唐氏综合征患儿先天性心脏病术后并发症和预后的病例对照研究
2015-04-20刘成军茅思远符跃强
刘成军 茅思远 符跃强 白 科 许 峰
·论著·
唐氏综合征患儿先天性心脏病术后并发症和预后的病例对照研究
刘成军 茅思远 符跃强 白 科 许 峰
目的 探讨唐氏综合征(DS)患儿先天性心脏病(先心病)术后的并发症及预后。方法以 2009年1月1日至2013年6月30日DS先心病术后患儿为DS组,选择同期非DS先心病术后患儿作为对照组。两组根据先心病类型分别分为简单和复杂型先心病亚组。比较两组患儿临床特征、术后并发症及预后。结果DS组和对照组分别纳入77例,两组年龄、性别构成、体重和先心病类型差异均无统计学意义。DS组简单先心病亚组46例(59.7%),复杂先心病亚组31例;对照组简单先心病亚组47例(61.0%),复杂先心病亚组30例。DS组机械通气时间和ICU住院时间较对照组明显延长(P均<0.05),低心排综合征、再插管、肺部感染和肺动脉高压的发生率较对照组亦明显增高(P均<0.05);病死率也高于对照组(6.5%vs1.3%),但差异无统计学意义(P=0.096)。DS组和对照组简单型先心病亚组并发症发生率及病死率差异均无统计学意义(P均>0.05)。DS组复杂型先心病亚组在机械通气时间、ICU住院时间、总住院天数较对照组相应亚组均明显延长,低心排综合征、肺动脉高压和肺部感染的发生率亦明显增高(P均<0.05),病死率DS组复杂型先心病亚组有增高趋向(12.9%vs3.3%,P=0.173)。结论DS不增加简单型先心病患儿术后并发症和病死率;但增加复杂型先心病术后并发症发生率的风险,有增加病死率的趋向。
唐氏综合征; 先天性心脏病; 术后并发症
唐氏综合征(DS)是最常见的一种染色体疾病,先天性心脏病(先心病)是其最常见的合并畸形。有资料显示,所有的先心病患儿中,有4%~10%伴有DS,而40%~60%的DS患儿合并有先心病[1]。在墨西哥,DS最常合并的先心病类型是动脉导管未闭(PDA)、室间隔缺损(VSD)和房间隔缺损(ASD);在欧美,房室间隔缺损(AVSD)是DS主要合并的先心病类型,可达40%~70%[1,2]。中国64.4%的DS患儿合并先心病,以间隔类缺损为主(87.0%),其中单纯ASD占15.4%,单纯VSD占9.7%,AVSD占14.6%,复合类间隔缺损占47.3%[3]。既往认为,DS合并先心病患儿预后不良,病死率较高,且术后住院时间长,易发生感染,增加病死率,常不考虑手术。但此类患儿若不手术治疗,肺动脉高压、肺部感染等并发症不易控制,反而影响患儿的生存质量。随着手术和监护技术的提高,手术不再是DS患儿的禁忌,并能显著提高其生存率[2,4,5]。但临床上关于DS患儿先心病术后并发症的发生率和预后,文献报道不一[2,6~10],有学者认为DS患儿先心病术后有较高的并发症风险,增加病死率[8,9];但近年来也有文献报道术后并不增加并发症发生率,不影响患儿的预后[2,6,7,10]。本研究通过病例对照研究设计,选取DS合并先心病术后患儿为DS组,以非DS先心病术后患儿为对照组,回顾性分析两组患儿的临床资料、并发症及病死率情况,探讨DS合并先心病患儿术后的预后。
1 方法
1.1 DS组纳入标准 ①2009年1月1日至2013年6月30日重庆医科大学附属儿童医院(我院)收治的先心病患儿;②行先心病手术治疗;③有特殊面容和(或)智力障碍等表现者;④经染色体检查确诊为DS。
1.2 对照组纳入标准 选择同期无特殊面容和智力障碍等表现的非DS先心病术后患儿,样本量与DS组1∶1匹配,年龄、先心病类型与DS组尽量匹配。
1.3 DS组和对照组共同排除标准 两组均排除急诊手术、延迟关胸、合并气道狭窄及其他类型遗传代谢疾病者。
1.4 亚组分析 考虑到各种先心病的解剖畸形、病理生理不同,手术方式不同,对临床预后的影响也不同[11],故本研究根据先心病类型[12]将DS组和对照组分别分为简单型先心病和复杂型先心病亚组。简单型先心病包括VSD、ASD和PDA,复杂型先心病包括完全性房室隔缺损(CAVSD)、法洛四联症(TOF)、右室双出口(DORV)、大动脉转位(TGA)和主肺动脉起源异常等。
1.5 肺动脉高压分度[13]根据心脏超声行肺动脉高压分度。轻度:肺动脉收缩压30~40 mmHg;中度:肺动脉收缩压~70 mmHg;重度:肺动脉收缩压>70 mmHg。先心病术后发生轻度以上肺动脉高压定义为术后肺动脉高压[2]。
1.6 资料截取 回顾性翻阅病史,截取以下临床资料用于本文分析:①性别、年龄、体重、诊断、肺动脉压、体循环时间和主动脉阻断时间;②术后ICU住院时间、总住院时间和机械通气时间;③术后并发症:包括低心排综合征(临床征象:窦性心动过速、少尿或无尿、肢端发凉、肝脏肿大、低血压、心脏骤停)、心律失常、肺部并发症(气胸、肺不张)、肺部感染、肺动脉高压、再次插管和肾功能不全(氮质血症或需要血液净化治疗);④预后。

2 结果
2.1 一般情况 研究期间我院共收治2 026例先心病术后患儿,其中经染色体检查确诊为DS患儿77例,包括简单型先心病亚组46例(ASD 7例,VSD 19例,VSD合并ASD 20例),复杂型先心病亚组31例(CAVSD 24例,TOF 5例,DORV 1例,主肺动脉起源异常1例)。同期选择77例非DS先心病患儿为对照组,其中简单型先心病亚组47例(ASD 4例,VSD 26例,VSD合并ASD 17例),复杂型先心病亚组30例(CAVSD 26例,TOF 4例)。DS组和对照组年龄、性别、体重和先心病类型差异均无统计学意义(表1)。
2.2 DS组与对照组临床特征和术后并发症比较 如表1所示,DS组术前肺动脉高压、体循环时间、主动脉阻断时间和总住院天数与对照组比较差异均无统计学意义(P均>0.05),术后机械通气时间和ICU住院时间较对照组明显延长(P均<0.05)。DS组术后低心排综合征、再插管、肺部感染和肺动脉高压的发生率较对照组明显增高(P均<0.05)。DS组死亡5例,其中2例因严重低心排综合征术后3 d内死亡,2例因多脏器功能衰竭死亡,1例因反复肺部感染并发急性呼吸窘迫综合征死亡。对照组1例因严重低心排综合征死亡。
2.3 简单型先心病和复杂型先心病亚组临床特征和术后并发症比较 如表1所示,DS组和对照组简单型先心病亚组在术后机械通气时间、ICU住院时间、总住院时间、并发症发生率及病死率上差异均无统计学意义(P均>0.05)。与对照组复杂型先心病亚组比较,DS组复杂型先心病亚组术后机械通气时间、ICU住院时间、总住院天数显著延长;低心排综合征、肺动脉高压和肺部感染的发生率明显增高(P均<0.05);病死率有增高的趋向(12.9%vs3.3%,P=0.173)。


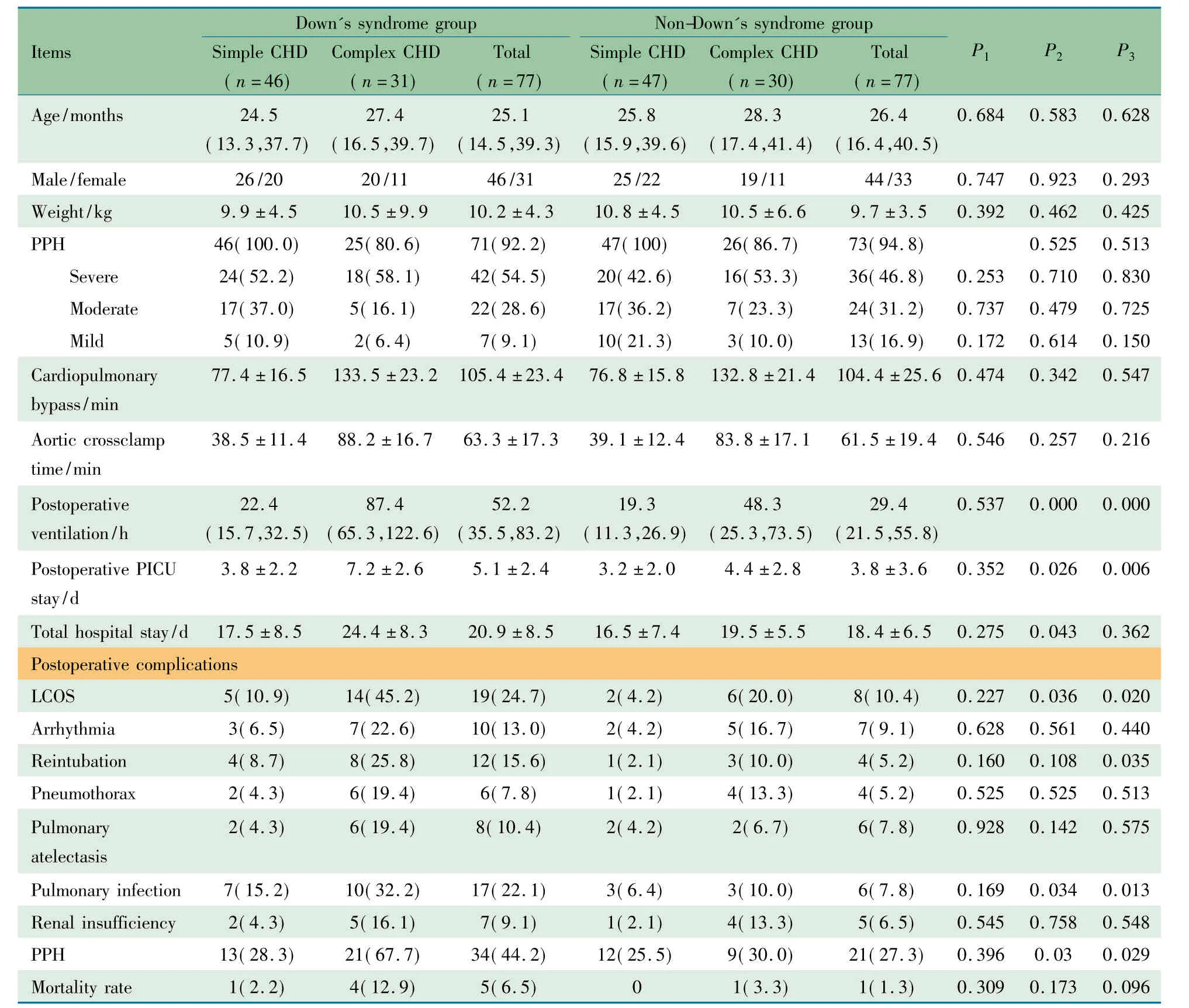
NotesP1: Comparisons of simple CHD betweetn DS and control groups;P2: Comparisons of complex CHD between DS and control groups;P3: Comparisons of total CHD between DS and control groups; PPH: Preoperative pulmonary hypertension; LOCS: Low cardiac output syndrome
3 讨论
虽然近年来DS患儿存活率明显增高,但总病死率是非DS患儿的5倍多,引起DS患儿死亡的主要原因是先心病和呼吸道感染[14,15]。DS合并先心病早期行矫治手术效果良好,手术风险无明显增加,且随着手术技术及治疗方法的改进,术后长期存活率明显提高,预期寿命延长[16,17],Al-Hay等[18]报道147 例CAVSD患儿中72%合并有DS,但与非DS患儿相比,DS并不增加手术的病死率,而且远期再手术率甚至还低于染色体检查正常的患儿。DS也不是手术的危险因素,与非DS患儿相比,DS患儿的心脏手术存活率和远期效果差异均无统计学意义[4]。国内资料显示,DS合并先心病术后病死率为2.9%,与同期先心病手术总体病死率(2.5%)相比仍然是可以接受的,而且中期随访结果也令人满意,表明手术治疗对于DS合并先心病患儿是安全有效的[19]。本文资料显示,DS组病死率略高于对照组,但两组差异无统计学意义,经亚组分析,两组简单型先心病亚组间病死率差异无统计学意义,但DS复杂型先心病亚组较对照组有增高趋向(12.9%vs3.3%)。
近年来有文献报道DS患儿先心病术后并不增加并发症发生率[10],但DS患儿存在免疫缺陷(主要表现为T淋巴细胞功能障碍)、生长发育落后、免疫力低下,可能合并肺血管梗阻性病变,多数文献报道术后早期仍有较高的并发症,其中最多见的是肺部感染[2,4]。Fudge等[2]研究发现,合并ASD、VSD和TOF的DS患儿住院时间较非DS患儿延长,肺部感染发生率增高。因肺部感染的发生率增加,DS患儿先心病术后机械通气和ICU住院时间明显延长[2,20],继而导致呼吸机相关性肺炎(VAP)的发生[21]。Van Trotsenburg等[7]报道DS患儿心脏手术后呼吸道感染的发生率为34%,且常发展为败血症,成为术后早期死亡的重要原因。咳嗽反射减弱、分泌物增多和胃食管反流等是导致DS先心病术后肺部感染的重要因素[14],同时也导致气管插管拔管失败的概率增大,再插管率增加。本文资料显示,DS组术后机械通气时间和ICU住院时间较对照组明显延长,肺部感染发生率明显高于对照组(22.1%vs7.8%),经亚组分析,DS组复杂型先心病亚组术后机械通气时间、ICU住院时间、肺部感染发生率明显高于对照组相应亚组,而在简单型先心病两亚组差异无统计学意义。因此术后要加强呼吸道管理,无菌操作,防止VAP的发生,并根据病原学结果选择敏感抗生素控制肺部感染,尽量缩短病程。
DS合并先心病的心脏畸形通常较复杂,多为复合畸形,容易早期形成肺动脉高压,甚至发生艾森曼格综合征,其原因大致分为2个方面:一方面是由于心脏结构畸形引起的心内分流,肺小动脉血流量增加,早期肺动脉呈反射性痉挛,肺循环阻力增加,肺动脉压升高[22];另一方面是DS合并先心病患者存在肺组织发育不全,主要表现为肺腺泡发育不全和残留双重肺毛细血管网,导致早期出现不可逆的肺血管病变,并呈进行性发展,加重肺动脉高压[23,24]。早期介入治疗或外科手术对肺动脉高压均有明显改善作用[3],避免发生艾森曼格综合征而失去手术机会。本文DS组与对照组术前肺动脉高压的发生率差异无统计学意义,也未发现艾森曼格综合征的患儿,这与患儿手术年龄较小,早期手术干预有关。本文2组患儿术后肺动脉高压发生率均明显下降,但术后DS组肺动脉高压的发生率明显高于对照组(44.2%vs27.3%,P<0.05),国外文献也有类似报道[2,25]。经亚组分析,DS组复杂型先心病亚组术后肺动脉高压的发生率明显高于对照组相应亚组,而在简单型先心病两亚组术后肺动脉高压的发生率差异无统计学意义。术后肺动脉高压也可能与手术持续时间、体外循环时间和先心病复杂程度有关。部分患儿体外循环心内直视手术后易发生反应性肺动脉高压,甚至肺高压危象,导致严重的低心排综合征,因此对于术前有重度肺动脉高压、或术后有肺动脉高压表现的患儿,术后要合理镇静、镇痛,中度过度通气,适宜氧合,维持PaCO2在30 mmHg左右(手术日),PaO290~100 mmHg,避免肺高压危象的发生,有条件可行肺动脉压监测[26],本文资料未发现体外循环术后肺动脉高压危象患儿。
低心排综合征是先心病特别是复杂型先心病术后较常见的并发症,也是导致患儿死亡的重要原因。目前认为可由多种原因引起,可能与患儿年龄、先心病类型、术前肺部感染、肺动脉高压程度、主动脉阻断时间和体外循环时间等因素有关[27,28]。有研究显示,DS患儿先心病术后左室心搏做功与舒张末期容积的比值稍低,左室射血分数较低,左室功能改善不显著[29],可能也是引起低心排综合征的原因之一。本研究发现,DS患儿较对照组术后更易发生低心排综合征(P=0.020),国外文献也有类似报道[2,25]。低心排综合征发生率在简单型先心病两亚组差异无统计学意义,但在复杂型先心病患儿中差异有统计学意义(P=0.036)。还有文献报道,DS患儿先心病术后易发生气胸、肺不张、心律失常和肾功能不全等[2],但本研究资料显示,两组上述并发症的发生率差异均无统计学意义。
综上所述,DS能增加复杂型先心病术后早期并发症发生率,并导致住院时间延长,有增高病死率的趋向;不增加简单型先心病术后的并发症发生率和病死率。
[1]de Rubens Figueroa J, del Pozzo Magaa B, Pablos Hach JL, et al. Heart malformations in children with Down syndrome. Rev Esp Cardiol, 2003, 56(9):894-899
[2]Fudge JC Jr, Li S, Jaggers J, et al. Congenital heart surgery outcomes in Down syndrome: analysis of a national clinical database. Pediatrics, 2010, 126(2): 315-322
[3]Xie X(谢雪), Zhang J. Correlative analysis between congenital heart diseases and Down′s syndrome. Chin J Appl Clin Pediatr(中华实用儿科临床杂志), 2014, 29(8):608-611
[4]Malec E, Mroczek T, Pajak J, et al. Results of surgical treatment of congenital heart defects in children with Down′s syndrome. Pediatr Cardiol, 1999, 20(5):351-354
[5]Reller MD, Morris CD. Is Down syndrome a risk factor for poor outcome after repair of congenital heart defects? J Pediatr, 1998, 132(4):738-741
[6]Calderon-Colmenero J, Flores A, Ramirez S, et al. Surgical treatment results of congenital heart defects in children with Down′s syndrome. Arch Cardiol Mex, 2004, 74(1):39-44
[7]van Trotsenburg AS, Heymans HS, Tijssen JG, et al. Comorbidity, hospitalization, and medication use and their influence on mental and motor development of young infants with Down syndrome. Pediatrics, 2006, 118(4):1633-1639
[8]Anaclerio S, Di Ciommo V, Michielon G, et al. Conotruncal heart defects: impact of genetic syndromes on immediate operative mortality. Ital Heart J, 2004, 5(8):624-628
[9]Seifert HA, Howard DL, Silbert JH, et al. Female gender increases the risk of death during hospitalization for pediatric cardiac surgery. J Thorac Cardiovasc Surg, 2007, 133(3):668-675
[10]Saffirio C, Marino B, Formigari R. Better surgical prognosis for patients with Down syndrome. J Thorac Cardiovasc Surg, 2008, 135(1):230
[11]Jenkins KJ, Gauvreau K, Newburger JW, et al. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg, 2002, 123(1):110-118
[12]Liu CJ(刘成军), Liu L, Xu F, et al. Analysis of influencing factors for capillary leak syndrome in children after cardiopulmonary bypass. Chinese Journal of Practical Pediatrics(中国实用儿科杂志), 2006, 21(10):753-755
[13]杨思源, 主编. 小儿心脏病学. 第三版. 北京:人民卫生出版社,2005.5
[14]Yang Q, Rasmussen SA, Friedman JM. Mortality associated with Down′s syndrome in the USA from 1983 to 1997: a population-based study. Lancet, 2002, 359(9311):1019-1025
[15]Day SM, Strauss DJ, Shavelle RM, et al. Mortality and causes of death in persons with Down syndrome in California. Dev Med Child Neurol, 2005, 47(3):171-176
[16]Kucik JE, Shin M, Siffel C, et al. Trends in Survival Among Children With Down Syndrome in 10 Regions of the United States. Pediatrics, 2013, 131(1):e27-36
[17]Frid C,Bjorkhem G, Jonzon A, et al. Long-tem survival in children with atrioventricular septal defect and common atrioventricular valvar orifice in Sweden. Cardiol Young, 2004, 14(1):24-31
[18]Al-Hay AA, MacNeill SJ, Yacoub M, et al. Complete atrioventricular septal defect, Down syndrome, and surgical outcome: risk factors. Ann Thorac Surg, 2003, 75(2):412-421
[19]Zhang WZ(张伟志), Yang YF, Huang C, et al. Impact of Down syndrome on the surgical treatment of congenital heart defects. J Cent South Univ(Med Sci)[中南大学学报(医学版)], 2012, 37(7):695-698
[20]Tibby SM, Durward A, Goh CT, et al. Clinical course and outcome for critically ill children with Down syndrome: a retrospective cohort study. Intensive Care Med, 2012, 38(8):1365-1371
[21]Gao HH(高海红), Yan LH, Zhang CY, et al. Risk factors of ventilator-associated pneumonia in infants and young children after open-heart surgery. Chin J Lung Dis(Electronic Edition)[中华肺部疾病杂志(电子版)], 2012, 5(3): 210-215
[22]Zheng Y(郑岩), Li BJ. Down综合征合并先天性心脏病肺动脉高压的特点. Med J Chin PLA(解放军医学杂志), 2007, 32(6): 650-651
[23]Galmbos C. Alveolar capillary dysplasia in a patient with Down′s syndrome. Pediatr Dev Pathol, 2006, 9(3):254-255
[24]Shehata BM, Abramowsky CR. Alveolar capillary dysplasia in an infant with trisomy 21. Pediatr Dev Pathol, 2005, 8(6):696-700
[25]Tóth R, Szántó P, Prodán Z, et al. Down syndrome and postoperative complications after paediatric cardiac surgery: a propensity-matched analysis. Interact Cardiovasc Thorac Surg, 2013, 17(4):691-697
[26]丁文祥,苏肇伉,主编. 小儿心脏外科重症临护手册. 北京:世界图书出版公司,2009.10
[27]Wang J(王进), Xu WJ, Wang MY, et al. 小儿先心病体外循环术后低心排出量综合征危险因素分析. Shandong Medical Journal(山东医药), 2008, 48(29): 46-47
[28]Song YH(宋云海), Xu ZM, Zhu LM, et al. Analysis of risk factors causing low cardiac output syndrome in patients with complicated congenital heart disease. Chin J Cardiovasc Rehabil Med(心血管康复医学杂志), 2008, 17(2): 145-148
[29]Kawaj T, wada Y, moto T, et a1.Comparison of hemodynamic data before and after corrective surgery for Down′s syndrome and ventricular septal defet.Heart Vessels, 1995, 10(3):154-157
(本文编辑:张萍)
The postoperative complications and prognosis of the children with Down′s syndrome undergoing congenital heart disease surgery: a case-control study
LIUCheng-jun,MAOSi-yuan,FUYue-qiang,BAIKe,XUFeng
(PICU,Children′sHospital,ChongqingMedicalUniversity,Chongqing400014,China)
FU Yue-qiang,E-mail:fuyueqiang@sina.com
ObjectiveTo explore the postoperative clinical characteristics, complications and prognosis of patients with Down′s syndrome(DS) undergoing congenital heart disease(CHD) surgery.MethodsChildren with DS undergoing CHD surgery between January 1, 2009 and June 30, 2013 were recruited as DS group, and children with non-DS undergoing CHD surgery in the same period were selected as the control group. The age and types of CHD in DS group and control group were matched. Two groups were all divided into simple CHD subgroup and complex CHD subgroup according to the type of CHD.The clinical characteristics, complications and prognosis of two groups were retrospectively analyzed.ResultsA total of 77 cases were enrolled in DS group and 77 cases in control group. The age, gender, bodyweight and types of CHD did not differ between DS group and control group.Ventilation duration, PICU stay, and the incidence of low cardiac output syndrome(LCOS),pulmonary infection, reintubation, pulmonary hypertension were much higher in DS group than those in control group [52.2(35.5-83.2) hvs29.4(21.5-55.8) h;(5.1±2.4) dvs(3.8±3.6) d,respectively, allP<0.05]. No statistically significant differences in in-hospital mortality rates were seen for patients in two groups(6.5% vs 1.3%,P>0.05). By hierarchical analysis, there was no significant difference in clinical characteristics, complications and mortality rates in DS and control group in simple CHD subgroup, but in complex CHD subgroup, ventilation duration, PICU stay, hospital stay [87.4(65.3-122.6) hvs48.3(25.3-73.5) h, (7.2±2.6) dvs(4.4±2.8) d, (24.4±8.3) dvs(19.5±5.5) d, respectively, allP<0.05)and the incidence of LCOS,pulmonary infection and pulmonary hypertension were much higher in DS group than those in control group (45.2%vs20.0%, 32.3%vs10.0%, 67.7%vs30.0%, respectively, allP<0.05). The mortality rate was higher in complex CHD of DS group than that in control group(12.9%vs3.3%,P>0.05).ConclusionDS did not increase mortality rate of children undergoing CHD surgery and had no effect on postoperative complications of simple CHD, but increased the risk of postoperative complications and mortality of complex CHD.
Down′s syndrome; Congenital heart disease; Postoperative complications
重庆医科大学附属儿童医院重症医学科 重庆,400014
符跃强,E-mail:fuyueqiang@sina.com
10.3969/j.issn.1673-5501.2015.03.005
2015-01-22
2015-05-20)