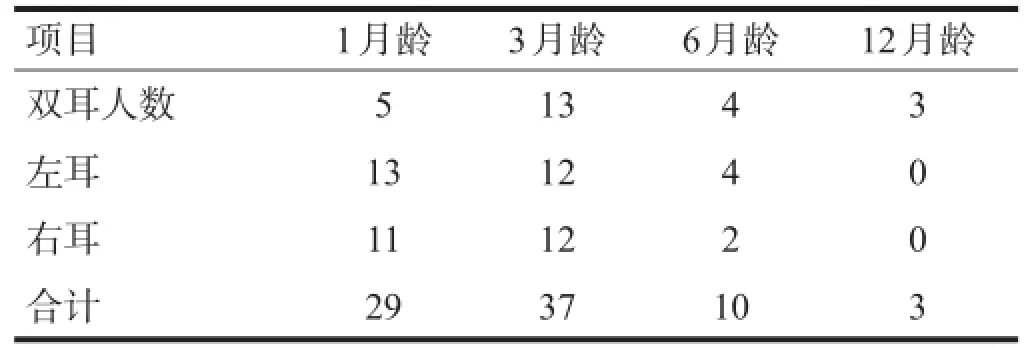
表1 高危儿听力筛查情况(n)
回顾分析高危因素,最后确诊听力障碍患儿3例中,1例为新生儿缺氧缺血性脑病,1例为早产低出生体质量,1例为高胆红素血症。
3 讨论
听力障碍是常见的出生缺陷。据国内外报道,高危新生儿听力障碍的发生率远高于正常新生儿[3-5]。正常新生儿中双侧听力障碍的发生率约0.1%~0.3%[7-8]。高危新生儿的听力障碍可能由宫内感染、低出生体质量、窒息、缺氧缺血性脑损伤、肺部疾病、颅内出血、高胆红素血症等疾病引起[9-11],特别是早产儿[12]。也存在遗传因素[13]。各种高危因素导致高危儿的听力损失多为中枢性的[14],临床上应用OAE、AABR及其他相关专业的检查如BAEP可以确诊[15-17],大部分损伤是可逆的[18-19]。但是有部分高危新生儿听力损伤具有获得性或进展性的特点,迟发型听力损伤的发病年龄最早可出现在8~12个月[20],最晚为4~5岁及以后[21-22],故对该人群听力进行定期听力监测和随访,显得尤为重要[23-24]。
国内报道正常新生儿听力障碍发生率为0.3%;经重症监护病房抢救的新生儿,听力障碍发生率高达22.6%[25]。本组高危儿最后确诊耳聋3例,发生率为0.89%,显示高危儿听力障碍发生率比正常新生儿高,但其听力损伤多为可逆性,故其最终耳聋发生率与正常新生儿基本一致。
本研究表明,应用OAE初筛有部分高危儿漏诊,复检采用AABR监测为阳性,进一步采用BAEP确诊,故采用OAE、AABR和BAEP可获得较全面的诊断。对出生时通过筛查的高危儿应提高警惕,因为他们亦有可能发生迟发性或获得性听力损伤,所以连续的听力检测尤为重要[26-27]。
及时发现,早期干预,可以改善患儿听力,刺激言语功能的发育,最终达到减少聋哑发病率的目的[28-30]。
高危儿听力损伤后有一段恢复期,不要过早下结论,造成家长思想负担过重,因为部分高危儿可恢复正常。本研究结果表明,通过实行听力监测可有效动态观察到高危儿听力障碍的发生、变化及转归,同时使有听力障碍高危儿及早得到干预,有效得到康复治疗,故建议在建立新生儿听力筛查同时,对高危儿要实施听力监测。
[1]Cavalcanti HG,Guerra RO.The role ofmaternal socioeconomic factors in the commitment to universal newborn hearing screening in the Northeastern region of Brazil[J].Int JPediatr Otorhinolaryngol,2012,76(11):1661-1667.
[2]Palmer SB,Bednarz SE,Dilaj KA,et al.Universal newborn hearing screening in m idw ifery education:a survey[J].JM idwiferyWomensHealth,2016,61(4):435-441.
[3]Erenberg A,Lemons J,Sia C,et al.Newborn and infant hearing loss:detection and intervention.American Academy of Pe-diatrics.Task Force on Newborn and Infant Hearing,1998-1999[J].Pediatrics,1999,103(2):527-530.
[4]Tanaka Y,Enomoto H,Takada K,et al.[Newborn Hearing Screening and Subsequent Diagnostic Evaluation:Analysis and Outcomes of 6,063 Infants Born in a Community Hospital][J].[in Japanese].Nihon Jibiinkoka Gakkai Kaiho,2016, 119(3):187-195.
[5]聂文英,宫露霞,刘玉俊,等.10501例新生儿听力筛查结果[J].中华医学杂志,2003,83(4):274-277.
[6]中华医学会儿科学会新生儿学组.新生儿缺氧缺血性脑病诊断依据和临床分度[J].中华儿科杂志,1997,35(2):99-100.
[7]Cubillana-Herrero JD,Pelegrin-Hernandez JP,Soler-Valcarcel A,et al.The assessment of the Newborn Hearing Screening Program in the Region of Murcia from 2004 to 2012[J].Int J Pediatr Otorhinolaryngol,2016,88:228-232.
[8]CavalcantiHG,Melo LP,Buarque LF,etal.Overview of newborn hearing screening programs in Brazilianmaternity hospitals[J].Braz JOtorhinolaryngol,2014,80(4):346-353.
[9]Barreira-Nielsen C,Fitzpatrick E,Hashem S,etal.Progressive hearing loss in early childhood[J].Ear Hear,2016,37(5): e311-e321.
[10]Colella-Santos MF,Hein TA,de Souza GL,et al.Newborn hearing screening and early diagnostic in the NICU [J]. Biomed Res Int,2014,2014:845308.
[11]Marlow ES,Hunt LP,Marlow N.Sensorineural hearing loss and prematurity[J].A rch Dis Child Fetal Neonatal Ed,2000, 82(2):F141-F144.
[12]Calcutt TL,Dornan D,Besw ick R,et al.Newborn hearing screening in Queensland 2009-2011:Comparison of hearing screening and diagnostic audiological assessment between term and preterm infants[J].J Paediatr Child Health, 2016.[Epub ahead of print]
[13]Lang-Roth R.Hearing impairment and language delay in infants:Diagnostics and genetics[J].GMSCurr Top OtorhinolaryngolHead Neck Surg,2014,13:c5.
[14]Mehl AL,Thomson V.The Colorado newborn hearing screening project,1992-1999:on the threshold of effective population-based universal newborn hearing screening[J].Pediatrics, 2002,109(1):E7.
[15]de Kock T,Swanepoel D,Hall JR.Newborn hearing screening at a community-based obstetric unit:Screening and diagnostic outcomes[J].Int J Pediatr Otorhinolaryngol,2016,84: 124-131.
[16]Khoza-Shangase K,Harbinson S.Evaluation of universalnewborn hearing screening in South African primary care[J].Afr J Prim Health Care Fam Med,2015,7(1).doi:10.4102/phcfm. v7i1.769.
[17]Kemaloglu YK,Gokdogan C,Gunduz B,etal.Newborn hearing screening outcomes during the first decade of the program in a reference hospital from Turkey[J].Eur Arch Otorhinolaryngol,2016,273(5):1143-1149.
[18]Mcgurgan IJ,Patil N.Neonatal hearing screening of high-risk infants using automated auditory brainstem response:a retrospective analysis of referral rates[J].Ir JMed Sci,2014,183 (3):405-410.
[19]van Dyk M,Swanepoel DW,Hall JR.Outcomes w ith OAE and AABR screening in the first 48 h-implications for newborn hearing screening in developing countries[J].Int JPediatr Otorhinolaryngol,2015,79(7):1034-1040.
[20]Caluraud S,Marcolla-Bouchetemble A,de Barros A,et al. Newborn hearing screening:analysis and outcomes after 100000 births in Upper-Normandy French region[J].Int JPediatrOtorhinolaryngol,2015,79(6):829-833.
[21]Stika CJ,Eisenberg LS,Johnson KC,et al.Developmental outcomes of early-identified children who are hard of hearing at 12 to 18 months of age[J].Early Hum Dev,2015,91(1): 47-55.
[22]Ching TY,Dillon H,Marnane V,etal.Outcomesof early-and late-identified children at 3 years of age:findings from a prospective population-based study[J].Ear Hear,2013,34(5): 535-552.
[23]A laee E,SiratiM,Taziki MH,et al.Risk factors for sensorineural hearing loss among high-risk infants in Golestan Province,Iran in 2010-2011[J].Iran Red CrescentMed J,2015,17 (12):e20419.
[24]Okano T,IwaiN,TaniguchiM,etal.[A clinicalstudy on 106 infant caseswho received detailed hearing tests after newborn hearing screening][J].[in Japanese].Nihon Jibiinkoka Gakkai Kaiho,2014,117(10):1249-1257.
[25]徐秀,王穗芬,彭咏梅,等.上海地区2378名新生儿听力筛查分析[J].中华儿科杂志,2006,35(1):571-573.
[26]Mann T,Cuttler K,Campbell C.Newborn hearing screens may give a false sense of security[J].JAm Acad Audiol,2001, 12(4):215-219,220-221.
[27]Hunter LL,Meinzen-Derr J,Wiley S,et al.Influence of the WICProgram on loss to follow-up fornewborn hearing screening[J].Pediatrics,2016,138(1).pii:e20154301.
[28]M ukherjee SS,M ukherjee S,Sarkar KD.Prevalence of hearing loss in high risk infants ofmediocre socio-economic background ataround one yearof ageand their correlation with risk factors[J].Indian J Otolaryngol Head Neck Surg,2013,65 (Suppl3):598-603.
[29]Finckh-Krämer U,GrossM,Bartsch M,etal.[Hearing screening of high risk newborn infants][J].[in German].HNO,2000, 48(3):215-220.
[30]沈晓明.新生儿听力筛查工作中需要重视的几个问题[J].中华医学杂志,2004,84(6):441.
Hearing Screening and Follow-up of High Risk Infant
LÜPan-pan,DONGRong-zhi,LIU Fang,WANGNa-na,XU Chong-feng,BINGWei-wei,GENG Li-meng
Departmentof Pediatrics,TheA ffiliated Hospitalof Binzhou MedicalUniversity,Binzhou,Shandong 256603,China
ObjectiveTo explore the hearing screening,and the change and outcome of hearing impairmentof high risk infants.MethodsFrom March,2015 to March,2016,336 high risk infantswere screened w ith otoacoustic emissions(OAE),auditory brainstem response (ABR)and brainstem auditory evoked-potential(BAEP)0-1,3,6,12months after born,respectively.ResultsAmong the 336 high risk infants,29 failed theexam inationsw ithin the1stmonth,37 cases failed in the3rdmonth,27 cases recovered in the9thmonth,and 7 cases recovered in the 12thmonth,3 caseswere finally diagnosed as deafness(0.89%).ConclusionOAE,ABR combining with BAEPexamination may obtain com prehensive diagnosis of hearing impairment for high risk infants,continuous listening com prehensionmonitoring can effectively dynam ically observe thehearing impairment,changesand outcomeof high risk infants.
high risk infants;hearing screening;otoacoustic emissions;auditory brainstem response;brainstem auditory-evoked potential;follow-up
10.3969/j.issn.1006-9771.2016.12.021
R246.81
B
1006-9771(2016)12-1459-03
2016-08-24
2016-09-05)
滨州市科技发展计划项目(No.2014ZC0155)。
滨州医学院附属医院儿科,山东滨州市256603。作者简介:吕攀攀(1985-),女,汉族,山东淄博市人,硕士,医师,主要研究方向:高危儿筛查及早期干预。E-mail:lvpanpan163@163.com。
