不同年龄保乳治疗的乳腺癌患者临床病理特征及预后分析
2016-05-31穆兰肖盟刘伟色刘苗王欣
穆兰,肖盟,刘伟色,刘苗,王欣
不同年龄保乳治疗的乳腺癌患者临床病理特征及预后分析
穆兰,肖盟,刘伟色,刘苗,王欣△
摘要:目的分析不同年龄保乳治疗的乳腺癌患者临床病理特征及预后。方法回顾性分析1997年10月—2010年5月天津医科大学肿瘤医院收治的827例行保乳治疗的乳腺癌患者的临床资料,根据诊断乳腺癌时年龄不同分3组,比较3组患者临床病理特征及生存情况。结果827例患者中,≤35岁组129例、36~54岁组530例、≥55岁组168例。≤35岁组患者中淋巴结转移数≥4的患者比例较大,且激素受体阴性率也较高。≤35岁组、36~54岁组、≥55岁组5年无局部复发生存率分别为86.0%、93.6%、94.0%(P < 0.01),5年无远处转移生存率分别为88.4%、91.3%、94.6%(P > 0.05),5年总生存率分别为91.5%、94.3%、95.2%(P > 0.05)。多因素分析显示,年龄≤35岁组的患者5年局部复发风险较36~54岁组及≥55岁组患者显著增高,5年远处转移风险高于≥55岁组的患者(P < 0.05),但5年死亡风险并未增加(P > 0.05)。结论≤35岁乳腺癌患者保乳术后5年局部复发及远处转移风险较高,5年死亡风险并未增加,仍可接受保乳治疗。
关键词:乳腺肿瘤;年龄组;肿瘤复发,局部;肿瘤转移;死亡;保乳治疗
△通讯作者E-mail:wangxin@tjmuch.com
近年来,保乳治疗成为早期乳腺癌患者理想的治疗方法[1]。保乳术创面小,保留形体美感[2],使年轻患者更倾向于选择保乳治疗[3]。据报道,年轻乳腺癌患者保乳治疗后局部复发风险较高,预后较差,特别是≤35岁的患者更是如此[4-5]。但也有学者认为,年龄与保乳治疗后患者预后无关[6]。因此,本研究对不同年龄保乳治疗的乳腺癌患者临床病理特征及预后结果进行比较,并探讨年龄对患者预后的影响。
1 资料与方法
1.1病例资料收集1997年10月—2010年5月天津医科大学肿瘤医院收治的行保乳治疗的乳腺癌患者临床资料。纳入标准:病理确诊为乳腺癌并接受保乳手术治疗;有完整的临床病理资料。排除标准:初治时已发现远处转移;炎性乳腺癌;诊断为乳腺癌后5年内死于其他疾病;男性乳腺癌。共收集827例,年龄19~85岁,中位年龄46岁。根据患者诊断乳腺癌时年龄不同分为:≤35岁组129例、36~54岁组530例、≥55岁组168例。
1.2方法所有患者均行肿瘤局部扩大切除术加腋窝淋巴结清扫术或前哨淋巴结活检术,术中对标本上、下、内、外、浅表、基底6点取材,行冰冻病理检查。术后行放疗和辅助化疗,对雌激素受体、孕激素受体阳性的患者行内分泌治疗,药物以三苯氧胺为主。
1.3随访术后2年内每3个月复查1次,术后第3年开始每6个月复查1次,术后第5年后每年复查1次。复查内容主要包括乳腺肿瘤标志物、乳腺超声、钼靶、胸X线片、腹部超声等检查,必要时行全身骨扫描等检查。通过临床及组织学检测诊断乳腺癌局部复发或远处转移情况。随访方式为电话、信件、查阅门诊住院病历等。随访内容主要为患者是否生存及复发转移。局部复发及远处转移时间按确诊乳腺癌日期至确诊肿瘤复发转移日期计算。总生存时间按确诊乳腺癌日期至乳腺癌相关性死亡或随访截止日期计算。随访截止时间为2015年5月。
1.4统计学方法采用SPSS 17.0软件进行统计学分析。运用χ2检验比较不同年龄组之间临床病理学特征差异,采用Kaplan-Meier法进行生存分析,Log-rank法进行组间对比,采用Cox比例风险回归模型进行多因素分析。P < 0.05为差异有统计学意义。
2 结果
2.1临床病理学特征≤35岁组未绝经为100.0%,均高于其他2组;淋巴结转移数≥4占8.5%,高于≥55岁组;雌激素受体阴性患者占45.7%,高于≥55岁组的患者;孕激素受体阴性率48.8%,高于36~54岁组;完成新辅助化疗的患者占10.9%,均高于另外2组;完成术后化疗的患者为100.0%,高于≥55岁组;未行内分泌治疗的患者占45.7%,均高于其他2组(均P < 0.016 7)。癌症家族史、肿瘤大小、病理类型、组织学分级、人表皮生长因子受体2(HER2)及放疗方面差异无统计学意义,见表1。
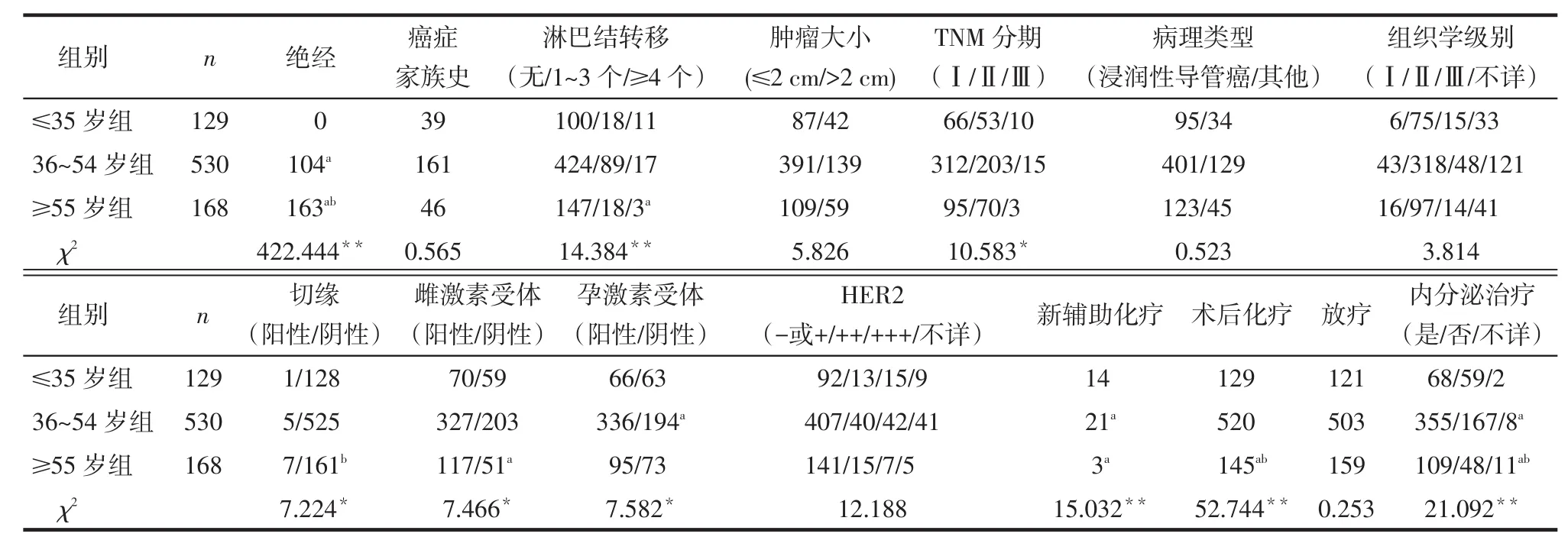
Tab. 1 Comparison of clinicopathological characteristics in patients with breast-conserving treatment between different age groups表1 不同年龄组保乳治疗的乳腺癌患者临床病理特征比较 例
2.2不同年龄组患者预后分析全体患者中位随访时间为84个月(18~209个月),5年局部复发率为7.5%,远处转移率为8.5%,死亡率为5.9%。Ka⁃plan-Meier生存分析显示:≤35岁组、36~54岁组、≥55岁组乳腺癌患者5年无局部复发生存率分别为86.0%、93.6%、94.0%(P < 0.01);5年无远处转移生存率为88.4%、91.3%、94.6%(P > 0.05);5年总生存率为91.5%、94.3%、95.2%(P > 0.05),见表2。不同年龄保乳治疗的乳腺癌患者5年无局部复发、5年无远处转移及5年总生存曲线分别见图1~3。
2.3单因素分析单因素分析结果显示,未接受化疗或放疗、组织学分级较高的乳腺癌患者5年局部复发率较高;未接受化疗或放疗的乳腺癌患者5年远处转移率较高;未化疗的患者死亡率较高(P< 0.05),见表2。

Tab. 2 Comparison of 5-year local regional relapse-free survival, distant metastasis-free survival and overall survival in patients with breast-conserving treatment according to different clinicopathological characteristics between different age groups表2 不同临床病理特征下保乳治疗患者5年无局部复发生存率、无远处转移生存率及总生存率比较 例

Fig.1 Survival curves of 5-year local regional relapse-free survival for patients with breastconserving treatment in different age groups图1 不同年龄组保乳治疗的患者5年无局部复发生存曲线

Fig. 2 Survival curves of 5-year distant metastasis-free survival for patients with breastconserving treatment in different age groups图2 不同年龄组保乳治疗的患者5年无远处转移生存曲线

Fig. 3 Survival curves of 5-year overall survival for patients with breast-conserving treatment in different age groups图3 不同年龄组保乳治疗的患者5年总生存曲线
2.4多因素分析将单因素分析中P< 0.1的因素纳入Cox比例风险模型进行多因素分析。结果提示:≤35岁组乳腺癌患者保乳术后5年局部复发风险与36~54岁组相比显著增加(HR=2.266,P= 0.006),与≥55岁组相比也显著升高(HR=3.075,P= 0.011)。其5年远处转移风险与≥55岁组相比明显升高(HR=3.067,P= 0.014)。年龄与保乳治疗患者5年死亡风险无关(P > 0.05)。组织学分级是保乳治疗患者的独立预后因素,化疗及放疗均降低保乳治疗患者5年局部复发及远处转移风险,而化疗可降低其5年死亡风险,见表3。

Tab. 3 Multivariate analysis of 5-year local regional relapse, distant metastasis and mortality risk of patients with breastconserving treatment表3 保乳治疗的乳腺癌患者5年局部复发、远处转移及死亡风险的多因素分析
3 讨论
3.1保乳治疗的年轻乳腺癌患者临床病理特征及预后本研究827例行保乳治疗的患者中,年龄≤35岁的患者中淋巴结转移数≥4的患者所占比例较大,且激素受体阴性的患者比例也较大。研究报道,年轻乳腺癌患者肿瘤侵袭性较强且诊断乳腺癌时倾向于晚期[7]。此外,其淋巴结阳性率较高,激素受体多为阴性,组织学级别也较高,淋巴管及血管浸润也比较普遍[8-9]。尽管对年轻乳腺癌的定义不完全相同,但这些研究结果与本研究基本一致。本研究中,年龄≤35岁的患者行新辅助化疗及术后化疗的比例较高,但其5年无局部复发生存率(86.0%)低于36~54岁(93.6%)及≥55岁(94%)的患者(P < 0.01)。此外,多因素分析结果显示,年龄≤35岁的患者5年局部复发风险显著高于36~54岁及≥55岁的患者,其5年远处转移风险高于≥55岁患者,说明年龄≤35岁是导致保乳治疗的乳腺癌患者预后不良的独立危险因素。其主要原因可能是年轻乳腺癌患者乳腺富含更多的胰岛素样生长因子(IGF)-1,其水平升高被认为是绝经前女性患乳腺癌的独立危险因素[10]。另外,年轻乳腺癌患者较高的局部复发率可能与其肿瘤组织克隆性微病变也有关[11]。
3.2年轻乳腺癌患者保乳治疗的探讨保乳治疗对年轻乳腺癌患者预后的影响,文献报道结果并不一致。研究指出,年龄<35岁乳腺癌患者保乳治疗后局部复发风险高于35~40岁患者[12]。年龄<45岁的患者10年局部复发风险明显高于年龄≥45岁的患者[3,13]。年龄<50岁也被认为是局部复发率升高的独立危险因素[14]。尽管各研究纳入的患者不同,对年轻乳腺癌的定义以及选取的临床病理因素不同,但总的来讲,年轻乳腺癌患者保乳治疗后局部复发风险是增高的。这与本研究结果一致。但是,也有研究发现年龄与保乳治疗患者局部复发风险并无关系[6]。本研究还发现,年龄≤35岁与≥55岁患者相比5年远处转移风险增加了,但与36~54岁患者相比风险并未增加。据报道,年龄≤35岁与>35岁的患者相比,远处转移的风险并未增加[15];年龄≤40岁的乳腺癌患者远处转移风险与>40岁的患者相比也没有增加[16]。当然,这些研究的分组方法、比较标准、纳入人群、随访时间等与本研究相比存在差异,因而研究结果也不尽相同。本研究中,年轻乳腺癌患者5年死亡风险未增加,可能与年轻患者身体基础状况较好有关。此外,有研究报道,与保乳治疗相比,根治性手术并没有改善年轻乳腺癌患者的预后[17],而保乳治疗后局部复发的早发现及早治疗也能够改善年轻乳腺癌患者的预后[18]。
综上所述,虽然年轻乳腺癌患者保乳治疗后局部复发及远处转移风险较高,但死亡风险并未增加。因此,保乳治疗对于年轻患者来讲并不是禁忌证。保乳治疗仍然是年轻乳腺癌患者一个可供选择的治疗方式,该结论有待今后更大样本的研究加以证实。
参考文献
[1] Franceschini G, Sanchez AM, Di Leone A, et al. Update on the surgical management of breast cancer [J]. Ann Ital Chir, 2015, 86: 89-99.
[2] Acil H, Cavdar I. Comparison of quality of life of Turkish breast cancer patients receiving breast conserving surgery or modified radical mastectomy[J]. Asian Pac J Cancer Prev, 2014, 15(13): 5377-5381.
[3] Vicini FA, Shaitelman S, Wilkinson JB, et al. Long-term impact of young age at diagnosis on treatment outcome and patterns of failure in patients with ductal carcinoma in situ treated with breast-con⁃serving therapy[J]. Breast J, 2013, 19(4): 365-373. doi: 10.1111/ tbj.12127.
[4] Hattangadi-Gluth JA, Wo JY, Nguyen PL, et al. Basal subtype of in⁃vasive breast cancer is associated with a higher risk of true recur⁃rence after conventional breast-conserving therapy[J]. Int J Radiat Oncol Biol Phys, 2012, 82(3): 1185- 1191. doi: 10.1016/j. ijrobp.2011.02.061.
[5] Goksu SS, Tastekin D, Arslan D, et al. Clinicopathologic features and molecular subtypes of breast cancer in young women(age
[6] Fredriksson I, Liljegren G, Arnesson LG, et al. Local recurrence in the breast after conservative surgery-- a study of prognosis and prognostic factors in 391 women[J]. Eur J Cancer, 2002, 38(14): 1860-1870.
[7] Lee HB, Han W. Unique features of young age breast cancer and its management[J]. J Breast Cancer, 2014, 17(4): 301- 307. doi: 10.4048/jbc.2014.17.4.301.
[8] Ahn SH, Son BH, Kim SW, et al. Poor outcome of hormone recep⁃tor-positive breast cancer at very young age is due to tamoxifen re⁃sistance: nationwide survival data in Korea--a report from the Kore⁃ an Breast Cancer Society[J]. J Clin Oncol, 2007, 25(17): 2360-2368. doi: 10.1200/JCO.2006.10.3754.
[9] Thapa B, Singh Y, Sayami P, et al. Breast cancer in young women from a low risk population in Nepal[J]. Asian Pac J Cancer Prev, 2013, 14(9): 5095-5099.
[10] Eriksson L, Czene K, Rosenberg L, et al. Possible influence of mam⁃mographic density on local and locoregional recurrence of breast cancer[J]. Breast Cancer Res, 2013, 15(4): R56. doi: 10.1186/ bcr3450.
[11] Chen W, Sonke JJ, Stroom J, et al. The effect of age in breast con⁃serving therapy: a retrospective analysis on pathology and clinical outcome data[J]. Radiother Oncol, 2015, 114(3): 314- 321. doi: 10.1016/j.radonc.2015.01.010.
[12] Oh JL, Bonnen M, Outlaw ED, et al. The impact of young age on lo⁃coregional recurrence after doxorubicin-based breast conservation therapy in patients 40 years old or younger: How young is "young" [J]? Int J Radiat Oncol Biol Phys, 2006, 65(5): 1345-1352. doi: 10.1016/j.ijrobp.2006.03.028.
[13] Kong I, Narod SA, Taylor C, et al. Age at diagnosis predicts local re⁃currence in women treated with breast-conserving surgery and post⁃operative radiation therapy for ductal carcinoma in situ: a popula⁃tion-based outcomes analysis[J]. Curr Oncol, 2014, 21(1): e96-e104. doi: 10.3747/co.21.1604.
[14] Rakovitch E, Nofech-Mozes S, Hanna W, et al. A population-based validation study of the DCIS Score predicting recurrence risk in in⁃dividuals treated by breast-conserving surgery alone[J]. Breast Can⁃cer Res Treat, 2015, 152(2): 389-398. doi: 10.1007/s10549-015-3464-6.
[15] Komoike Y, Akiyama F, Iino Y, et al. Ipsilateral breast tumor recur⁃rence(IBTR)after breast- conserving treatment for early breast cancer: risk factors and impact on distant metastases[J]. Cancer, 2006, 106(1): 35-41. doi: 10.1002/cncr.21551.
[16] Bijker N, Peterse JL, Duchateau L, et al. Risk factors for recurrence and metastasis after breast-conserving therapy for ductal carcino⁃ma-in-situ: analysis of European Organization for Research and Treatment of Cancer Trial 10853[J]. J Clin Oncol, 2001, 19(8): 2263-2271.
[17] Cao JQ, Truong PT, Olivotto IA, et al. Should women younger than 40 years of age with invasive breast cancer have a mastectomy? 15-year outcomes in a population-based cohort[J]. Int J Radiat Oncol Biol Phys, 2014, 90(3): 509-517. doi: 10.1016/j.ijrobp.2014.06.041.
[18] van der Sangen MJ, Poortmans PM, Scheepers SW, et al. Prognosis following local recurrence after breast conserving treatment in young women with early breast cancer[J]. Eur J Surg Oncol, 2013, 39(8): 892-898. doi: 10.1016/j.ejso.2013.05.004.
(2015-08-04收稿2015-10-03修回)
(本文编辑李鹏)
作者单位:天津医科大学肿瘤医院乳腺肿瘤一科,国家肿瘤临床医学研究中心,天津市肿瘤防治重点实验室,乳腺癌防治教育部重点实验室(邮编300060)
Analysis of clinicopathological features and prognosis in different-age patients with breast cancer treated with breast-conserving therapy
MU Lan,XIAO Meng,LIU Weise,LIU Miao,WANG Xin△
The First Department of Breast Cancer, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin Medical University, Ministry of Education, Key Laboratory of Breast Cancer Prevention and Therapy, Tianjin 300060, China
△Corresponding Author E-mail: wangxin@tjmuch.com
Abstract:Objective To analyze the clinicopathological features and prognosis in patients with breast cancer treated with breast-conserving therapy according to the age when breast cancer diagnosed. Methods Clinical data of 827 patients with breast-conserving therapy in Tianjin Medical University Cancer Institute and Hospital from October 1997 to May 2010 were analyzed retrospectively. According to age when breast cancer was diagnosed, patients were subdivided into three groups. Clinicopathological characteristics and survival were compared between three groups. Results Of the 827 patients, 129 cases were≤35 years old, 530 cases were 36-54 years old and 168 cases were aged≥55 years. The proportion of lymph node metastasis number≥4 and the negative rate of hormone receptors were higher in patients with age≤35 years old. The 5-year local regional recurrence-free survival rates were 86.0%, 93.6%, and 94.0% for patients aged≤35 years old, 36-54 years old, and≥55 years old, respectively (P < 0.01). The 5-year distant metastasis-free survival rates were 88.4%, 91.3%, and 94.6% for patients with age≤35 years old, 36-54 years old, and≥55 years old, respectively (P > 0.05). The 5-year over⁃all survival rates were 91.5%, 94.3%, and 95.2% for patients aged≤35 years old, 36-54 years old, and≥55 years old, respec⁃tively (P > 0.05). Multivariate analysis showed that 5-year local regional relapse risks were significantly increased in patients aged≤35 years compared to patients aged 36-54 years and≥55 years (P < 0.05), and the 5-year distant metastasis risk was higher in this group than that of patients aged≥55 years (P = 0.014), while 5-year mortality risk was not increased in patients with age≤35 years old (P > 0.05). ConclusionAfter breast-conserving therapy, the risk of 5-year local regional recurrence and distant metastasis are relatively higher in patients aged≤35 years old, while the risk of mortality within 5 years does not increase in this group. Patients with age≤35 years old remain appropriate candidates for breast-conserving treatment.
Key words:breast neoplasms;age groups;neoplasm recurrence, local;neoplasm metastasis;death;breast-conserving therapy
中图分类号:R737.9
文献标志码:A
DOI:10.11958/20150088
基金项目:国家自然科学基金资助项目(81472472)
作者简介:穆兰(1989),女,硕士在读,主要从事乳腺肿瘤外科学研究
