经微导管估测冠状动脉侧支血流状态的临床意义
2016-12-12沈迎丁风华张瑞岩杨震坤胡健沈卫峰
沈迎 丁风华 张瑞岩 杨震坤 胡健 沈卫峰
·临床研究·
经微导管估测冠状动脉侧支血流状态的临床意义
沈迎 丁风华 张瑞岩 杨震坤 胡健 沈卫峰
目的 验证经微导管测定冠状动脉闭塞远端压力(Pd)的精确性,并探讨该方法在评估冠状动脉侧支循环中的作用。方法 连续入选249例稳定型心绞痛伴至少一支冠状动脉完全闭塞3个月以上患者,于冠状动脉介入治疗时当导引钢丝通过闭塞病变后,应用微导管测定Pd,对其中40例(验证组)再用压力导丝进行压力测定。根据主动脉平均压和Pd计算冠状动脉侧支血流指数(collateral flow index,CFI)。结果 (1)经微导管测定的Pd与压力导丝测得值显著相关,组内相关系数为0.751(95%CI0.611~0.840,P<0.001);两种方法计算的CFI也显著相关,组内相关系数为0.679(95%CI0.391~ 0.830,P<0.001)。(2)Pd与主动脉收缩压、舒张压、平均压均显著相关(均P<0.001),但CFI仅与Pd相关(r=0.843,P<0.001),而与主动脉收缩压(r=-0.030)、舒张压(r=-0.051)和平均压(r=-0.057)无显著相关性(均P>0.05)。(3)女性、高龄(年龄≥70岁)、糖尿病、血脂异常、吸烟和肾功能减退患者Pd和CFI减低(均P<0.05),而高血压病患者Pd和CFI增高。结论 介入治疗时,应用微导管可以精确地测定Pd,这可能对评估冠状动脉侧支循环状态和冠心病患者治疗具有重要的临床价值。
冠心病; 慢性完全闭塞病变; 侧支循环; 经皮冠状动脉介入治疗
既往研究表明,良好的冠状动脉侧支循环为缺血高危心肌提供潜在的供血,有助于改善冠心病患者的心肌缺血程度、缩小心肌梗死范围、保护心功能、延长生存时间[1-3]。慢性闭塞病变即使侧支形成良好,血运重建仍然可能有益,因此,对完全闭塞的冠状动脉病变常常采用经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)[4-5]。临床医师在PCI术中常常应用各种导引钢丝结合微导管技术,以跨越慢性闭塞部位并提高PCI的成功率。既往在冠状动脉侧支循环生理学意义评估时,常需用压力导丝测定冠状动脉内压力[6],明显增加医疗费用。为此,本研究以压力导丝测定的冠状动脉闭塞远端压力(Pd)和冠状动脉侧支血流指数(collateral flow index,CFI)为基准,验证经微导管测定的相应参数的精确性,分析Pd与主动脉压及CFI的关系,探讨影响冠状动脉侧支循环的临床因素。
1 对象与方法
1.1 研究对象
连续入选249例稳定型心绞痛伴至少一支冠状动脉完全闭塞3个月以上患者。稳定型心绞痛诊断根据美国心脏病学会/美国心脏协会推荐的诊断标准[7]。记录患者的临床特征、冠心病危险因素、生化测定结果。依据心肌梗死发生日期、心绞痛突然加重或以往冠状动脉造影显示,判断冠状动脉闭塞的时间。排除标准:(1)最近3个月内接受PCI者;(2)以往接受冠状动脉旁路移植术(coronary artery bypass graft,CABG)者;(3)肾功能衰竭且需要血液透析者;(4)慢性心力衰竭、肺源性心脏病(肺心病)、恶性肿瘤、免疫系统疾病;(5)1型糖尿病。高血压定义为血压≥140/90 mmHg(1 mmHg=0.133 kPa)或需要应用药物治疗以控制血压[8]。根据美国糖尿病协会和国家胆固醇教育规划第三次报告标准诊断2型糖尿病和高脂血症[9-10]。
1.2 Pd和冠脉动脉CFI测定
所有患者接受经桡动脉入径冠状动脉造影,冠状动脉内径减小>70%为明显狭窄,1支以上血管伴明显狭窄时为多支病变。以常规方法行完全闭塞病变PCI。在指引导管到达冠状动脉开口后,首先将导引钢丝、微导管(Finecross,Terumo Co)成功通过冠状动脉闭塞处,同时自指引导管内注射少量对比剂以确认冠状动脉始终处于完全闭塞状态。将压力换能器置于腋中线,并接通大气调零点。然后,记录主动脉压和Pd。主动脉压经6 F指引导管测得(注意导管顶端远离冠状动脉开口,确保主动脉测压曲线正常,无阻尼)。Pd经微导管测得。根据公式计算CFI,即CFI=(Pd-CVP)/(Pa-CVP),其中Pa为主动脉平均压,CVP为中心静脉压。由于本研究所有患者均无临床心力衰竭症状或静脉压增高的表现,因此CVP假定为5 mmHg[11]。
为了验证经微导管测定Pd和CFI的正确性,对最初的40例患者(验证组)在微导管测定Pd后即刻,应用压力导丝(St Jude Medical,USA)进行Pd测定:(1)将压力导丝与主动脉压曲线两者校零并“等同”(equalizing)。(2)将压力导丝的探头插过微导管顶端并置于冠状动脉阻塞远端,同步记录主动脉压和Pd。
1.3 统计学分析
应用SPSS 23.0统计学软件进行数据分析。连续变量以均数±标准差表示,分类变量以频数(百分比)表示。用Kolmolgorov-Smirnov方法检验连续变量是否为正态分布。总体和验证组连续变量比较用t检验(正态分布)或Mann-WhitneyU检验(非正态分布),分类变量用卡方检验。用组内相关性分析、配对t检验和Bland-Altman方法,验证经微导管和压力导丝测定Pd和CFI相关性和差异程度。Pd与主动脉压的关系用线性回归分析。应用多因素线性逐步回归分析以决定Pd及CFI的独立影响因素。所有统计分析均用双侧检验,以P<0.05为差异有统计学意义。
2 结果
2.1 验证组和总体患者的一般资料比较
验证组(40例)和总体(249例)患者性别、年龄、体重指数等一般情况,高血压病、糖尿病、血脂异常和吸烟等冠心病危险因素,血压、血糖、血脂、肾功能、C反应蛋白和左心室射血分数等临床和生化指标,冠状动脉造影和用药情况等资料比较,差异均无统计学意义(均P>0.05,表1)。
2.2 经微导管测定Pd和CFI的精确性
经微导管测定的Pd与压力导丝测得值显著相关,组内相关系数为0.751(95%CI0.611~0.840,P<0.001,图1A),两者差值均数为1.68 mmHg(95%CI-1.42~4.77,P=0.280,图1B)。同样,两种方法计算的CFI也显著相关,组内相关系数为0.679(95%CI0.391~ 0.830,P<0.001,图1C),两者差值均数为0.019(95%CI-0.02~0.053,P=0.279,图1D)。
注:ACEI,血管紧张素转化酶抑制药;ARB,血管紧张素Ⅱ受体拮抗药;1 mmHg=0.133 kPa
2.3 Pd与主动脉压及冠状动脉CFI的关系
在249例患者中,主动脉收缩压、舒张压、平均压与CFI均呈正态分布。Pd与主动脉收缩压、舒张压、平均压均显著相关(均P<0.001,图2)。然而,CFI仅与Pd相关(r=0.843,P<0.001),而与主动脉收缩压(r=-0.030)、舒张压(r=-0.051)和平均压(r=-0.057)无显著相关性(均P>0.05)。
2.4 影响Pd和CFI的因素
在249例患者中,Pd为(47.16±13.34)mmHg,CFI为(0.45±0.12)。单因素分析显示,女性、高龄(年龄≥70岁)、糖尿病、血脂异常、吸烟和肾功能减退患者Pd和CFI减低(均P<0.05),而高血压病患者Pd和CFI增高(表2)。多因素分析显示,性别、年龄、高血压病、糖尿病、血脂异常、吸烟、估算的肾小球滤过率和C反应蛋白为Pd和CFI的独立影响因素(表3)。

Pd,冠状动脉闭塞远端压力;CFI,冠状动脉侧支血流指数;cath,微导管;wire,压力导丝;1 mmHg=0.133 kPa图1 经微导管和压力导丝测定Pd和CFI相关性和Bland-Altman分析 A.经微导管和压力导丝测定Pd的相关性;B.经微导管和压力导丝测定Pd的差值;C.经微导管和压力导丝测定CFI的相关性;D.经微导管和压力导丝测定CFI的差值

Pd,冠状动脉闭塞远端压力;1 mmHg=0.133 kPa图2 Pd与主动脉收缩压、舒张压和平均压的关系
3 讨论
近年来,尽管人们对冠状动脉侧支循环的重要性有了足够的认识,但至今尚缺乏评估侧支形成生理学意义的可靠方法。本研究首先对所有研究对象进行严格的选择,各例均存在冠状动脉慢性完全闭塞,这是因为冠状动脉完全闭塞是侧支形成的先决条件。而且,微导管在冠状动脉慢性完全闭塞病变介入治疗中应用已十分普遍,也为侧支循环的研究提供方便。
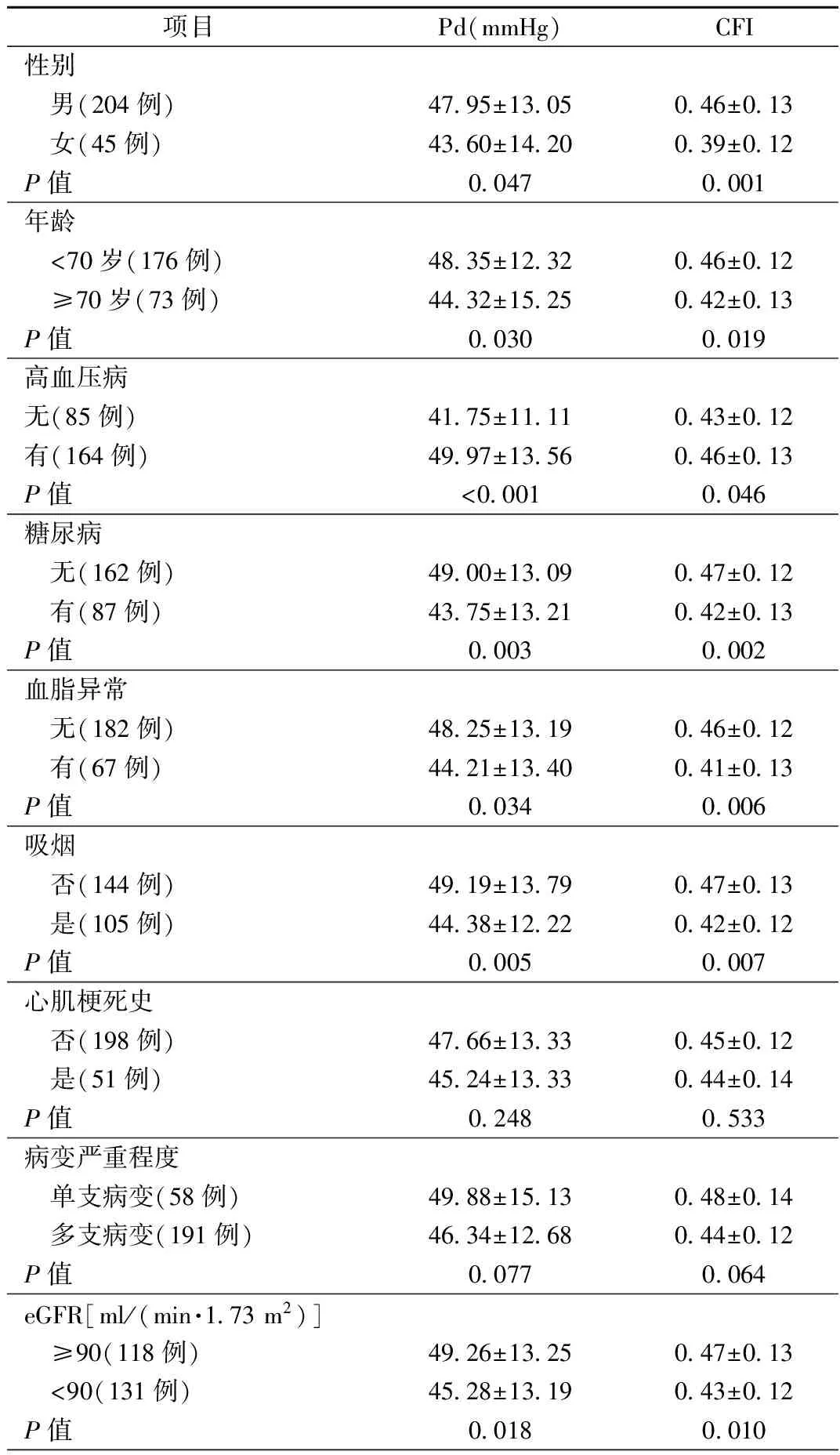
表2 各亚组Pd和CFI比较
注:eGFR,估算的肾小球滤过率;Pd,冠状动脉闭塞远端压力;CFI,冠状动脉侧支血流指数;1 mmHg=0.133 kPa
当前,大多数临床医师采用Rentrop记分法对冠状动脉侧支循环进行目测分级,尽管该方法简单,但其仅提供冠状动脉侧支循环的半定量评估,而且受到对比剂用量、注射速度以及采集图像的影响[12]。同样,冠状动脉造影本身产生灌注压和心肌需氧量的变化也影响冠状动脉侧支血流评估的精确性。理论上,冠状动脉内压力可以应用压力导丝测得,这些已在血流储备分数评估冠状动脉临界病变、指导PCI策略时广泛应用[13-14]。对冠状动脉慢性完全闭塞病变介入治疗时,尽管压力导丝可以很容易地经微导管插至闭塞远端冠状动脉,记录Pd并计算CFI,但该压力导丝价格昂贵,限制其临床上推广应用。本研究表明,应用微导管直接测得的Pd与压力导丝测得值以及两种方法结合主动脉测压推算的CFI显著相关,这些结果说明,经微导管测定Pd可为临床评估冠状动脉侧支循环提供一个简便的方法。
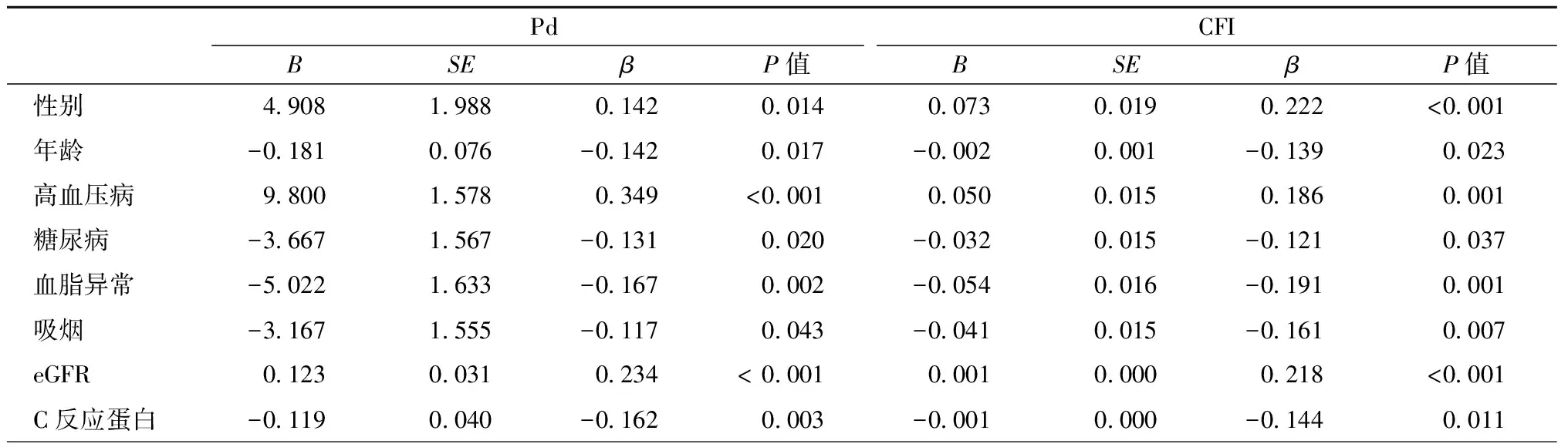
表3 Pd和CFI的多因素分析
注:eGFR,估算的肾小球滤过率;Pd,冠状动脉闭塞远端压力;CFI,冠状动脉侧支血流指数
冠状动脉侧支形成可能是心外膜冠状动脉与右心房(冠状窦)之间的压力阶差升高、冠状动脉阻力降低和侧支血管增大等综合作用的结果,被认为主要与动脉生成有关[6,15]。由于冠状动脉灌注主要发生于舒张期,因而舒张压被认为是提高侧支血流的重要因素[16]。然而,本研究显示冠状动脉完全闭塞时,尽管Pd与主动脉压存在一定的相关性,但CFI仅与Pd相关,而与主动脉压无关。这些提示,良好的侧支循环能维持较高的Pd。后者使切应力增大,激活内皮细胞表面的机械感受器,调节内皮一氧化氮合成,促进冠状动脉侧支发生和成熟[17-19]。
本研究显示,冠状动脉侧支形成受众多的临床、生化、炎症指标和血管造影因素的影响,这些发现与以往的报道相似[12,16,20-21]。老年、女性患者、吸烟、高脂血症等影响内皮细胞生长而使冠状动脉侧支形成不佳。糖尿病时,糖基化终末产物形成,并与其受体相互反应,导致弥漫性冠状动脉病变以及侧支循环形成适应性反应异常[22]。肾功能障碍(即使肾小球滤过率轻度减低)对某些侧支形成的必要因素(例如促新生血管生长因子、内皮细胞功能、冠状循环血流状态、细胞内信号、白细胞和骨髓源性内皮祖细胞等)产生不利影响[23-24]。同时,肾功能异常也可能通过增加胰岛素抵抗进一步加重糖尿病,进而导致冠状动脉侧支形成不佳。相反,高血压(特别是舒张压增高)在一定程度上作为一种代偿机制,有利于维持正常的冠状动脉侧支血流。但如果舒张压过低或过高,则可能降低冠状动脉侧支的灌注。这种舒张压与冠状动脉侧支形成之间的关系与以往报告的血压与心血管事件发生率呈现的J型关系是一致的[16,25]。
综上所述,经微导管测定Pd以及结合主动脉压推算CFI,是一种评价侧支循环的实用方法,可为冠状动脉慢性完全闭塞病变的病理生理提供进一步认识,可能对这些患者的治疗策略制定具有一定的临床价值。
[1] Steg PG, Kermer A, Mancini GB, et al. Impact of collateral flow to the occluded infarct-related artery on clinical outcomes in patients with recent myocardial infarction: a report from the randomized occluded artery trial. Circulation, 2010, 121(25):2724-2730.
[2] Meier P. The sword of Damocles: an illustrative example of the life-saving effect of the collateral circulation. J Invasive Cardiol, 2011, 23(3):E47-E48.
[3] Meier P, Hemingway H, Lansky AJ, et al. The impact of the coronary collateral circulation on mortality: a meta-analysis. Eur Heart J, 2012, 33(5):614-621.
[4] Khan MF, Wendel CS, Thai HM, et al. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes: a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv, 2013, 82(1):95-107.
[5] Sachdeva R, Agrawal M, Flynn SE, et al. The myocardium supplied by a chronic total occlusion is a persistently ischemic zone. Catheter Cardiovasc Interv, 2014, 83(1):9-16.
[6] Traupe T, Gloekler S, de Marchi SF, et al. Assessment of the human coronary collateral circulation. Circulation, 2010, 122(12):1210-1220.
[7] Fraker TD Jr, Fihn SD, Gibbons RJ, et al. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol, 2007, 50(23): 2264-2274.
[8] Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens, 2013, 31(7):1281-1357.
[9] Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care, 2003, 26(Suppl 1):S5-S20.
[10] Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel Ⅲ). JAMA, 2001, 285(19):2486-2497.
[11] van der Hoeven NW, Teunissen PF, Werner GS, et al. Clinical parameters associated with collateral development in patients with chronic total coronary occlusion. Heart, 2013, 99(15):1100-1105.
[12] Shen Y, Ding FH, Zhang RY, et al. Serum cystatin C reflects angiographic coronary collateralization in stable coronary artery disease patients with chronic total occlusion. PLoS One, 2015, 10(9):e0137253.
[13] Zhang D, Lv S, Song X, et al. Flow fractional reserve versus angiography for guiding percutaneous coronary intervention. Heart, 2015, 101(6):455-462.
[14] 陈盈文, 胡允兆, 吴焱贤, 等. 血流储备分数在冠状动脉复杂病变经皮冠状动脉介入治疗中的应用. 中国介入心脏病学杂志,2015,23(6):320-325.
[15] Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med, 2000, 6(4):389-395.
[16] Shen Y, Ding FH, Wu F, et al. Association of blood pressure and coronary collateralization in type 2 diabetic and nondiabetic patients with stable angina and chronic total occlusion. J Hypertens, 2015, 33(3):621-626.
[17] Chou E, Suzuma I, Way KJ, et al. Decreased cardiac expression of vascular endothelial growth factor and its receptors in insulin-resistant and diabetic states: a possible explanation for impaired collateral formation in cardiac tissue. Circulation, 2002, 105(3):373-379.
[18] Cai WJ, Kocsis E, Luo X, et al. Expression of endothelial nitric oxide synthesis in the vascular wall during arteriogenesis. Mol Cell Biochem, 2004, 264(1-2):193-200.
[19] Galie PA, Nguyen DH, Choi CK, et al. Fluid shear stress threshold regulates angiogenic sprouting. Proc Natl Acad Sci U S A, 2014, 111(22): 7968-7973.
[20] Sun Z, Shen Y, Lu L, et al. Clinical and angiographic features associated with coronary collateralization in stable angina patients with chronic total occlusion. J Zhejiang Univ Sci B, 2013, 14(8):705-712.
[21] Shen Y, Lu L, Liu ZH, et al. Increased serum level of CTRP1 is associated with low coronary collateralization in stable angina patients with chronic total occlusion. Int J Cardiol, 2014, 174(1):203-206.
[22] Shen Y, Lu L, Ding FH, et al. Association of increased serum glycated albumin levels with low coronary collateralization in type 2 diabetic patients with stable angina and chronic total occlusion. Cardiovasc Diabetol, 2013, 12:165.
[23] Xie SL, Li HY, Deng BQ, et al. Poor coronary collateral vessel development in patients with mild to moderate renal insufficiency. Clin Res Cardiol, 2011, 100(3):227-233.
[24] Shen Y, Ding FH, Wu F, et al. Cystatin C versus creatinine- based definition of renal dysfunction for predicting poor coronary collateralization in type 2 diabetic patients with stable coronary artery disease. J Diabetes Metab, 2014, 5(11):453-459.
[25] Vamos EP, Harris M, Millett C, et al. Association of systolic and diastolic blood pressure and all cause mortality in patients newly diagnosed type 2 diabetes: retrospective cohort study. BMJ, 2012, 345:e5567.
Clinical significance of coronary collateral flow status assessment using microcatheters
SHEN Ying, DING Feng-hua, ZHANG Rui-yan, YANG Zhen-kun, HU Jian, SHEN Wei-feng.
Department of Cardiology, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai 200025, China
SHEN Wei-feng, Email: rjshenweifeng@126.com
Objective To evaluate the accuracy of measurement of mean intracoronary pressure distal to an occluded segment (Pd) using a microcatheter, and to assess the clinical significance of coronary collateral flow index (CFI) in patients with chronic total coronary occlusion (CTO). Methods A total of 249 consecutive patients undergoing percutaneous coronary intervention (PCI) for CTO (>3 months) were enrolled. Pd was measured via a microcatheter in all patients and was also determined using a pressure wire in the first 40 enrolled patients as the verified group. Aortic pressure was recorded through a 6F flow-filled guiding catheter, and CFI was then calculated. Results (1) Pd and CFI determined using a microcatheter correlated significantly with the results obtained from the pressure wire (r=0.751 andr=0.679, allP< 0.001). (2) Pd was closely related to aortic systolic, diastolic, and mean pressure, but CFI correlated only with Pd (r=0.843,P<0.001). (3) Old age (age≥70 years old), female gender, diabetes, smoking, hyperlipidemia and reduced renal function were associated with lower Pd and CFI (allP<0.05), whereas patients with hypertension had higher Pd and CFI. Conclusions During PCI for CTO, coronary collateral circulation may be accurately evaluated by measurement of Pd through a microcatheter and this tecknique shows significant usefullness in the assessment of colleteral circulation status.
Coronary artery disease; Chronic total occlusion; Collateral circulation; Percutaneous coronary intervention
10.3969/j.issn.1004-8812.2016.10.002
上海市科委项目(14ZR1425800);上海交通大学医工结合研究项目
200025 上海,上海交通大学医学院附属瑞金医院心脏科
沈卫峰,Email:rjshenweifeng@126.com
R541.4
2016-06-22)
