单侧颈内动脉闭塞患者脑灌注与症状、闭塞时期及闭塞位置的关系
2024-11-01张桂荣张妍妍梁文斌丁墩

摘要:目的" 评估单侧颈内动脉闭塞(ICAO)患者症状与脑灌注关系、闭塞时期及位置对脑灌注的影响。方法" 纳入2021年9月~2023年3月在西安交通大学第二附属医院神经内科就诊的符合纳入排除标准的16例ICAO患者,通过Dr Brain's软件动脉自旋标记模块计算区域脑血流量(CBF)。比较症状性及无症状ICAO、急性及慢性ICAO、起始部及颅内段闭塞患者全脑、双侧大脑中动脉供血区、大脑前动脉供血区、ASPECTS区域(尾状核、豆状核、岛带、内囊、M1、M2、M3、M4、M5、M6)、脑叶(额叶、顶叶、颞叶、岛叶)的区域脑血流量在标记后延迟时间(PLD)为1.5 s和2.5 s的差异。结果" 症状性及无症状、急性及慢性、起始部及颅内段ICAO患者全脑CBF、非闭塞侧半球各区域CBF在PLD 1.5 s 及 PLD 2.5 s的差异均无统计学意义(Pgt;0.05)。起始部和颅内段ICAO患者闭塞侧半球区域CBF在PLD 1.5 s及PLD 2.5 s的差异均无统计学意义(Pgt;0.05)。在PLD 1.5 s时,症状性ICAO患者闭塞侧M5区域CBF较无症状者明显降低,闭塞侧内囊CBF较无症状者升高(Plt;0.05);在PLD 2.5 s时,症状性及无症状ICAO患者各区域CBF的差异均无统计学意义(Pgt;0.05)。在PLD 1.5 s时,急性ICAO患者闭塞侧大脑中动脉、M1、M5及额叶区域CBF较慢性ICAO者降低(Plt;0.05);在PLD 2.5 s时,急性ICAO患者在闭塞侧大脑中动脉、M1、M5、M6及额叶的区域CBF较慢性ICAO者降低(Plt;0.05)。结论" 急性ICAO较慢性ICAO患者闭塞侧大脑中动脉供血区和部分ASPECTS皮质区域脑灌注受损更加严重,症状性ICAO与闭塞侧ASPECT部分区域灌注进一步受损有关,颈内动脉不同闭塞位置的脑灌注无差异。
关键词:动脉自旋标记;颈内动脉闭塞;脑血流量;缺血性卒中;血流动力学
Relationship between symptoms, occlusion period, and site with cerebral perfusion in patients with internal carotid artery occlusion
ZHANG Guirong, ZHANG Yanyan, LIANG Wenbin, DING Dun
Department of Medical Imaging, the Second Affiliated Hospital of Xi'an Jiaotong University, Xi'an 710004, China
Abstract: Objective To assess the relationship between symptoms and cerebral perfusion in patients with unilateral internal carotid artery occlusion (ICAO), and the influence of the occlusion period and location on cerebral perfusion. Methods Sixteen patients with ICAO who met the inclusion and exclusion criteria were enrolled in the Department of Neurology of the Second Affiliated Hospital of Xi'an Jiaotong University from September 2021 to March 2023. Regional cerebral blood flow (CBF) was measured by Dr Brain's software ASL module. Differences in regional CBF in global, middle cerebral artery (MCA) territory, anterior cerebral artery territory, Alberta Stroke Programme Early Computed Tomography Score (ASPECTS) regions (include caudate nucleus, lentiform nucleus, insula ribbon, internal capsule and M1-M6) and brain lobes (include frontal, parietal, temporal, insular lobe) of different subgroups (symptomatic and asymptomatic, acute and chronic, initial and intracranial ICAO) at PLD 1.5 s and PLD 2.5 s were evaluated. Results The CBF of symptomatic and asymptomatic, acute and chronic, initial and intracranial ICAO patients found no differences in the global and contralateral hemisphere at PLD 1.5 s and PLD 2.5 s (Pgt;0.05). The CBF of initial and intracranial ICAO patients found no differences in the ipsilateral hemisphere at PLD 1.5 s and PLD 2.5 s (Pgt;0.05). In the occluded hemisphere, the CBF of symptomatic ICAO was significantly lower than that of asymptomatic at PLD 1.5 s in M5, the CBF of symptomatic was significantly higher than that of asymptomatic at PLD 1.5 s in internal capsule (Plt;0.05). The CBF of symptomatic and asymptomatic ICAO found no differences in the ipsilateral hemisphere at PLD 2.5 s (Pgt;0.05). In the occluded hemisphere, the CBF of acute ICAO was significantly lower than that of chronic at PLD 1.5 s in middle cerebral artery territory, M1, M5, frontal lobe; the CBF of acute ICAO was significantly lower than that of chronic at PLD 2.5 s in middle cerebral artery territory, M1, M5, M6, frontal lobe (Plt;0.05). Conclusion Acute ICAO has further perfusion impairment than chronic ICAO in the middle cerebral artery territory and partly ASPECTS cortical areas of the occluded side. Symptomatic ICAO was associated with further perfusion impairment in partly ASPECT area of the occluded side. There was no significant difference in cerebral perfusion at different locations of internal carotid artery occlusion.
Keywords:" arterial spin labeling; internal carotid artery occlusion; cerebral blood flow; ischemic stroke; hemodynamic
动脉粥样硬化性颈内动脉闭塞(ICAO)是脑缺血事件的重要原因,栓塞和灌注不足是脑卒中的两个重要机制[1, 2] 。脑灌注成像是评估脑血流动力学变化的功能成像方法,三维动脉自旋标记(ASL)磁共振成像可实现脑血流量无创定量评估。临床上颈内动脉闭塞人群的临床症状、影像改变表现出巨大异质性,但相关ASL灌注研究较少;且既往研究采用单一标记后延迟时间(PLD)或手动绘制区域兴趣,使得脑血流量(CBF)测量耗时、费力。随着人工智能技术的发展,Dr Brain-ASL软件可以实现快速全脑和解剖区域脑血流定量测量。
颈内动脉闭塞包括急性和慢性闭塞,既往研究显示急性ICAO与临床预后差有关[3, 4] 。ICAO患者可出现不同的临床特征,从无症状到短暂性脑缺血发作(TIA)或急性严重卒中综合征[5] 。有症状ICAO患者的缺血性事件复发率为每年10%~18%,但无症状ICAO患者的复发率相对较低[6] 。ICAO可发生在任何节段,颅内段和颅外段颈内动脉闭塞具有不同的临床和影像学特征[7] 。闭塞部位是与预后不良相关的变量之一[8] 。Alberta卒中项目早期CT评分(ASPECTS)是一种简单可靠的定性评分系统,广泛用于评估早期缺血性脑梗死的严重程度,是血管内治疗决策的重要筛选标准[9-12] ,有助于预测治疗效果和预后。ASPECTS评分,现已从CT平扫延伸至MR的DWI/FLAIR等序列来进行梗死评分,脑灌注成像较常规序列能更早识别梗死及缺血区,但目前ASPECTS相关区域的灌注评价研究尚缺乏。本研究拟采用新CBF定量软件分析方法评估包括常规前循环脑区以及ASPECTS区域在内的脑灌注改变,旨在探讨ICAO患者的症状与脑灌注的关系,闭塞时期和闭塞部位对脑灌注影响,进一步细化ICAO患者脑灌注评估工作,为明确颈内动脉闭塞患者临床和影像特征异质性原因提供客观证据,加深临床医生对该类病变认识,进而指导临床决策,为后续研究提供基础。
1" 资料与方法
1.1" 一般资料
本研究经我院伦理学审批通过(审批号:2022156)。选择2021年9月~2023年3月在西安交通大学第二附属医院神经内科就诊的颈内动脉闭塞患者。纳入标准:行数字减影血管造影检查并确诊单侧ICAO的患者;同期行PLD 1.5 s、PLD 2.5 s的3D-pCASL成像。排除标准:对侧血管有中度或重度狭窄(≥50%);图像质量差或ASL使用单PLD或其它标记后延迟时间扫描;患有脑损伤/手术/精神疾病/其他影响大脑的疾病。
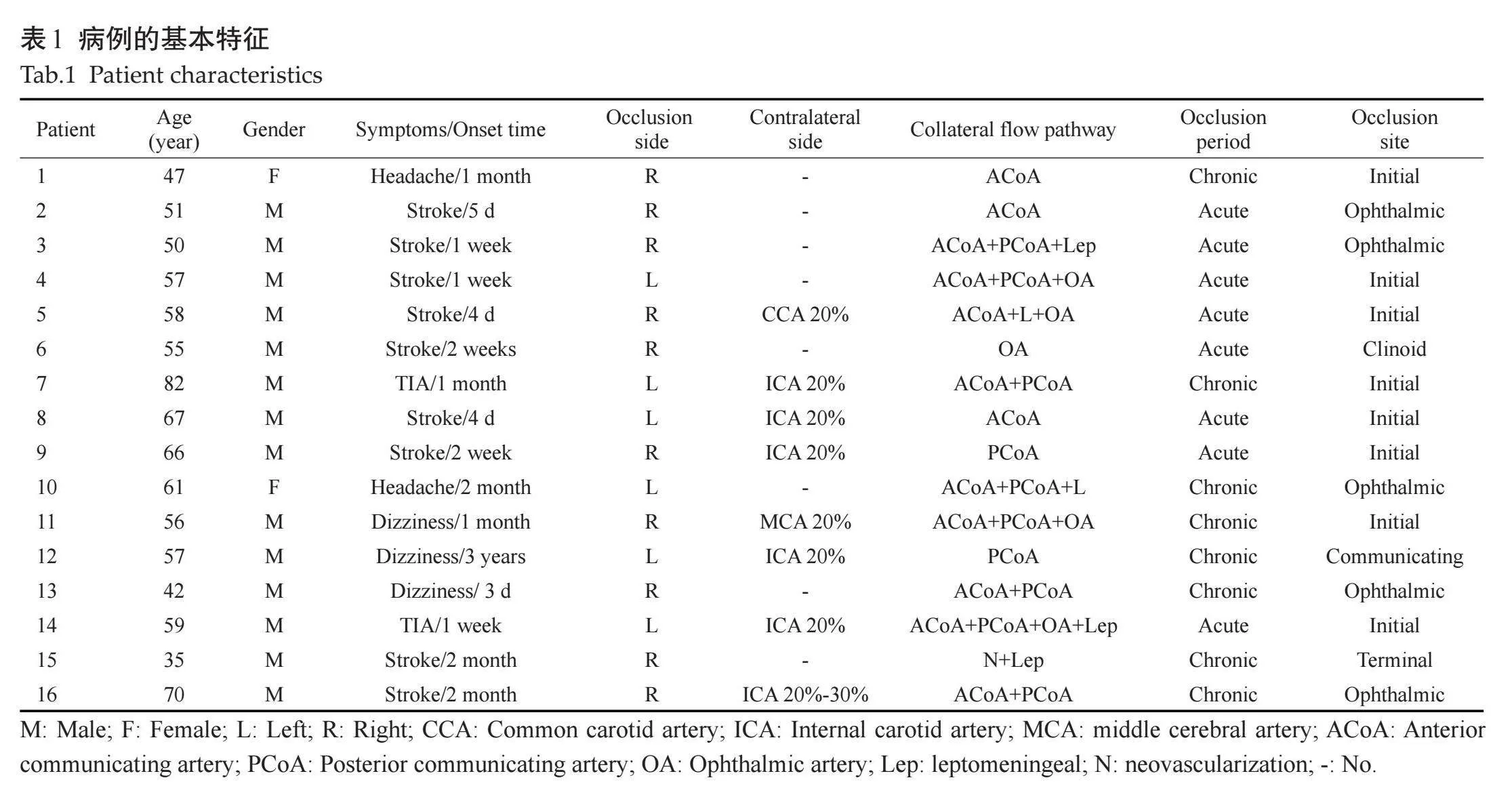
36例ICAO患者中,排除对侧头颈部血管狭窄程度大于50%患者10例,排除伴有癫痫和既往颅脑手术患者2例,排除单PLD患者8例。最终16例ICAO患者(2例女性和14例男性;年龄57.06±11.24岁)纳入本研究。患者分组如下:脑或视网膜缺血表现包括与同侧颈内动脉闭塞(ICA)相关的短暂性或非致残性症状,定义为有症状[13] ,否则定义为无症状患者,本组有症状ICAO患者11例,无症状ICAO患者5例。根据临床和影像学的相关证据,参考既往文献[14, 15] ,将闭塞时间小于1周定义为急性ICAO,大于4周定义为慢性ICAO,本组8例为急性ICAO,8例为慢性ICAO。根据闭塞部位,8例为颈内动脉起始部闭塞,8例为颈内动脉颅内段闭塞。各组间年龄、性别的差异无统计学意义(Pgt;0.05)。
1.2" MRI成像
全脑三维pCASL序列使用3.0T MR扫描仪(HDxt Signa,GE)扫描,配备8通道头部线圈用于信号采集。参数为:TR 4599 ms(PLD=1525 ms),TR 5294 ms(PLD=2525 ms),回波时间10.86 ms,标记时间1500 ms,视野24 cm×24 cm,层厚4.0 mm,36层,背景抑制。
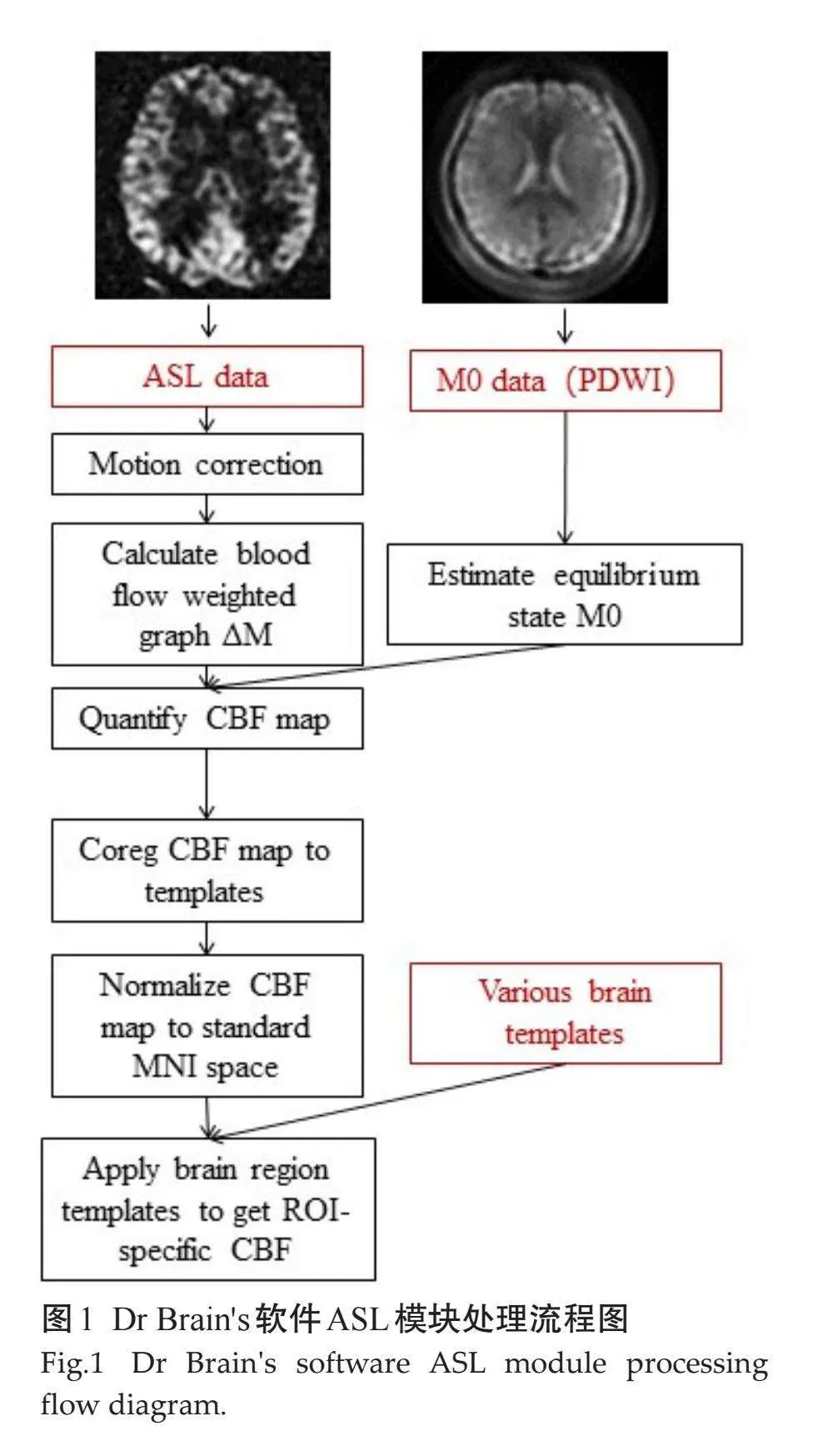
1.3" 数据分析
将ASL序列原始数据包(PLD 1.5 s和PLD 2.5 s)脱敏后上传至Dr Brain软件ASL模块(YIWEI医疗科技),基于Buxton血流动力学模型,血液T1和脑组织T1常数分别为1650 ms和1165 ms,处理流程(图1)。评估ICAO患者不同亚组的全脑、大脑前动脉(ACA)、大脑中动脉(MCA)供血区、ASPECTS区域(包括尾状核、状核、岛带、内囊和M1-M6)、额叶、顶叶、颞叶、岛叶区域CBF在不同PLD的差异。
1.4" 统计学分析
采用SPSS 21.0软件进行统计分析。所有计量数据均经Shapiro-Wilk进行正态性检验,符合正态分布的以均数±标准差表示,不符合正态分布的以中位数(四分位数间距)表示。数据符合正态分布且方差齐性,组间比较采用独立样本t检验,否则采用Mann-Whitney U检验。以Plt;0.05为差异有统计学意义。
2" 结果
2.1" 患者的临床资料
ICAO患者的基本特征(表1)。
2.2" 有症状和无症状ICAO患者区域CBF差异
有症状和无症状ICAO患者全脑CBF在PLD 1.5 s[23.312±4.803 vs 26.000±3.555 mL/(min·100 g),P=0.285]和PLD 2.5 s[28.457±5.338 vs 29.888±2.264 mL/(min·100 g),P=0.579]的差异无统计学意义。
在闭塞侧半球,PLD 1.5 s时,症状性ICAO患者M5区域CBF较无症状者降低[13.586±6.930 vs 22.176±4.929 mL/(min·100 g), P=0.026],内囊CBF较无症状者升高[25.861±3.122 vs 21.392±2.791 mL/(min·100 g),P=0.016],其它14个脑区的差异无统计学意义(Pgt;0.05);在PLD 2.5 s时,症状性和无症状ICAO患者16个区域CBF的差异无统计学意义(Pgt;0.05)。
在非闭塞侧半球,有症状和无症状ICAO患者在PLD=1.5 s和PLD=2.5 s时各区域CBF的差异无统计学意义(Pgt;0.05)。
2.3" 急性和慢性ICA闭塞区域CBF差异
急性和慢性ICAO患者在PLD 1.5 s[22.945±5.344 vs 25.359±3.440 mL/(min·100 g),P=0.301)]和PLD 2.5 s[27.411±6.003 vs 30.398±1.871 mL/(min·100 g),P=0.115]全脑CBF的差异无统计学意义。
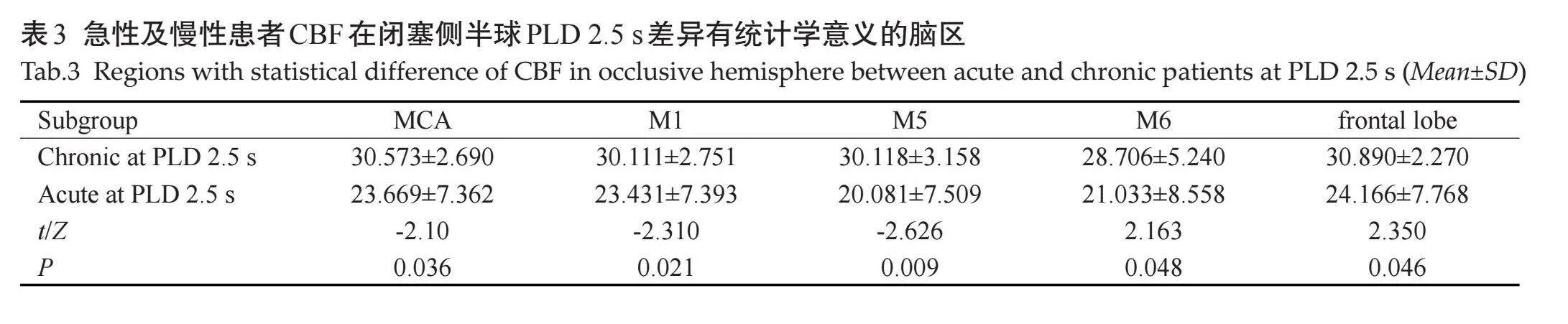
在闭塞侧半球,当PLD 1.5 s时,急性ICAO患者在MCA、M1、M5及额叶的区域CBF较慢性ICAO者降低(Plt;0.05,表2),但在其它12个脑区CBF的差异无统计学意义(Pgt;0.05);当PLD 2.5 s时,急性ICAO患者在MCA、M1、M5、M6及额叶的区域CBF较慢性ICAO者降低(Plt;0.05,表3),而在其它11个脑区CBF的差异无统计学意义(Pgt;0.05)。
在非闭塞侧半球,急性和慢性ICAO患者在PLD 1.5 s和PLD 2.5 s时各区域CBF的差异无统计学意义(Pgt;0.05)。
2.4" 颈内动脉起始部和颅内段闭塞区域CBF差异
起始部ICAO患者和颅内段ICAO患者全脑CBF在PLD 1.5 s[24.068±3.872 vs 23.676±5.287 mL/(min·100 g),P=0.943]和PLD 2.5 s[29.868±4.337 vs 27.941±4.868 mL/(min·100 g),P=0.417]的差异均无统计学意义。起始部和颅内段闭塞患者在PLD 1.5 s和PLD 2.5 s时,两侧半球所有脑区CBF的差异均无统计学意义(Pgt;0.05)。
3" 讨论
ICAO基于侧支血流的差异可以有不同的临床过程,从无症状到严重的神经功能不足[16] 。症状性ICAO的年发病率在一般人群中约为6/100 000人[17] 。本研究纳入ICAO患者中,68.75%(11/16)表现为有症状,31.25%(5/16)表现为无症状。症状性ICAO患者长期预后较差[13] ,卒中年复发率为5%~6%[13] ,脑血流动力学受损及侧支流严重的患者复发率为9%~18%[18-20] 。无症状性ICAO脑卒中复发率小于2%[19, 21] 。既往研究表明,无症状和有症状ICAO患者与对照组相比,闭塞侧ACA和MCA基线CBF均显著降低[22] 。然而,目前国内外尚无关于有/无症状ICAO患者脑血流量差异的对比研究。国内一项研究显示前循环大血管严重狭窄/闭塞患者,在PLD 1.5 s和PLD 2.5 s,有症状患者双侧半球脑CBF均低于无症状患者[23] 。本研究结果显示,在PLD 1.5 s时,有症状ICAO者较无症状者闭塞侧M5区CBF降低,非闭塞侧有/无症状患者CBF在双PLD时均无差异,提示ICA闭塞导致闭塞侧灌注行为异常,闭塞侧区域性脑灌注减低及延迟可能是患者症状出现的原因,但由于本文样本量有限,需要进一步的大样本研究来明确ICAO患者症状与脑区灌注不足关系。
急性ICAO与严重和持续的神经功能缺陷有关,对静脉溶栓无效,并预示着更可怕的临床结果[7, 24] 。慢性ICAO患者通常没有明显的临床症状,很多时候是常规影像学检查时偶然发现。本研究中,87.5%(7/8)的急性ICAO患者表现为缺血性卒中,12.5%(1/8)表现为TIA;62.5%(5/8)的慢性ICAO患者表现为头痛或头晕,25%(2/8)表现为卒中,12.5%(1/8)表现为TIA。当前的分析结果显示,在闭塞侧半球PLD 1.5 s和PLD 2.5 s时,急性ICAO患者部分MCA和ASPECTS皮质区域CBF明显低于慢性ICAO者,提示急性ICAO脑灌注受损更加严重,更低灌注是急性ICAO者脑缺血事件更高发病率的原因。这可能与急性ICA闭塞阻止了闭塞血管的侧支循环建立、调节和限制脑损伤的进展,慢性闭塞进展可能允许远端侧支血管的发育以避免严重的缺血事件发生有关[7] 。目前国内外尚无关于急性/慢性ICAO患者脑血流量差异的对比研究,本研究结果明确了急慢性期ICAO对脑灌注影响,认为判断ICA急慢性期闭塞对临床决策至关重要,随着ICA闭塞时间的延长,血栓逐渐纤维化,阻碍微导丝通过闭塞动脉,使其难以再通,增加并发症的风险[25] 。除了结合临床特征,高分辨MR血管壁成像在评估闭塞时期、闭塞位置及范围方面也有重要临床价值。
根据Bouthillier分类,颈内动脉的颅内外部分可分为7个节段[26]。由于近端血流动力学复杂,低剪切应力、血流停滞和血流分离,ICA闭塞在近端更常见[27] 。有研究注意到ICAO患者神经系统的严重程度和梗死面积从近端到远端不断增加[28] 。本研究结果显示,ICA起始部和颅内段闭塞患者的全脑CBF以及双侧半球区域CBF在PLD 1.5 s和PLD 2.5 s的差异均无统计学意义,提示颈内动脉的不同闭塞位置其脑灌注本质无明显差异。目前国内外尚无关于不同ICAO闭塞位置脑血流量差异的研究,本文小样本量也可能是导致其差异无统计学意义的原因。但ICA的闭塞位置对于血管内治疗至关重要,它可以帮助医生为患者选择合适的再通技术、支架或介入装置的大小[8] 。既往研究表明,ICA闭塞部位越低,再通成功率越高[29] 。此外,既往研究显示再通的维持基本依赖于闭塞位置,以颈内动脉床突段为界,其远端和近端再闭塞的年发生率分别为91%和0%[30] 。所以,闭塞位置评估对临床决策仍然具有重要意义。
综上所述,急性ICAO较慢性ICAO患者闭塞侧大脑中动脉供血区和部分ASPECTS皮质区域脑灌注受损更加严重;症状性ICAO与闭塞侧ASPECTS部分区域灌注进一步受损可能有关;颈内动脉不同闭塞位置的脑灌注无明显差异。本研究创新性地使用新技术实现更快速、细致全脑和区域CBF评估,首次评估了ICAO患者ASPECTS区域脑灌注,解决了临床实际问题,为后续的研究和临床治疗决策提供了理论基础。但本研究由于样本量有限,在将现有结果解释应用至其它人群时应谨慎,后续研究将继续扩大样本量。
参考文献:
[1]" "Rodda RA. The arterial patterns associated with internal carotid disease and cerebral infarcts[J]. Stroke, 1986, 17(1): 69-75.
[2]" "Saini H, Cerejo R, Williamson R, et al. Internal Carotid Artery Occlusion: Management[J]. Curr Neurol Neurosci Rep, 2022, 22(7): 383-8.
[3]" "Bhatia R, Hill MD, Shobha N, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real‑world experience and a call for action[J]. Stroke, 2010, 41(10): 2254-8.
[4]" "Paciaroni M, Inzitari D, Agnelli G, et al. Intravenous thrombolysis or endovascular therapy for acute ischemic stroke associated with cervical internal carotid artery occlusion: the ICARO-3 study[J]. J Neurol, 2015, 262(2): 459-68.
[5]" "Faught WE, van Bemmelen PS, Mattos MA, et al. Presentation and natural history of internal carotid artery occlusion[J]. J Vasc Surg, 1993, 18(3): 512-24.
[6]" "Powers WJ, Derdeyn CP, Fritsch SM, et al. Benign prognosis of never-symptomatic carotid occlusion[J]. Neurology, 2000, 54(4): 878-82.
[7]" "Malhotra K, Goyal N, Tsivgoulis G. Internal carotid artery occlusion: pathophysiology, diagnosis, and management[J]. Curr Atheroscler Rep, 2017, 19(10): 41.
[8]" "Morofuji Y, Horie N, Tateishi Y, et al. Arterial spin labeling magnetic resonance imaging can identify the occlusion site and collateral perfusion in patients with acute ischemic stroke: comparison with digital subtraction angiography[J]. Cerebrovasc Dis, 2019, 48(1/2): 70-6.
[9]" "Barber PA, Demchuk AM, Zhang J, et al. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score[J]. Lancet, 2000, 355(9216): 1670-4.
[10] Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke[J]. N Engl J Med, 2015, 372(11): 1019-30.
[11] Lloyd M. A randomized trial of intraarterial treatment for acute ischemic stroke[J]. J Emerg Med, 2015, 48(4): 521.
[12] Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke[J]. N Engl J Med, 2015, 372(24): 2285-95.
[13] Klijn CJ, Kappelle LJ, Algra A, et al. Outcome in patients with symptomatic occlusion of the internal carotid artery or intracranial arterial lesions: a meta‑analysis of the role of baseline characteristics and type of antithrombotic treatment[J]. Cerebrovasc Dis, 2001, 12(3): 228-34.
[14] Michel P, Ntaios G, Delgado MG, et al. CT angiography helps to differentiate acute from chronic carotid occlusion: the \"carotid ring sign\"[J]. Neuroradiology, 2012, 54(2): 139-46.
[15] Iwata T, Mori T, Tajiri H, et al. Long-term angiographic and clinical outcome following stenting by flow reversal technique for chronic occlusions older than 3 months of the cervical carotid or vertebral artery[J]. Neurosurgery, 2012, 70(1): 82-90.
[16]" Liebeskind DS, Flint AC, Budzik RF, et al. Carotid I’s, L’s and T’s: collaterals shape the outcome of intracranial carotid occlusion in acute ischemic stroke[J]. J Neurointerv Surg, 2015, 7(6): 402-7.
[17] Flaherty ML, Flemming KD, McClelland R, et al. Population-based study of symptomatic internal carotid artery occlusion: incidence and long-term follow-up[J]. Stroke, 2004, 35(8): e349-52.
[18]Grubb RL, Derdeyn CP, Fritsch SM, et al. Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion[J]." JAMA, 1998, 280(12): 1055-60.
[19] Vernieri F, Pasqualetti P, Passarelli F, et al. Outcome of carotid artery occlusion is predicted by cerebrovascular reactivity[J]. Stroke, 1999, 30(3): 593-8.
[20] Klijn CJ, Kappelle LJ, van Huffelen AC, et al. Recurrent ischemia in symptomatic carotid occlusion: prognostic value of hemodynamic factors[J]. Neurology, 2000, 55(12): 1806-12.
[21]" Bornstein NM, Norris JW. Benign outcome of carotid occlusion[J]. Neurology, 1989, 39(1): 6-8.
[22] Hartkamp NS, Petersen ET, Chappell MA, et al. Relationship between haemodynamic impairment and collateral blood flow in carotid artery disease[J]. J Cereb Blood Flow Metab, 2018, 38(11): 2021-32.
[23]" 谷家美, 王" 雁. 动脉自旋标记技术在前循环大血管严重狭窄/闭塞患者中的应用价值[J]. 临床医学进展, 2020, 6(7): 1269-76.
[24] Kwak JH, Zhao L, Kim JK, et al. The outcome and efficacy of recanalization in patients with acute internal carotid artery occlusion[J]. AJNR Am J Neuroradiol, 2014, 35(4): 747-53.
[25]" Xu BF, Liu R, Jiao LQ, et al. Carotid endarterectomy for in-stent restenosis: a case report and literature review[J]. Biomed Rep, 2017, 7(2): 128-32.
[26] Alain B, Van LHR, Keller JT. Segments of the internal carotid artery: a new classification[J]. Neurosurgery, 1996, 38(3): 425-32.
[27]Harrison MJ, Marshall J. The finding of thrombus at carotid endarterectomy and its relationship to the timing of surgery[J]. Br J Surg, 1977, 64(7): 511-2.
[28]Hong JM, Lee SE, Lee SJ, et al. Distinctive patterns on CT angiography characterize acute internal carotid artery occlusion subtypes[J]. Medicine, 2017, 96(5): e5722.
[29] Chen YH, Leong WS, Lin MS, et al. Predictors for successful endovascular intervention in chronic carotid artery total occlusion[J]. JACC Cardiovasc Interv, 2016, 9(17): 1825-32.
[30]" Lee CW, Lin YH, Liu HM, et al. Predicting procedure successful rate and 1‑year patency after endovascular recanalization for chronic carotid artery occlusion by CT angiography[J]. Int J Cardiol, 2016, 221: 772-6.
(编辑:林" 萍)