关节上下腔注射透明质酸联合稳定性咬合板治疗颞下颌关节盘不可复前移位的对比研究
2016-05-30尹小朋龚忠诚宁晓婷克热木阿巴斯胡露露林兆全
杨 萌, 尹小朋, 龚忠诚, 宁晓婷, 王 玥, 胡 鑫, 刘 慧, 克热木·阿巴斯, 凌 彬,邵 博, 胡露露, 林兆全
(新疆医科大学第一附属医院颌面肿瘤外科, 乌鲁木齐 830054)
关节上下腔注射透明质酸联合稳定性咬合板治疗颞下颌关节盘不可复前移位的对比研究
杨萌, 尹小朋, 龚忠诚, 宁晓婷, 王玥, 胡鑫, 刘慧, 克热木·阿巴斯, 凌彬,邵博, 胡露露, 林兆全
(新疆医科大学第一附属医院颌面肿瘤外科, 乌鲁木齐830054)
摘要:目的探讨关节上腔注射和关节下腔注射透明质酸(hyaluronic acid,HA)联合稳定性咬合板(stable biteplate,SBP)在治疗颞下颌关节盘不可复性前移位中的应用及其疗效。方法62例颞下颌关节盘不可复性前移位患者中,4例未完成治疗,58例患者随机分为两组:A组(27例)给予关节上腔注射HA联合稳定性咬合板,B组(31例)给予关节下腔注射HA联合稳定性咬合板,比较两组患者治疗前、后最大开口位(MMO)和关节压诊(JP)指数的变化。结果A、B组治疗3个月后较同组治疗前的最大开口位、关节压诊指数明显改善,差异有统计学意义(P<0.05)。治疗3个月后,B组最大开口位和关节压诊指数改善较A组明显,差异有统计学意义(P <0.05)。A、B组患者颞下颌关节症状及功能随着治疗次数的增加而改善。结论关节上下腔注射HA联合稳定性咬合板对于治疗颞下颌关节盘不可复性前移位均有良好的效果,关节下腔注射HA联合稳定性咬合板治疗效果优于关节上腔注射HA联合稳定性咬合板。
关键词:颞下颌关节; 透明质酸; 稳定性咬合板; 关节腔注射
不可复性关节盘前移位(anterior disc displacement without reduction, ADDw/oR)是一种常见的颞下颌关节紊乱病(temporomandibular disorders,TMD),临床症状包括疼痛、关节杂音、张口受限、下颌运动异常等,严重影响患者的进食、言语功能及生活质量。玻璃酸钠(hyaluronic acid,HA)是关节滑液的组成部分,其物理性质和功能已经明确[1-2]。近年来关节腔内注射HA治疗颞下颌关节紊乱病取得良好的效果,受到大家的关注。咬合板有多种优点,可用于治疗多种颞下颌关节紊乱病,缓解各种症状[3-5],是一种无创的治疗方法,可作为早期或长期治疗颞下颌关节紊乱病的手段[6-7]。本研究通过最大开口位和关节压诊指数,对经不同关节腔注射方法联合稳定性咬合板治疗颞下颌关节盘不可复性前移位患者的疗效进行评价,为临床治疗提供参考依据。
1资料与方法
1.1一般资料选择2013年9月-2014年7月就诊于新疆医科大学第一附属医院颞下颌关节门诊的TMD患者62例,其中4例患者第一次就诊后未复诊,58例患者完成治疗,男性8例,女性50例,年龄13~61岁,病程为2 w~16个月。随机分为两组:A组(27例)给予关节上腔注射HA联合稳定性咬合板,B组(31例)给予关节下腔注射HA联合稳定性咬合板。A组平均年龄(26.96±11.86)岁,女性23例(85.19%),病程(4.67±4.29)个月,最大开口度(27.78±5.86)mm,关节压诊指数(1.78±0.85);B组平均年龄(29.16±12.00)岁,女性27例(87.10%),病程(3.65±3.45)个月,最大开口度(27.42±6.12)mm,关节压诊指数(1.81±0.91),两组治疗前一般情况均衡可比,差异无统计学意义。
1.2纳入标准所有患者均由1名颞下颌关节医师初步检查,根据病史(疼痛史、关节弹响史)、临床表现(开口度,开口型等)、影像学检查(开闭口侧位断层片、CBCT、 MRI)诊断为颞下颌关节盘不可复性前移位,患者近1个月内未采用其他治疗方法,58例均建立完整的病历资料。
1.3治疗方法每2周治疗1次,3次为1个疗程,每次治疗后均遵照医嘱严格佩戴稳定咬合板,每次复诊时、治疗3个月后评价疗效。
1.3.1A组行关节上腔注射,患者靠于治疗椅,头侧位,耳前区常规皮肤消毒,患者呈半张口,进针点为耳屏前与髁突之间的凹陷区,进入皮肤后向前、上、内进针2~2.5 cm达骨面后稍后退,注入2%盐酸利多卡因,如位置准确,推注时省力,可回抽,反复灌洗后注入透明质酸钠约2.0 mL,缓慢退出针头,棉球按压5 min。
1.3.2B组操作如前,患者小张口,同时前伸下颌,于耳屏前与髁突后方之间凹陷下约2 mm处进针,相当于髁突顶后方,向前刺入达髁突后斜面,退约1 mL,患者张闭口数次,针头可随髁突运动,分别经2%盐酸利多卡因灌洗后,推入约2.5 mL透明质酸钠,棉球按压5 min。
1.4疗效评价[8-10]治愈:开口度、开口型正常,下颌运动正常,开闭口时无关节弹响,关节区及周围肌群无压痛。 显效:开口度为3~3.4 cm,开口型正常,下颌运动正常,无关节弹响,疼痛消失。好转:开口度<3 cm,开口型正常,无关节弹响,无疼痛,关节区域及关节周围肌群偶有压痛。无效:患者临床症状及体征无任何改变。
1.5统计学处理采用SPSS17.0软件对数据进行处理,组内数据比较使用配对t检验,组间数据比较使用独立样本t检验,P<0.05为差异有统计学意义。
2结果
2.1治疗前后最大开口度和关节压诊指数的比较治疗3个月后,A、B组最大开口度均较治疗前明显增大,差异有统计学意义(P<0.05),关节压诊指数较治疗前均明显减小,差异有统计学意义(P<0.05)。治疗3个月后关节下腔较关节上腔的最大开口度和关节压诊指数改善明显,差异有统计学意义(P<0.05)(表 1)。

表1 治疗前后最大开口度和关节压诊指数的比较(±s)
注:与同组治疗前比较,*P<0.05; 与A组比较,#P<0.05。
2.2两组患者治疗效果比较A、B组患者颞下颌关节症状及功能随着治疗次数的增加而改善,治疗3个月后A组显效19例(70.37%),治愈3例(11.11%),B组显效24例(77.42%),治愈7例(22.58%)(表 2)。
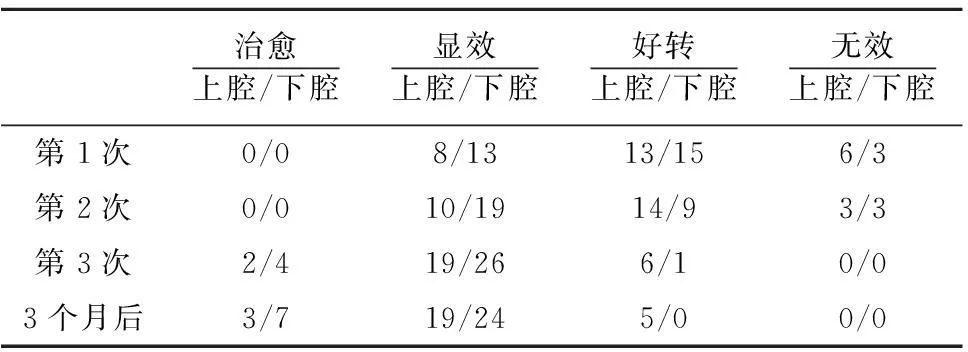
表2 两组患者治疗效果比较/例
3讨论
颞下颌关节盘不可复性前移位(ADDw/oR)是指关节盘与髁状突位置关系的异常,开闭口位时关节盘均停留在髁状突横嵴的前方,导致下颌运动时关节盘受挤压,长此以往发生变形使髁突不能正常地滑动和转动,临床表现为开口度下降和关节区肌肉组织疼痛。尽管不治疗关节盘不可复性前移位,其主诉和症状可减轻或自愈,但关节盘和髁状突的病理改变不会自愈,下颌运动时关节盘反复受到髁状突运动的推挤可致双板区或关节盘附着牵拉损伤,甚至穿孔。TMD的治疗目的是减轻疼痛、恢复功能、提高生活质量[11]。目前主要采用的治疗方法包括咬合导板[12]、关节腔药物注射[13]、激光[14]等方式。
对于颞颌关节紊乱病的影像学诊断,CBCT具有多平面观察、低放射剂量的优点,被认为是一个非常有潜力的诊断方法,而对于软组织的改变,MRI则是首选[15-16]。
本研究对于病人进行关节的开闭口侧位断层片常规的影像学检查,同时结合病人病史、临床检查做出综合判断,对于不能明确诊断的再行进一步影像学检查,通过患者开闭口位,能够对下颌运动时髁状突的位置、髁状突的骨质变化得到一个较为客观的评价,同时因其花费低、辐射剂量小,对于病人是较为理想的选择。
稳定性咬合板能够覆盖上颌或下颌全牙弓,咬合板平面与对颌后牙接触,通过不断调整咬合板的牙合平面重建稳定的下颌位置,消除牙合干扰,使下颌处于一个最佳的生理位置,通过放松肌肉,重新分配牙合力,又不会对牙齿造成伤害,可对关节腔注射治疗起到很好的巩固作用[17-18]。同时,咬合板能够增加关节腔的间隙,减少髁突表面的压力,创造有利于关节盘回弹的条件。研究表明颞下颌关节内压高是导致关节腔内滑液成分改变的原因,能够导致关节炎和关节的内部紊乱[19]。有关研究认为牙合垫的应用能够分解关节压力,改善关节的功能[20-23]。
瑞典的Kopp等[24-25]最早报道HA用于治疗颞下颌关节病取得治疗的效果。HA抗炎作用通过抑制吞噬作用、趋化作用、前列腺素的合成、金属蛋白酶的活性、清除滑膜组织上的氧自由基实现[26-27]。同时,HA还具有润滑、缓冲、营养、抗炎及软骨修复的作用,通过注射HA能够在组织表面形成一层保护膜,改变关节腔内压,减少摩擦。有研究显示单纯关节下腔或关节上腔联合下腔注射HA比单纯关节上腔注射HA治疗颞颌关节紊乱病疗效更好[28-29]。关节下腔注射可通过改变关节腔内压力,解除关节盘吸效应,对于症状的改善优于关节上腔治疗。颞下颌关节下腔体积较上腔小,下腔注射相较于上腔注射技术上更难掌握,需要具有丰富经验的临床医师操作。本研究显示在治疗中,用2%盐酸利多卡因盥洗,不仅可稀释患者关节腔内的炎性介质,同时利多卡因能够减轻患者治疗过程的疼痛,当颞颌关节紊乱发生时,关节腔内大分子量的HA变为小分子量的HA,因而造成滑液的粘弹性明显下降,使用分子量为80万~120万ku的大分子量的HA,很好地弥补了关节腔中损失大分子的HA。
本研究结果显示,58例患者在经过1个疗程的治疗后,患者的临床症状得到明显改善,随着治疗次数的增加,治疗效果也越来越明显,差异有统计学意义(P<0.05)。通过比较治疗前、后的最大开口位和关节压诊指数,认为关节下腔注射HA联合稳定性咬合板在提高患者开口度及减轻患者疼痛方面优于单纯上腔注射HA联合稳定性咬合板的治疗方法。
总之,应用透明质酸钠关节下腔注射联合稳定性咬合板能够改善患者开口度及疼痛症状,疗效肯定,值得推广。
参考文献:
[1] Takahashi T, Tominaga K, Takano H, et al. A decrease in the molecular weight of hyaluronic acid in synovial fluid from patients with temporomandibular disorders[J]. J Oral Pathol Med, 2004, 33(4):224-229.
[2] Guarda-Nardini L, Stifano M, Brombin C, et al. A one-year case series of arthrocentesis with hyaluronic acid injections for temporomandibular joint osteoarthritis[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2007, 103(6):e14-e22.
[3] Ekberg E, Nilner M. Treatment outcome of appliance therapy in temporomandibular disorder patients with myofascial pain after 6 and 12 months[J]. Acta Odontol Scand, 2004, 62(6):343-349.
[4] Wahlund K, List T, Larsson B. Treatment of temporomandibular disorders among adolescents: a comparison between occlusal appliance, relaxation training, and brief information[J]. Acta Odontol Scand, 2003, 61(4):203-211.
[5] Wassell RW, Adams N, Kelly PJ. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: one-year follow-up[J]. J Am Dent Assoc, 2006, 137(8):1089-1098.
[6] Yatani H, Minakuchi H, Matsuka Y, et al. The long-term effect of occlusal therapy on self-administered treatment outcomes of TMD[J]. J Orofac Pain, 1998, 12(1):75-88.
[7] Ekberg E, Vallon D, Nilner M. The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial[J]. J Orofac Pain, 2003, 17(2):133-139.
[8] Fricton JR, Schiffman EL. Reliability of a craniomandibular index[J]. J Dent Res, 1986, 65(11):1359-1364.
[9] Fricton JR, Schiffman EL. The craniomandibular index: validity[J]. J Prosthet Dent, 1987, 58(2):222-228.
[10]Helkimo M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state[J]. Svensk Tandlakare Tidskrift Swedish Dental Journal, 1974,67(2):101-121.
[11]Barak S, Katz J. Pain and dysfunction of the temporomandibular joint: etiology and treatment[J]. Harefuah, 1992, 123(12):545-547.
[12]Nagata K, Maruyama H, Mizuhashi R, et al. Efficacy of stabilisation splint therapy combined with non-splintmultimodal therapy for treating RDC/TMD axis I patients: a randomised controlled trial[J]. J Oral Rehabilit, 2015,42(12):890-899.
[13]Lu J, Long X, Deng M, et al. Treatment of temporomandibular joint disc perforation with injection of hyaluronic acid or disc repair[J]. Chin J Stomatol, 2014, 49(8):476-480.
[14]Nabeel S, Murugavel C, Gnanam A. Management of temporomandibular disorders with low level laser therapy[J]. J Maxillofac Oral Surg, 2014,13(4):444-450.
[15]Ahmad M, Hollender L, Anderson Q, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009, 107(6):844-860.
[16]Sinha V, Pradhan H, Mohammad S, et al. Efficacy of plain radiographs, CT scan, MRI and ultra sonography in temporomandibular joint disorders[J]. Nat J Maxillofac Surg, 2012,3(1):2-9.
[17]Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009, 107(2):212-223.
[18]Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances. Evidence of their efficacy[J]. J Am Dent Assoc, 2001, 132(6):770-777.
[19]Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment[J]. J Dent Res, 2008, 87(4):296-307.
[20]Dao TT, Lavigne GJ. Oral splints: the crutches for temporomandibular disorders and bruxism[J]. Crit Rev Oral Biol Med, 1998, 9(3):345-361.
[21]Levick JR. An investigation into the validity of subatmospheric pressure recordings from synovial fluid and their dependence on joint angle[J]. J Physiol (Lond), 1979, 289(1):55-67.
[22]Okeson JP. Joint intracapsular disorders: diagnostic and nonsurgical management considerations[J]. Dent Clin North Am, 2007, 51(1):85-103.
[23]Sanders B. Management of internal derangements of the temporomandibular joint[J]. Semin Orthod, 1995, 1(4):244-257.
[24]Kopp S, Wenneberg B, Haraldson T, et al. The short-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint pain and dysfunction[J]. J Oral Maxillofac Surg, 1985,43(6):429-435.
[25]Kopp S, Carlsson GE, Haraldson T, et al. Long-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint arthritis[J]. J Oral Maxillofac Surg, 1987, 45(11):929-935.
[26]Tuncel U. Repeated sodium hyaluronate injections following multiple arthrocenteses in the treatment of early stage reducing disc displacement of the temporomandibular joint: a preliminary report[J]. J Cranio Maxillofac Surg, 2012, 40(8):685-689.
[27]Basterzi Y, Sari A, Demirkan F, et al. Intraarticular hyaluronic acid injection for the treatment of reducing and nonreducing disc displacement of the temporomandibular joint[J]. Ann Plast Surg, 2009, 62(3):265-267.
[28]Smolka W, Iizuka T. Arthroscopic lysis and lavage in different stages of internal derangement of the temporomandibular joint: correlation of preoperative staging to arthroscopic findings and treatment outcome[J]. J Oral Maxillofac Surg, 2005, 63(4):471-478.
[29]Li C, Long X, Deng M, et al. Osteoarthritic changes after superior and inferior joint space injection of hyaluronic acid for the treatment of temporomandibular joint osteoarthritis with anterior disc displacement without reduction: acone-beam computed tomographic evaluation[J]. J Oral Maxillofac Surg, 2015, 73(2):232-244.
(本文编辑王艳)
The comparsion between superior and inferior joint space injections of hyaluronic acid (HA) combined with stable biteplate in the treatment of patient with temporomandibular joint (TMJ) anterior disc displacement without reduction(ADDw/oR)
YANG Meng, YIN Xiaopeng, GONG Zhongcheng,NING Xiaoting, WANG Yue, HU Xin, LIU Hui,Keremu Abass, LING Bin, SHAO Bo, HU Lulu, LIN Zhaoquan
(OncologicalDepartmentofOral&MaxillofacialSurgery,theFirstAffiliatedHospitalofXinjiangMedicalUniversity,Urumqi830054,China)
Abstract:ObjectiveTo explore the effect of superior and inferior joint space injections of hyaluronic acid (HA) combined with stable biteplate (SBP) in therapy of patients diagnosed with temporomandibular joint (TMJ) anterior disc displacement without reduction (ADDw/oR). MethodsSixty-two patients with ADDw/oR were randomly divided into two groups. Four cases did not complete the treatment. Group A (27 cases) received superior joint space injection of HA combined with SBP, Group B (31 cases) received inferior joint space injection of HA combined with SBP, MMO and JP were detected before treatment and at 3 mouths after treatment. The data was processed using SPSS17.0 software package. ResultsAt 3 months after treatment, In the groups A and B, MMO improved significantly compared with before treatment, and JP decreased significantly relative to before (P<0.05). At 3 months after treatment,group B compared with group A, MMO and JP were significantly improved. A, B two groups of patients with temporomandibular joint symptoms and function with the increase in the number of treatment to improve. ConclusionSuperior and inferior joint space injections of HA combined with SBP were effective methods for the treatment of patients with ADDw/oR. The injection of HA within the inferior joint space combined with SBP has a better effect.
Keywords:temporomandibular joint; hyaluronic acid; stable biteplate; intra-articular injections
[收稿日期:2015-11-20]
doi:10.3969/j.issn.1009-5551.2016.05.021
中图分类号:R782.6
文献标识码:A
文章编号:1009-5551(2016)05-0611-04
作者简介:杨萌(1989-),男,在读硕士,研究方向:颞下颌关节疾病基础与临床。通信作者:龚忠诚,男,博士,副教授,硕士生导师,研究方向:颞下颌关节疾病基础与临床,E-mail:gump0904@aliyun.com。
基金项目:国家自然科学基金(31260229); 新疆维吾尔自治区青年科技创新人才培养工程项目(2014721046)
