儿科早期预警系统评分对门诊急性呼吸道感染患儿分流及病情评估的价值
2016-10-19胡师东吴海珍麻丽丽胡晓光贾晓慧
胡师东 吴海珍 麻丽丽 胡晓光 贾晓慧▲
1.温州医科大学附属第二医院儿童呼吸科,浙江温州325027;2.浙江省温州市中西医结合医院ICU,浙江温州325000
儿科早期预警系统评分对门诊急性呼吸道感染患儿分流及病情评估的价值
胡师东1吴海珍2麻丽丽1胡晓光1贾晓慧1▲
1.温州医科大学附属第二医院儿童呼吸科,浙江温州325027;2.浙江省温州市中西医结合医院ICU,浙江温州325000
目的探讨儿科早期预警系统评分对门诊急性呼吸道感染患儿分流及病情评估的价值。方法本研究采用横断面调查,收集2015年5月1日~31日于在温州医科大学附属第二医院和温州市中西医结合医院呼吸科门诊就诊的急性呼吸道感染患儿资料,计算PEWS评分。比较住院及非住院患儿的PEWS评分,将住院患儿进一步按PEWS评分分为重症组与非重症组,比较两组之间患儿年龄、初诊至入院时间、住院费用及日平均费用等差异。结果研究期间共收集1954例患儿资料,大部分初诊患儿的PEWS评分≤2分,≥4分的患儿属于少数,入院患儿的PEWS评分高于非入院患儿。重症组与非重症组之间患儿年龄未见明显差异[90(69.5,150)vs 93(72.5,152),P= 0.750],重症组从初诊至入院的时间明显较非重症组短[0(0,0.5)vs 2(1,2),P<0.01],住院费用[11035(8885,21541)vs 4818(3749,6477.5),P<0.01]及日平均费用[1210(878,1964)vs 611(544,717),P<0.01)]均较非重症组明显增高,并且死亡率明显高于重症组(23.1%vs 0,P=0.003),但住院天数差异无统计学意义[10(6,16)vs 8(6,12.5),P= 0.297]。结论PEWS是简单有效的评分系统,在急性呼吸道感染患儿的门诊病情评估以及有效分流中具有准确的指导作用,可做为一种常规的评估工具。
儿童早期预警评分;门诊分流;病情严重指标;急性呼吸道感染
[Abstract]Objective To explore the value of pediatric early warning system score in distribution and disease evaluation of infant patients with acute respiratory infections in outpatient clinic.Methods Cross-sectional investigation was applied in this study.The data of infant patients with acute respiratory infections who were diagnosed in the Respiratory Outpatient of Second Affiliated Hospital of Wenzhou Medical University,Wenzhou Hospital of Combined TCM and Western Medicine From May1to May31in 2015 were collected,and PEWS scores were calculated.PEWS scores were compared between the hospitalized patients and non-hospitalized patients.The hospitalized infant patients were further assigned to the severe group and non-severe group according to the PEWS scores.Patients'age,time from first diagnosis to admission,expenses of hospitalization and daily average expenses were compared and analyzed between two groups.Results A total of 1954 infant patients data were collected in the study period,and PEWS score in most patients in the first diagnosis was≤2,and few patients were with the score of≥4.The PEWS score in the admitted patients was higher than that in the non-admitted patients.There was not significant difference of patients'age between the severe group and non-severe group[90(69.5,150)vs 93(72.5,152),P=0.750].The time from first diagnosis to admission in the severe group was significantly shorter than that in the non-severe group[0(0,0.5)vs 2(1,2),P<0.01],andthe hospitalization expenses[11035(8885,21541)vs 4818(3749,6477.5),P<0.01]and daily average expenses[1210(878,1964)vs 611(544,717),P<0.01]were all significantly higher than those in the non-severe group.The mortality rate was significantly higher than that in the severe group(23.1%vs 0,P=0.003),but the length of stay was not statistically significantly different[10(6,16)vs 8(6,12.5),P=0.297].Conclusion PEWS is a simple and effective scoring system,and plays an accurate guiding role in the evaluation of diseases in outpatient clinic and effective distribution in the infant patients with acute respiratory infections,which can be taken as a regular evaluation tool.
[Key words]Pediatric early warning scores;Outpatient distribution;Disease severity indicators;Acute respiratory infections
急性呼吸道感染是婴幼儿期最常见的疾病之一,因为婴幼儿自身气道窄、肺泡直径小、数量少,并且呼吸中枢调节能力差,在急性呼吸道感染疾病时易发生气道梗阻、呼吸衰竭。因此,对于患儿量较多的门诊,如何简单、快速、有效地识别高危患儿具有重要的意义。儿科早期预警系统评分(pediatric early warning score,PEWS)[1-2]可及时准确地识别儿童潜在的危重疾病,具有一定的临床应用价值[3],适用于普通病房住院患儿病情风险评估、急诊室患儿分流及预检分诊[4],同样适用于评估意外伤害急诊患儿的病情[5]。本研究选择2015年5月因急性呼吸道感染就诊的患儿1954例,首诊时进行儿科早期预警系统评分(PEWS),并对这部分患儿进行分析,评估该评分系统在门诊患儿分流及病情评估中的作用。现报道如下。
1 资料与方法
1.1一般资料
收集2015年5月1日~31日于在温州医科大学附属第二医院和温州市中西医结合医院呼吸科门诊就诊的急性呼吸道感染患儿1954例。非住院患儿1868例,收住入院患儿86例,其中男49例,女37例;其中按PEWS评分标准重症患儿13例,非重症患儿73例。纳入标准:年龄29 d~3岁;具有急性呼吸道感染症状:咳嗽、发热,伴或不伴影像学阳性结果;排除标准:免疫缺陷;先天性心脏病;支气管肺发育不良;先天性气道畸形(如气道狭窄和气道软化症)等。
1.2研究方法
采用横断面调查的方法,记录患儿的PEWS评分、分流去向。将住院的患儿分为重症组及非重症组,其中重症组纳入标准为PEWS评分≥4分或者一项评分达到3分[6,7],对重症组与非重症组患儿的年龄、初诊至入院的时间、住院费用、死亡率等进行比较。
1.3统计学方法
所有统计学检验使用SPSS19.0统计学软件进行计算,研究中定量资料给予正态检验分析,正态分布资料采用均数±标准差(x±s)描述,非正态分布资料用中位数、四分位数描述;符合正态分布、方差齐性的资料给予t检验,不符合正态分布及方差齐性的采用秩和检验,等级资料采用Krusakl-Wallis H检验。定性资料采用χ2检验或Fisher确切概率法分析。P<0.05为差异有统计学意义。
2 结果
2.1非住院及住院患儿的PEWS评分分布
2015年5月共收集1954份首次就诊时进行PEWS评分的患儿资料,根据此后的治疗过程分为住院患儿及非住院患儿两组,两组PEWS评分见表1及图1、2,将住院患儿与非住院患儿的PEWS评分分布用Krusakl-Wallis H分析比较发现,住院患儿的PEWS评分高于非住院患儿(P<0.01)。
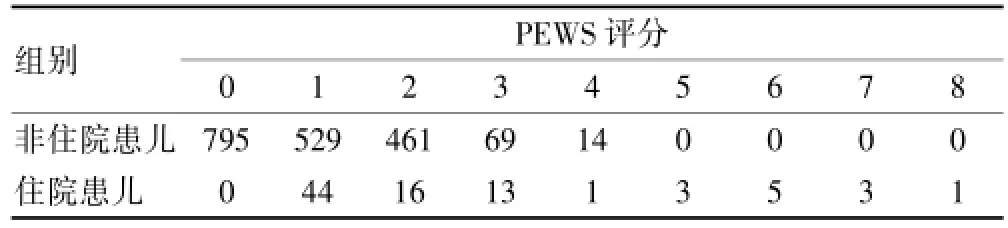
表1 非住院及住院患儿的PEWS评分分布(n)
2.2住院患儿的临床特征
根据PEWS评分将86例住院患儿分为重症组与非重症组。两组的临床特征见表2。两组患儿的年龄及性别未见明显差异,具有可比性。重症组从初诊至入院时间明显较非重症组短,住院费用及日平均费用均较非重症组明显增高,且死亡率明显高于重症组,但两组的住院天数比较差异无统计学意义(P>0.05)。
3 讨论
急性呼吸道感染是婴幼儿常见的感染性疾病,小儿呼吸系统解剖生理特点以及机体免疫特点致使该年龄段人群呼吸系统感染性疾病发病率高,其临床症状可以从不显性感染到威胁生命的重症感染,尤其是急性下呼吸道感染,严重威胁患儿健康。目前全世界每年死于肺炎的5岁以下儿童大约140万,占死因构成的18.3%,肺炎仍是第一位死亡原因[8]。在急性呼吸道感染的流行季节往往导致儿科门诊患者骤增,如何在就诊的患儿中早期识别病情危重的患儿并进行早期处理对于提高诊疗质量、改善患儿预后显得非常重要。

表2 重症组与非重症组的临床特征比较
为了准确识别急危重症患儿,目前临床上存在多种评分系统,其中APACHEⅡ评分是使用最广泛且较权威的评分工具[9],但该评分参数多、获取时间长、计算复杂,不利于对大量的门诊就诊患儿做出快速的评估。儿科早期预警系统评分(PEWS)是较为简单易操作的评分系统,包括神经系统(意识)、心血管系统和呼吸系统3个方面,不依赖年龄分类,操作较为简单,不需要用到特殊设备,且可重复性好,因此对于门诊患儿具有很强的操作性,可用于患儿病情变化的早期评价,为临床儿科医生的诊断和治疗决策提供依据,指导临床治疗[10-13]。

图1 非住院患儿PEWS评分分布
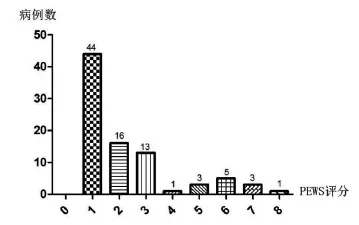
图2 住院患儿PEWS评分分布
本研究在2015年5月1日~31日共观察1954例门诊就诊的急性呼吸道感染患儿,结果显示住院患儿的PEWS评分高于非住院患儿(P<0.01),因此利用PEWS评分结果可以及时做出判断,可以对急性呼吸道感染患儿进行快速准确的分流。此外,门诊大部分的初诊患儿的PEWS评分≤2分,0~1分的患儿占了很大比例,属于无需处理、无需观察的干预等级,反映了国内家长对患儿急性呼吸道感染缺乏基本应变知识。因此,有必要对家长进行基本的医疗常识宣教,增强家庭处理患儿病情的能力,对轻症患儿可以减轻家庭以及医院的负担,同时避免不必要的医疗资源占用。在此基础上进一步对收住入院治疗的86例患儿进行分析,发现重症组就诊至收住病房的时间明显短于非重症组,在重症组中住院费用、日均住院费用及死亡率均明显高于非重症组,与Bell、Parshuuram等[14,15]的研究结果一样,也证实了PEWS评分可以做为评估患儿病情严重程度的指标等[16-17]。Egdell等[18]认为PEWS评分对于需要转入ICU的危重症患儿的识别敏感性为70%,特异性为90%。通过进行PEWS评分,能帮助医护人员方便、快捷地识别、处理危重症、潜在危重症患儿,提高监护级别,及早抢救或转移患儿去更恰当的治疗单元[19,20],可以减少临床医疗及护理安全隐患,提高医疗质量。
综上所述,本研究证实PEWS是简单有效的评分系统,在急性呼吸道感染患儿的门诊病情评估以及有效分流中具有准确的指导作用,适合在门诊患儿中做为一种常规的评估工具。
[1]Monaghan A.Detecting and managing deterioration in children[J].Paediatric Nursing,2005,17(1):32-35.
[2]Parshuram CS,Hutchison J,Middaugh K.Development and initial validation of the Bedside Paediatric Early WarningSystem score[J].Critical Care,2009,13(4):R135.
[3]任宏飞,刘常清,李继平.改良早期预警评分系统及其在急诊科的应用研究进展[J].护理学报,2013,20(2B):23-26.
[4]左超,祝益民.儿童早期预警评分的临床应用进展[J].中华儿科杂志,2014,52(9):712-714.
[5]王丽,张富强,何伟锋,等.儿童早期预警评分在意外伤害急诊患儿病情评估中的应用[J].护理学报,2015,22(16):56-58.
[6]Akre M,Finkelstein M,Erickson M,et al.Sensitivity of the pediatric early warning score to identify patient deterioration[J].Pediatrics,2010,125(4):e763-e769.
[7]陆国平,程晔.儿科早期预警系统评分[J].中华实用儿科临床杂志,2013,28(18):1361-1364.
[8]Liu L,Johnson HL,Cousens S,et al.Global,regional,and national causes of child mortality:An updated systematic analysis for 2010 with time trends since 2000[J].Lancet,2012,379(9832):2151-2161.
[9]Marcin JP,Pollack MM.Review of the methodologies and applications of scoring systems in neonatal and pediatric intensive care[J].Pediatric Critical Care Medicine:A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies,2000,1(1):20-27.
[10]Panesar R,Polikoff LA,Harris D,et al.Characteristics and outcomes of pediatric rapid response teams before and after mandatory triggering by an elevated Pediatric Early Warning System(PEWS)score[J].Hospital Pediatrics,2014,4(3):135-140.
[11]Gold DL,Mihalov LK,Cohen DM.Evaluating the Pediatric Early Warning Score(PEWS)system for admitted patients in the pediatric emergency department[J].Academic emergency medicine:Official Journal of the Society for Academic Emergency Medicine,2014,21(11):1249-1256.
[12]Breslin K,Marx J,Hoffman H,et al.Pediatric early warning score at time of emergency department disposition is associated with level of care[J].Pediatric Emergency Care,2014,30(2):97-103.
[13]蔡群,徐美玉,李斌.儿童早期预警评分在病毒性脑炎中的应用[J].江苏医药,2014,40(1):67-69.
[14]Bell D,Mac A,Ochoa Y,et al.The Texas Children's Hospital Pediatric Advanced Warning Score as a predictor of clinical deterioration in hospitalized infants and children:A modification of the PEWS tool[J].Journal of Pediatric Nursing,2013,28(6):e2-e9.
[15]Parshuram CS,Duncan HP,Joffe AR,et al.Multicentre validation of the bedside paediatric early warning system score:A severity of illness score to detect evolving critical illness in hospitalised children[J].Critical Care,2011,15(4):R184.
[16]Hunt EA,Zimmer KP,Rinke ML,et al.Transition from a traditional code team to a medical emergency team and categorization of cardiopulmonary arrests in a children's center[J].Archives of Pediatrics&Adolescent Medicine,2008,162(2):117-122.
[17]张佳燕,胡菲,张玉侠.儿童早期预警评分在留诊观察患儿分流中的应用[J].护理研究,2015,29(10):3744-3746.
[18]Egdell P,Finlay L,Pedley DK.The PAWS score:Validation of an early warning scoring system for the initial assessment of children in the emergency department[J]. EMJ,2008,25(11):745-749.
[19]张梅,范媛,朱继红,等.儿童早期预警评分系统在小儿普外科中的应用[J].中华现代护理杂志,2014,20(32):4133-4137.
[20]Solevag AL,Eggen EH,Schroder J,et al.Use of a modified pediatric early warning score in a department of pediatric and adolescent medicine[J].Plo S One,2013,8(8):e72534.
Value of pediatric early warning system score in distribution and disease evaluation of infant patients with acute respiratory infections in outpatient clinic
HU Shidong1WU Haizhen2MA Lili1HU Xiaoguang1JIA Xiaohui1
1.Department of Pediatric Respiratory,the Second Affiliated Hospital of Wenzhou Medical University,Wenzhou 325027,China;2.Department of ICU,Wenzhou Hospital of Combined TCM and Western Medicine,Wenzhou325000,China
R725.6
A
1673-9701(2016)24-0008-04
2016-05-26)
浙江省医药卫生科技计划项目(2014RCA015)
