超声造影在肾脏囊性病变良恶性鉴别中的应用价值
2016-05-31忻晓洁毛怡然张晟
忻晓洁,毛怡然,张晟
超声造影在肾脏囊性病变良恶性鉴别中的应用价值
忻晓洁,毛怡然,张晟
摘要:目的探讨超声造影在囊性肾癌诊断中的应用价值。方法选取我院肾脏囊性病变患者73例,分析二维超声及超声造影检查的图像特征,73例均行手术治疗并取得病理结果,对比病理结果评价2种方法的诊断价值。结果囊性肾癌64例,肾囊肿9例。二维灰阶及彩色多普勒超声显示囊性肾癌多表现为形状不规则,壁厚,内有实性成分或分隔,并多伴有血流信号;肾囊肿多表现为形状规则,内有少许实性成分或纤薄分隔,无明显血流信号。超声造影显示囊性肾癌造影剂起始时间(15.13±4.21)s,达峰时间(23.42±5.68)s,消退时间(28.42±4.27)s;增强方式表现为快进快退22例(34.3%)、快进慢退30例(46.8%)、慢进快退2例(3.2%)、慢进慢退4例(6.3%)、等进等退6例(9.3%);增强强度呈现高增强42例(65.6%)、等及低增强22例(34.4%)。肾囊肿中3例未见造影剂充盈,余6例造影剂起始时间(16.67±2.73)s,达峰时间(25.83±3.06)s,消退时间(34.17±4.26)s;增强方式表现为快进快退1例(16.7%)、快进慢退1例(16.7%)、等进等退4例(66.6%);增强强度呈高增强2例(33.3%)、等或低增强4例(66.7%)。二维灰阶超声在肾脏囊性病变诊断中的敏感度、特异度、阳性预测值、阴性预测值、准确度分别为85.9%、66.7%、94.8%、40.0%、83.6%,超声造影为92.2%、77.8%、96.7%、58.3%、90.4%。结论超声造影技术可以作为囊性肾癌诊断及鉴别诊断的一种有效方法。
关键词:肾肿瘤;超声检查,多普勒;囊性肾癌;超声造影技术;敏感性与特异性
囊性肾癌(cystic renal cell carcinoma,CRCC)是指在影像学或手术中发现的具有囊性改变的肾癌,与复杂囊肿鉴别不易,诊断的准确率较低。超声造影作为一项新技术,因其能够更好地显示低速血流,近年来发展迅速,在临床中获得较为广泛的应用[1]。本研究通过对二维超声及超声造影在囊性肾癌诊断结果的对比,探讨超声造影技术在囊性肾癌诊断及鉴别诊断中的应用价值。
1 对象与方法
1.1研究对象选择2012年1月—2015年3月在我院检查并诊断为肾脏囊性占位的患者共73例,男52例,女21例,年龄16~72岁,平均(42.6±13.7)岁,均于我院接受手术治疗并取得病理结果。病变位于右肾41例,左肾32例。病灶最大者13.7 cm×9.2 cm,最小者1.8 cm×1.3 cm。
1.2仪器与试剂应用PHILPS IU22彩色多普勒超声仪,C5~1探头,频率1.0~5.0 MHz,机械指数(MI)0.05~0.08。超声造影剂为六氟化硫微泡注射液(商品名:声诺维Sono Vue)。取5 mL生理盐水与冻干粉配置成混悬液,震荡5 s后,取1.5 mL经肘正中静脉快速团注后,以5 mL生理盐水冲管。
1.3方法
1.3.1二维及彩色多普勒检查患者取仰卧位或侧卧位,应用二维灰阶模式进行检查,观察病灶大小、形态、边界、囊壁厚度、内部回声、有无分隔及实性结节等。应用彩色多普勒模式观察病灶的血流情况。
1.3.2超声造影检查通过二维灰阶超声检查确定病灶位置,选定肿瘤的最佳扫查位置和最大切面,通过肘正中静脉注入造影剂,转换至造影模式,动态观察造影过程,时间约为2~6 min,采集并存储图像。
1.3.3图像分析由至少2位高年资医师对病灶进行分析,观察病灶造影表现,包括起始时间、达峰时间、消退时间、增强方式及增强强度等。起始时间为注药后于病灶内最开始出现造影剂时间。达峰时间为造影剂灌注达峰值的时间。消退时间为造影剂开始消退时间。增强方式:达峰时间与肾皮质基本相同为同步增强,快于肾皮质为快进增强,慢于肾皮质为减慢增强;增强后与肾皮质同时减退为同步减退,减退快于肾皮质为快速减退,减退慢于肾皮质为缓慢减退。增强强度:高增强为峰值强度高于肾皮质,等或低增强为峰值强度等或低于肾皮质。
1.3.4病理学检查肿物手术切除后送病理检验。取材用4%甲醛固定、石蜡包埋脱水,取最佳切面切片。对标本进行苏木素-伊红(HE)染色及链霉亲和素-过氧化物酶(streptavi⁃din peroxidase,SP)免疫组化染色。采用2004年WHO肾脏肿瘤组织学分类方法进行分类。
1.4统计学方法采用SPSS 13.0软件进行统计分析。起始时间、达峰时间、消退时间用均数±标准差(x ±s)表示。以病理学诊断结果为金标准,评价2种影像诊断方法的敏感度和特异度。
2 结果
2.1二维灰阶超声及彩色多普勒诊断特征囊性肾癌多表现为边界不清晰、形状不规则的囊性或囊实性肿物,壁较厚,肿物内可见中等回声或中强回声的实性成分或分隔,见图1。应用彩色多普勒观察,周边或内部可见星点状、线状或半环状血流信号,见图2。良性病变多表现为边界清晰、形状尚规则的囊性肿物,囊壁较薄、光滑,部分病变内部可见低弱回声或分隔。应用彩色多普勒观察多数肿物未探及血流信号。

Fig.1 Ultrasound image features of cystic renal carcinoma图1 囊性肾癌二维灰阶超声图像特征
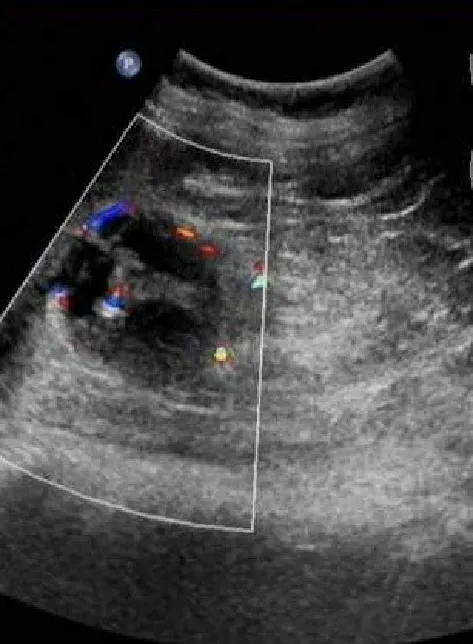
Fig. 2 Color doppler image features of cystic renal carcinoma图2 囊性肾癌彩色多普勒图像特征
2.2超声造影诊断特征
2.2.1囊性肾癌超声造影特征囊性肾癌共64例。包括单房囊肿型4例,多房囊肿型28例,囊实型32例。起始时间11~18 s,平均(15.13±4.21)s;达峰时间19~28 s,平均(23.42±5.68)s;消退时间26~41 s,平均(28.42±4.27)s。增强模式:造影剂充填快于肾皮质,呈快进52例;慢于肾皮质,呈慢进6例;与肾皮质呈同步6例。快于肾皮质消退,呈快退24例;慢于肾皮质消退,呈慢退34例;与肾皮质同步消退6例。快进慢退30例(46.8%)、快进快退22例(34.3%)、慢进快退2例(3.2%)、慢进慢退4例(6.3%)、等进等退6例(9.3%)。增强水平:病灶中增强水平高于肾皮质,呈高增强42例(65.6%);与肾皮质增强水平相同或低于肾皮质,呈等或低增强22例(34.4%),见图3、4。
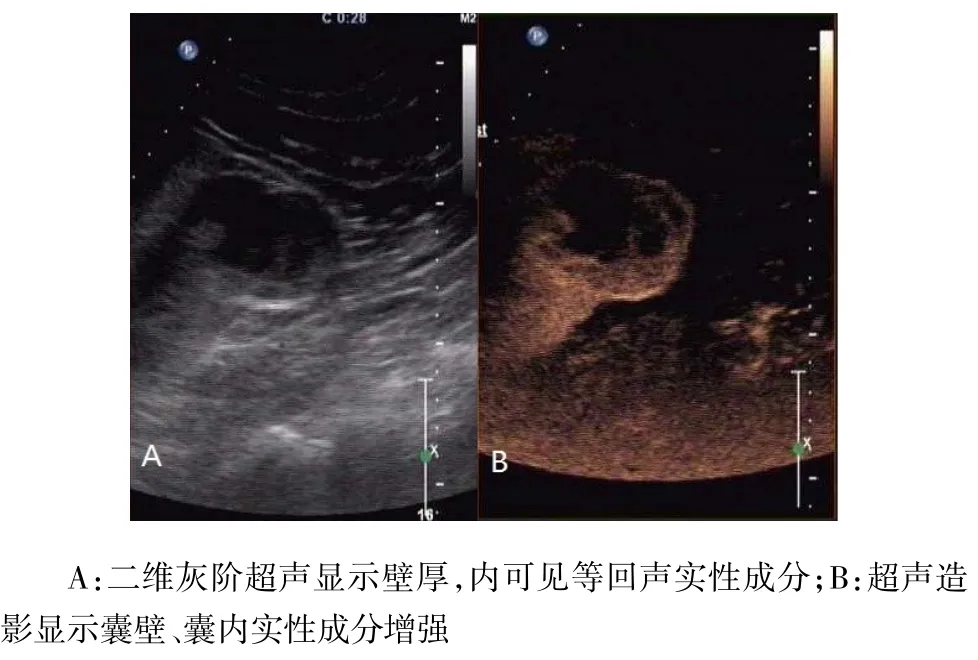
Fig. 3 Comparison of ultrasound and contrast-enhanced ultrasound imaging in cystic-solid renal carcinoma图3 囊实型肾癌二维超声及超声造影图像比较
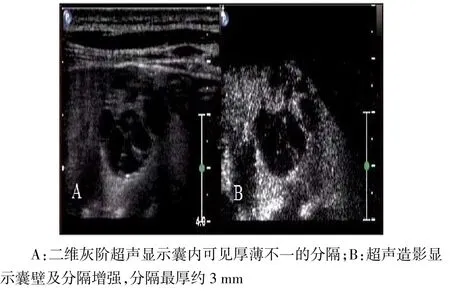
Fig.4 Comparison of ultrasound and contrast-enhanced ultrasound imaging in multiocular cystic renal carcinoma图4 多房囊肿型肾癌二维超声及超声造影图像对比
2.2.2肾囊肿超声造影特征肾囊肿9例,包括单房性3例,多房性6例。3例未见造影剂充盈;余6例造影剂起始时间13~21 s,平均(16.67±2.73)s,达峰时间22~31 s,平均(25.83±3.06)s,消退时间28~ 42 s,平均(34.17±4.26)s。增强方式表现为快进快退1例(16.7%)、快进慢退1例(16.7%)、等进等退4例(66.6%)。增强强度:高增强2例(33.3%)、等或低增强4例(66.7%),见图5。
2.3病理诊断本组73例病变中,病理回报恶性肿瘤64例,其中囊性透明细胞癌36例、肾乳头癌3例、多房囊性肾细胞癌22例、转移癌3例(原发灶为卵巢)。病理回报良性病变9例,为肾脏囊肿,伴有出血、积化或炎症。
2.4二维超声及超声造影诊断比较二维灰阶超声、超声造影及病理诊断结果,见表1。二维超声在肾脏囊性病变诊断的敏感度、特异度、阳性预测值、阴性预测值及准确度分别为85.9%、66.7%、94.8%、40.0%、83.6%,超声造影为92.2%、77.8%、96.7%、58.3%、90.4%。
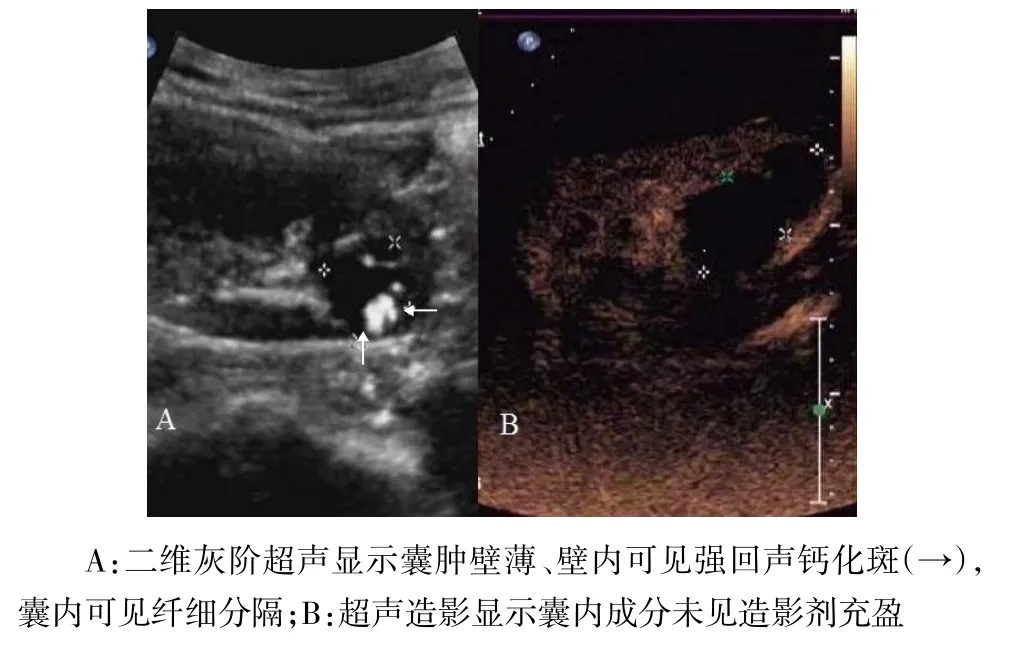
Fig. 5 Comparison of ultrasound and contrast-enhanced ultrasound imaging in complex renal cyst图5 复杂性肾囊肿二维超声及超声造影图像比较
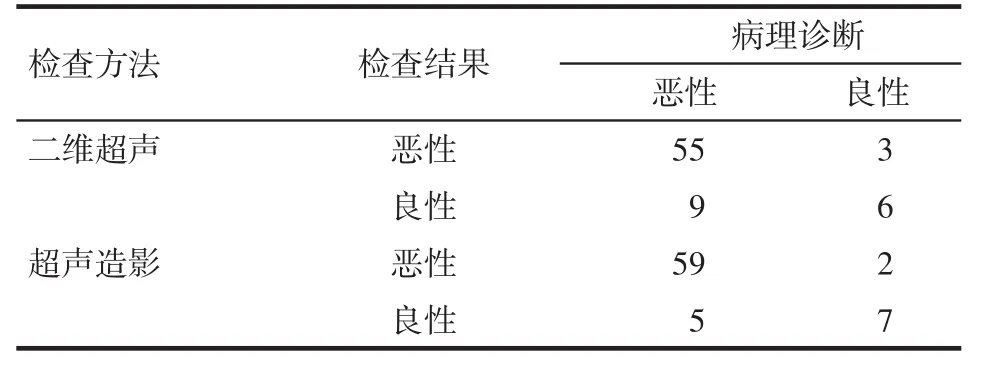
Tab.1 Comparison of diagnostic results between ultrasound and contrast-enhancement ultrasound and pathological detection of cystic renal tumors表1 二维灰阶超声、超声造影及病理诊断结果比较(例)
3 讨论
3.1超声造影在囊性肾癌中的应用囊性肾癌是一种特殊类型肾癌,约占肾脏恶性肿瘤的10%,与复杂性肾囊肿鉴别困难,易出现漏诊及误诊。常规超声检查受肿瘤位置、大小、深度影响,病灶囊壁及内部结构不能清晰显示,更无法显示血供。近年来超声造影技术不断发展进步,已成为评价囊性肾癌血供的新方法。恶性肿瘤血管多数发育畸形、走形迂曲、排列紊乱,呈旋涡状血管网或血窦[2]。超声造影对肾脏囊性病变血供的显示率达73.5%,高于增强CT的55.6%[3]。超声造影利用造影剂中微气泡成分增加组织及血管的声阻抗差,可敏感显示肿瘤内毛细血管,提高囊性肾癌诊断的准确度[4]。
3.2影响增强特征的因素肾脏囊性肿物超声造影增强特征与肿瘤内部血管的数目、密度、血管有无扭曲及短路等情况相关。由于肾脏血供丰富,内部有较多微血管,囊性肾癌增强模式多表现为快进慢退及快进快退[5]。本研究中快进慢退30例,快进快退22例。肿瘤内部血管密度高、管径大、存在动静脉瘘,减少了造影剂在病灶内充盈及灌注时间,表现为快进快退;当肿瘤内部血管密度小、管径小、血管走形迂曲或者存在栓塞时,增加了造影剂充盈时间,表现为慢退[6]。Nilsson等[7]在对肾脏实性病变的研究中发现,超声造影的增强模式与肿瘤分化程度相关。在本研究中,与病理结果对比发现,低分化的恶性肿瘤多表现为快进快退,而高分化的恶性肿瘤多表现为快进慢退。
3.3多房囊肿型囊性肾癌超声造影特征囊性肾癌根据声像图表现及形成机制可分为3型:单房囊肿型、多房囊肿型和囊实型。其中多房囊肿型肾癌与复杂性肾囊肿在影像学鉴别更为困难。多房囊肿型肾癌超声图像多表现为囊性病变内数量不同、粗细不等的分隔,复杂性肾囊肿则多表现为光滑纤细的分隔。在进行良恶性鉴别诊断时,分隔数目、厚度以及血流分布具有较高的价值[8]。Bosniak分级系统认为分隔厚度>1 mm,分隔数目≥4条判断为恶性的可能性较大[9]。曾红春等[10]提出分隔数目≥3条及分隔厚度≥1.75 mm可作为囊性病灶良恶性的最佳诊断界值。本研究中1例多房囊性占位,囊壁厚,分隔数目>4条,厚度>2 mm,囊壁可见低增强,结合其特征考虑为囊性肾癌,但术后病理提示为囊肿。因此在鉴别诊断时需综合判断,提高诊断准确度。
3.4肾脏囊肿超声造影特征肾脏良性囊性病变在二维超声表现为壁薄、无回声囊性病变,超声造影多表现为无造影剂充填的囊肿或者周边可见环状或半环状增强的病变。造影剂充填及消退时间与肾皮质相似,在肾脏囊肿内并发出血或炎症时,囊肿内部分隔不规则增厚、囊壁结节钙化、实性成分或其内可见少许低增强时,与囊性肾癌鉴别困难,容易发生误诊及漏诊[11]。
综上所述,超声造影能够帮助显示病变内低速血流,使肿物内新生血管网及毛细血管团显像,帮助提高肾脏囊性病变诊断的准确度,能够作为一种诊断及鉴别诊断的方法。
参考文献
[1] Li CX,Huang BJ. Research progress of quantitative analysis of re⁃nal tumor perfusion with contrast- enhanced ultrosonography[J]. Chin J Ultrasonography,2013,22(8):724-727.[李翠仙,黄备建.超声造影新技术对肾肿瘤血流灌注定量分析的研究进展[J].中华超声影像学杂志,2013,22(8):724-727].doi:10.3760/cma.j. issn.1004-4477.2013.08.020.
[2] Liu CY,Wang FX,Xie Q,et al. Diagnosis and different diagnosis of renal occuping lesions by contrast- enhanced ultrasound[J].J Clin Ultrasound in Med,2011,13(8):524-526.[刘春英,王芳晓,谢晴,等.肾脏占位病变的超声造影诊断及鉴别诊断[J].临床超声医学杂志, 2011,13(8):524-526].doi:10.3969/j.issn.1008-6978.2011.08.008.
[3] Jiang J,Chen YQ,Zhou YC. Contrast-enhanced ultrasonography of cystic renal cell carcinomas:conpared with contrast-enhanced CT[J]. Chin J Med Imaging Technol,2008,24(10):1628-1630.[蒋琚,陈亚青,周永昌.囊性肾癌的超声造影与增强CT对照研究[J].中国医学影像学,2008,24(10):1628-1630].doi:10.13929/j.1003-3289. 2008.10.044.
[4] Xu N.Progress in the application of contrast-enhanced ultrasonogra⁃phy in the diagnosis and differential diagnosis of cystic renal cell carcinoma[J].Medical Information,2015,28(9):345.[徐宁.超声造影在囊性肾癌及其鉴别诊断中的应用研究进展[J].医学信息,2015,28(9):345].
[5] Fan Y,Su HW.Investigation of value of contrast- enhanced ultra⁃sound in diagnosis for benign and malignant renal tumors[J].Medi⁃cal Recapitulate,2013,19(7):1332-1334.[樊勇,苏宏伟.超声造影在肾脏良恶性肿瘤诊断中的价值探讨[J].医学综述,2013,19 (7):1332-1334].doi:10.3969/j.issn.1006-2084.2013.07.066.
[6] Xu Y,Zhang S,Wei X,et al.Evaluation of complex cystic renal mass with contrast enhanced ultrasonography[J].J Clin Urology(Chi⁃na),2013,28(7):485-488.[徐勇,张晟,魏玺,等.超声造影评估复杂性囊性肾脏肿物的作用[J].临床泌尿外科杂志,2013,28 (7):485-488].doi:10.13201/j.issn.1001-1420.2013.07.019.
[7] Nilsson A. Contrast-enhanced ultrasound of the kidneys[J]. Eur Ra⁃diol, 2004, 14(8): 104-109.
[8] Ascenti G, Mazziotti S, Zimbaro G, et al.Complex cystic renal mass⁃es: characterization with contrast-enhanced US[J].Radiology,2007,243(1):158-165.
[9] Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system[J]. Radiology, 2004, 231(2):365 -371.
[10] Zeng HC,Mulati R,Wang YX,et al. Value of contrast-enhanced ul⁃trasonography using Bosniak criteria in the diagnosis of renal cystic lesions[J].Chin J Med Imaging Technol, 2014,30(12):1888-1892.[曾红春,木拉提·热夏提,王颖鑫,等.超声造影应用Bosniak分级诊断肾囊性病灶的价值[J].中国医学影像技术,2014,30(12):1888-1892].doi:10.13929/j.1003-3289.2014.12.046.
[11] Lin Y,Li JW,Wu SS.The value of SonoVue contrast-enhanced ul⁃trasound diagnosis in cystic renal cell carcinoma[J].Strait Pharma⁃ceutical Journal ,2014,26(12):158-159.[林芸,李建卫,吴松松.声诺维超声造影在囊性肾癌中的诊断价值[J].海峡药学,2014,26 (12):158-159].
(2015-05-19收稿2015-08-26修回)
(本文编辑李鹏)
应用研究
作者单位:天津医科大学肿瘤医院超声诊疗科,国家肿瘤临床医学研究中心,天津市肿瘤防治重点实验室(邮编300060)
The value of contrast-enhanced ultrasonography in differential diagnosis of cystic renal carcinoma
XIN Xiaojie,MAO Yiran,ZHANG Sheng
Department of Ultrasound, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center of Cancer, Key Laborary of Cancer Prevention and Therapy, Tianjin 300060, China
Abstract:ObjectiveTo evaluate the values of contrast-enhanced ultrasound in diagnosis of cystic renal cell carcino⁃ma. Methods A total of 73 patients with renal cystic lesions were included in this study. The image features of ultrasound and contrast-enhanced ultrasound examination were analysed. All of patients underwent surgical treatment and had patholog⁃ical results. The diagnostic values of the ultrasound and contrast-enhanced ultrasound were analyzed by evaluating the im⁃age features of cystic renal cell carcinoma. Results There were 64 cases of cystic renal cell carcinoma, 9 cases of benign cyst. With ultrasound and color doppler ultrasound,irregular shape, thickness wall, solid ingredients, divisions and more blood flow signals were found in cystic renal cell carcinoma. Renal cyst showed regular shape, few solid component and thin separation and inconspicuous blood flow signals. In contrast-enhanced ultrasound, cystic renal cancer contrast agent appear⁃ing time was (15.13±4.21)s, and reached the peak time (23.42±5.68)s, fade time was (28.42±4.27)s. The enhanced mode for fast in and fast out was found in 22 cases (34.3%), fast in and slow out in 30 cases (46.8%), slow in and fast out in 2 cases (3.2%), slow in and slow out in 4 cases (6.4%), and synchronously in and out in 6 cases (9.3%). The hyper-enhancement was found in 42 cases (65.6%), the iso-enhancement and hypo-enhancement in 22 cases (34.4%). In renal cyst, There were three cases out of contrast filling. In other 6 cases, the contrast agent appearing time was (16.67±2.73)s, the peak time was (25.83±3.06)s and fade time was (34.17±4.26)s. The enhanced mode for fast in and fast out was found in 1 case (16.7%), fast in and slow out in 1 case (16.7%) and synchronously in and out in 4 cases (66.6%). The hyper-enhancement was found in 2 cases (33.3%), the iso-enhancement and hypo-enhancement in 4 cases (66.7%). The sensitivity, specificity, positive predic⁃tive value, negative predictive value and accuracy of ultrasound were 85.9%, 66.7%, 94.8%, 40.0% and 83.6%. The sensitiv⁃ity, specificity, positive predictive value, negative predictive value and accuracy of contrast- enhanced ultrasound were 92.2%, 77.8%, 96.7%, 58.3% and 90.4%. Conclusion Contrast-enhanced ultrasound can be used in benign and malignan⁃cy identification of renal cystic lesion.
Key words:kidney neoplasms;ultrasonography, doppler;cystic renal cell carcinoma;contrast-enhanced ultrasonogra⁃phy techniques; sensitivity and specificity
中图分类号:R445.19
文献标志码:A
DOI:10.11958/58950
作者简介:忻晓洁(1964),副主任医师,学士学位,主要从事超声诊断方面研究
