MRI诊断膝关节退行性病变的价值及影像学特征
2024-10-31李小军黎学兵陈钇地姚鹏杨早胡春阳龚艳
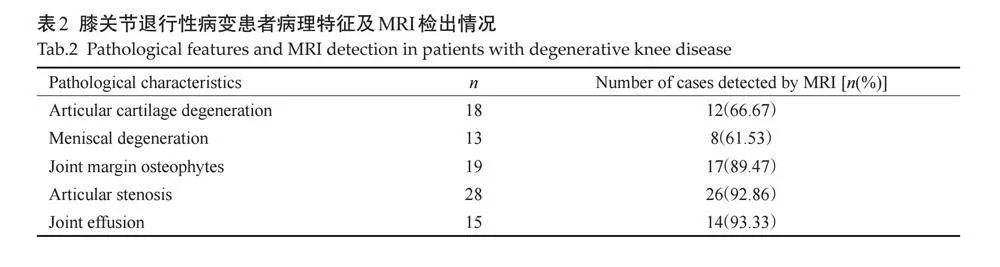
摘要:目的 "探讨膝关节退行性病变MRI影像学特征,并分析MRI定量指标对膝关节退行性病变的诊断价值。方法 "选择2019年2月~2023年4月湖北民族大学附属民大医院接诊的疑似膝关节退行性病变患者162例。患者检查前均先休息30 min后行MRI扫描,并对对内侧髁、外侧髁T1、T2、T2*值及髌骨脂肪含量(FF)值进行测量。在MRI扫描后1周内行膝关节镜检查,根据镜检结果是否符合膝关节退行性病变将患者分为观察组(n=93)与对照组(n=69)。比较2组各MRI指标,并以ROC曲线分析各指标单独检测与联合检测对膝关节退行性病变的诊断价值。结果 "MRI常规扫描对关节软骨变性检出率仅为66.67%,半月板退变检出率为61.53%。关节边缘骨质增生、关节腔隙狭窄、关节积液检出率较高,分别为89.47%、92.86%、93.33%。观察组患者内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF(%)均高于对照组,差异有统计学意义(Plt;0.05)。ROC分析结果显示内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF(%)对膝关节退行性该病诊断截断值分别为1018.92、39.27、22.34、994.71、39.91、22.74、79.18%,曲线下面积分别为0.911、0.892、0.619、0.813、0.904、0.917、0.791(Plt;0.05)。结论 "MRI常规扫描对关节软骨变性、半月板退变检出率较低,内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF(%)均可用于膝关节退行性病变的诊断。
关键词:膝关节退行性病变;MRI;诊断价值;ROC曲线分析
Value of MRI diagnosis of degenerative knee joint lesions and its imaging features
LI Xiaojun1, LI Xuebing1, CHEN Yidi2, YAO Peng1, YANG Zao1, HU Chunyang1, GONG Yan1
1Department of Radiology, Minda Hospital of Hubei Minzu University, Enshi 445099, China; 2Department of Radiology, West China Hospital, Sichuan University, Chengdu 610044, China
Abstract: Objective To explore the changes in MRI imaging features of degenerative lesions of the knee joint and analyze the diagnostic value of MRI quantitative indicators for it. Methods " A total of 162 patients with suspected degenerative lesions of the knee joint who were admitted to Minda Hospital, Hubei University for Nationalities from February 2019 to April 2023 were selected. Before examination, patients rested for 30 min before undergoing MRI scans, and measured the T1, T2, T2* values of the medial and lateral condyles, as well as the patellar fat fraction (FF) values. Knee arthroscopy was performed within 1 week after MRI scanning, and the patients were divided into observation group (n=93) and control group (n=69) according to whether the microscopic findings were consistent with degenerative lesions of the knee joint. The MRI indexes of the two groups were compared, and the diagnostic value of each index for degenerative lesions of the knee joint was analyzed by ROC curve. Results The detection rate of articular cartilage degeneration by routine MRI scanning was only 66.67%, and the detection rate of meniscus degeneration was 61.53%. The detection rates of hyperostosis at the joint margin, joint cavity stenosis, and joint effusion were 89.47%, 92.86%, and 93.33%, respectively. The medial condylar T1 value, medial condylar T2 value, medial condylar T2* value, lateral condylar T1 value, lateral condylar T2 value, lateral condylar T2* value and FF (%) of the patients in the observation group were higher than those in the control group, and the difference was statistically significant (Plt;0.05). ROC analysis results showed that the cutoff values of medial condylar T1, medial condylar T2, medial condylar T2*, lateral condylar T1, lateral condylar T2, lateral condylar T2* and FF for the diagnosis of degenerative lesions of the knee joint were 1018.92, 39.27, 22.34, 994.71, 39.91, 22.74, 79.18%, respectively, and the AUCs were 0.911, 0.892, 0.619, 0.813, 0.904, 0.917, 0.791 (Plt;0.05). Conclusion Routine MRI scanning has a low detection rate for articular cartilage degeneration and meniscus degeneration. The values of medial condyle T1, medial condyle T2, medial condyle T2*, lateral condyle T1, lateral condyle T2, lateral condyle T2* and FF (%) can be used for the diagnosis of degenerative lesions of the knee joint.
Keywords: degenerative lesions of the knee joint; MRI; diagnostic value; ROC curve analysis
膝关节退行性病变多因关节软骨损伤、磨损所致,在中老年人群中高发。膝关节退行性病变的病理机制涉及多个因素,最终导致软骨的损伤和退化,引发膝关节疼痛、重症、僵硬、活动受限等临床表现[1] 。因膝关节软骨缺少血管、淋巴、神经等的营养支持,在出现损伤后修复难度大,随着病情进展可引起关节畸形、功能障碍,最终致患者丧失基本生活能力[2-3] 。早期发现膝关节退行性病变,并指导临床及时采取保护、治疗措施有助于延缓病情,对于提高患者生活质量具有重要的价值。既往研究主要采用形态改变、关节间隙变化等MRI指标评估患者膝关节退行性病变情况,无法实现早期诊断,出现上述指标改变时患者多已病情较严重,失去了早期诊断的价值[4] 。近年研究发现MRI生理定量指标可及时发现软骨生化成分改变,并对软骨损伤程度进行定量评估[5] ;同时,MRI化学位移呈现还可通过测量骨髓脂肪含量变化而用于评估骨量减少情况(膝关节退行性病变与骨量减少密切相关)[6] 。但上述指标联合检测对膝关节退行性病变的诊断价值如何,目前尚无定论。本研究将上述指标进行联合检测以及早发现膝关节软骨早期损伤及骨量变化情况,通过分析上述MRI定量指标对膝关节退行性病变的诊断价值,旨在为膝关节退行性病变的早诊断、早干预、早治疗提供参考,现报道如下。
1 "资料与方法
1.1 "一般资料
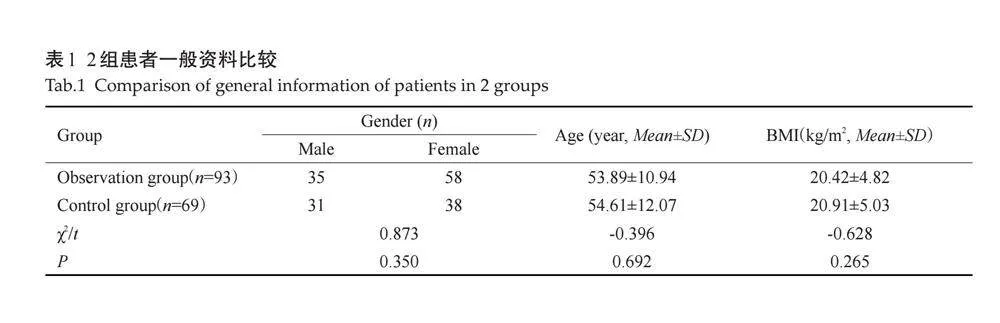
选择2019年2月~2023年4月湖北民族大学附属民大医院接诊的疑似膝关节退行性病变患者162例。纳入标准:有关节疼痛、肿胀、僵硬等疑似膝关节退行性病变的表现;患者意识清醒,可配合检查;患者已获知情同意。排除标准:风湿性关节炎的患者、化脓性关节炎、痛风等其他膝关节疾病患者;既往有半月板修补、韧带重建等膝关节手术史的患者;有MRI检查禁忌证或不能耐受长时间进行MRI检查者;图像伪影严重,影响评估者。162例患者中,男66例,女96例,年龄45~73(54.20±11.03)岁;BMI 18.92~27.03(20.63±3.92)kg/m2。根据是否符合膝关节退行性病变,将患者分为观察组(n=93)与对照组(n=69)。2组患者性别、年龄、BMI指数差异均无统计学意义(Pgt;0.05,表1)。本研究已获我院伦理委员会审核通过(伦理编号:P2023006)。
1.2 "方法
1.2.1 "MRI扫描 " 患者检查前均先休息30 min,采用GE 3.0T SIGNA "Pioneer磁共振扫描仪进行检查。患者仰卧,足先进,受检膝盖置膝关节线圈中,并使关节微屈约30°。固定膝关节使扫描中心位于髌骨下缘中点,参照文献[7] 方法分别行矢状位、轴状位及冠状位扫描T2WI脂肪抑制,矢状位T1WI、T1-mapping、T2-mapping及T2*-mapping序列扫描。获得T1-mapping、T2-mapping及T2*-mapping伪彩图与解剖图。DIXON法:参照文献[8] 以3D容积内插屏气检查序列对膝关节进行扫描,获得同相位图、反相位图、水相图及脂像图。
1.2.2 "图像处理 " 在工作站中处理mapping伪彩图,由2位具高级职称影像科医生参照文献方法对内侧髁、外侧髁T1、T2、T2*值及髌骨脂肪含量(FF)值进行测量[7-8]。将受检膝关节股骨内、外侧髁承重面三等分,放大后每部分软骨层面避开积液及骨质,取2 mm2 感兴趣区测量T2值后于相同位置取相同大小感兴趣区测量T2*和T1值,将3处平均值作为股骨内、外侧髁T1、T2、T2* 值。通过信号强度(SI)计算FF(%)=[SIfat/(SIfat+SIwater)]×100%。
1.2.3 "关节镜检查 " 在MRI扫描后1周内以Smithamp;nephew 560P HD成像系统行膝关节镜检查,根据镜检结果为金标准进行膝关节退行性病变诊断。比较病例组与对照组各MRI指标,并以ROC曲线分析各指标单独检测与联合检测对膝关节退行性病变的诊断价值。
1.3 "统计学分析
采用SPSS21.4软件分析数据,计数资料以n(%)表示,组间比较行卡方检验;计量资料以均数±标准差表示,组间比较行t检验;以ROC法分析各指标单独检测与联合检测对膝关节退行性病变的诊断效能。以Plt;0.05为差异有统计学意义。
2 "结果
2.1 "膝关节退行性病变患者影像学特征分析
本研究中MRI常规扫描对关节软骨变性检出率仅为66.67%,半月板退变检出率为61.53%。关节边缘骨质增生、关节腔隙狭窄、关节积液检出率较高,分别为89.47%、92.86%、93.33%(表2)。
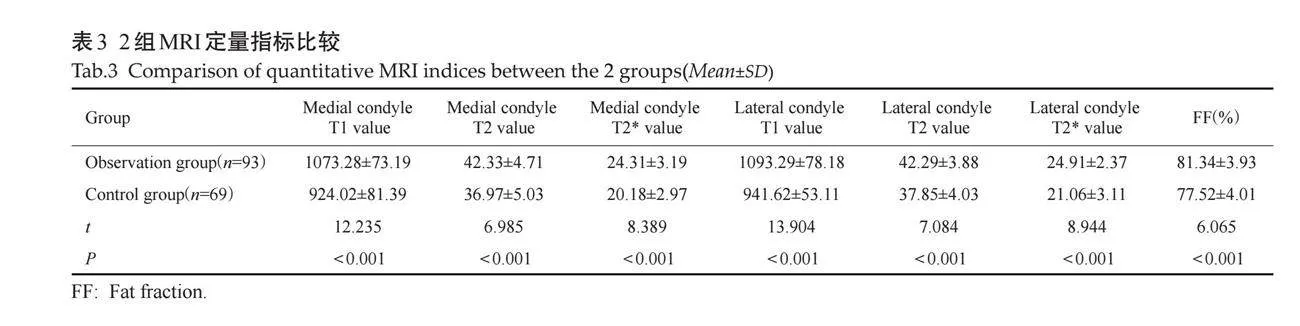
2.2 "2组MRI定量指标比较
观察组患者内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF(%)均高于对照组,差异有统计学意义(Plt;0.001,表3)。
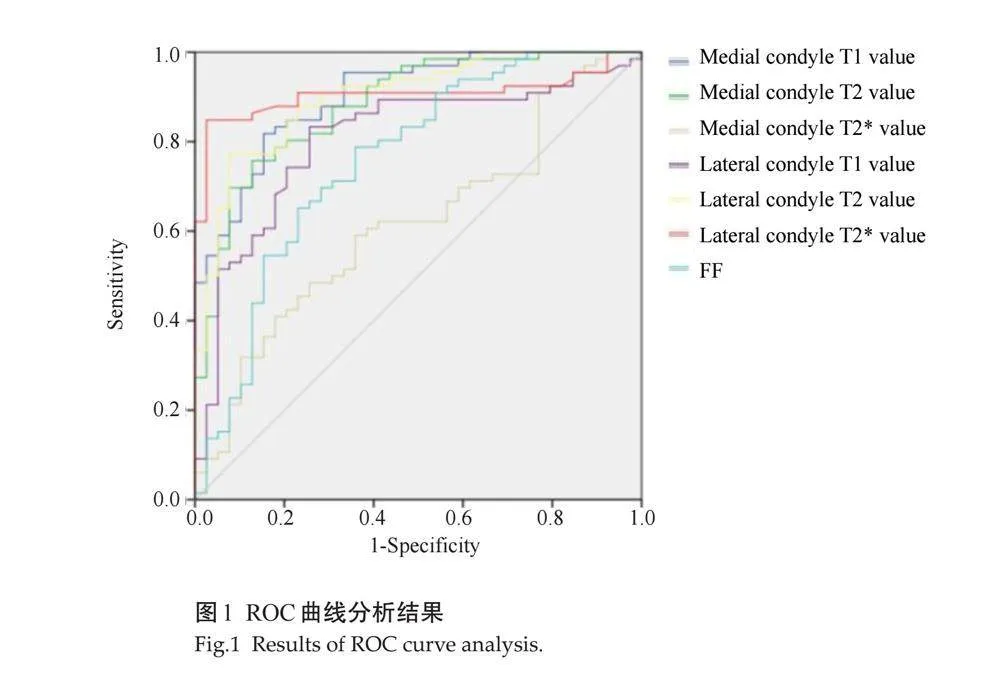
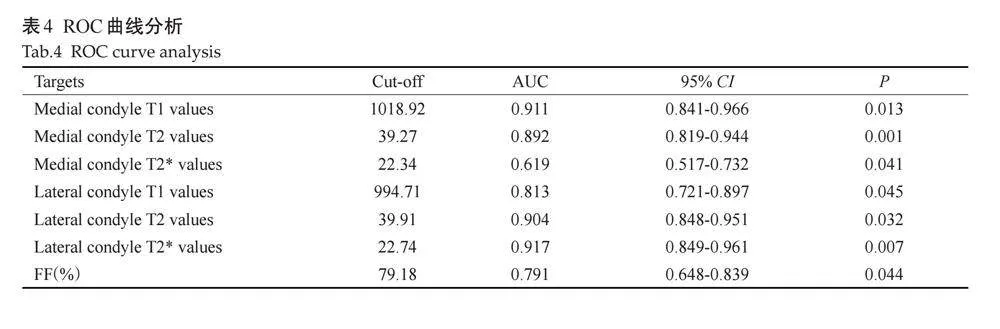
2.3 "ROC曲线分析
ROC曲线分析结果显示,内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF对膝关节退行性该病诊断截断值分别为1018.92、39.27、22.34、994.71、39.91、22.74及79.18%,AUC分别为0.911、0.892、0.619、0.813、0.904、0.917、0.791,均有统计学意义(Plt;0.05,图1、表4)。
3 "讨论
膝关节退行性病变为临床常见病,该病发生机制复杂,目前尚未被完全阐释,普遍认为其发生与坐姿习惯、膝关节劳损、局部炎症刺激、环境等因素有关[9-10] 。该病早期症状缺乏特异性,难以引起足够的重视,若得不到及时有效的治疗可致病情持续进展而影响疗效。MRI为膝关节退行性病变常用诊断方法,本研究结果显示,常规的MRI扫描对关节边缘骨质增生、关节腔隙狭窄、关节积液等较严重的膝关节退行性病变检出率较高,而对于关节软骨变性、半月板退变等早期病变诊断难度较大。考虑主要与常规MRI扫描对于关节软骨变性、半月板退变等早期病变的诊断根据关节面光整程度、“虫蚀状”改变等影像学特征进行分析,在早期病变时上述特征难以被发现,因此结合客观性更强、敏感度更高的量化指标有助于提高诊断效能,提高早诊率[11-12] 。
MRI软骨生理学定量技术与化学位移成像技术均为近年发展的新技术,软骨生理学定量分析主要通过分析组织固有弛豫值改变而实现对关节软骨内部变化的分析。有研究将其用于分析膝关节软骨变化情况,但少有学者将该技术用于膝关节退行性病变的诊断;化学位移成像则是通过对测定的组织信号计算脂肪分数而反映机体脂肪含量的改变,因骨质疏松的发生与骨髓腔内脂肪含量增多有关,近年也有研究将该指标用于反应骨质疏松情况,但将其用于膝关节退行性病变诊断者较少[13-17] 。本研究结果显示:观察组患者内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF(%)均高于对照组,且ROC分析结果显示上述指标用于膝关节退行性病变具有较高的诊断效能。膝关节软骨主要由软骨细胞及细胞外基质组成,细胞外基质包括水、胶原蛋白多糖及胶原糖胺聚合糖[18-19] 。在T2-mapping序列中软骨含水量、胶原纤维含量及排列方向的改变均可引起检测值的改变;T1值除受胶原含量变化影响外,蛋白多糖含量的改变也可引起该指标的异常改变[20-21] 。T2*-mapping序列与T2-mapping序列相比,其使用的是磁梯度而非180°聚相射频脉冲,因而对于磁场的不均匀性更为敏感,加上T2*-mapping序列的TE更短,因而其对软骨胶原蛋白结构改变更为敏感[22-23] 。因此,上述3种序列可由不同成分的改变反应膝关节软骨的变化,对于膝关节退行性病变的诊断效能更高。膝关节退行性病变的早期表现除关节软骨退化外,大量患者还伴有骨质量改变[24-25] 。骨骼主要由钙等无机物质与骨皮质、骨小梁等有机物组成,钙等无机物变化对于骨质量的影响已进行了大量的研究,有机物对骨质量的影响近年逐渐被关注,骨髓腔内的脂肪细胞与成骨细胞均由充质干细胞分化而来,骨髓内脂肪细胞增多将引起成骨细胞活动受抑制而影响骨生成,因而骨髓腔内脂肪水平更高膝关节退行性病变风险越大[26-27] 。本研究发现观察组患者FF水平更高,FF值是根据脂肪质子与水质子共振频率不同,在重复时间内设定2个或以上的特定回波时间所获得同相位及反相位图计算后所得到的脂肪分数,其水平升高提示骨髓腔内脂肪水平更高,成骨细胞抑制更明显。通过上述指标的检测可由不同方面反映膝关节软骨改变及骨质量变化情况,有助于提高膝关节软骨退行性病变的诊断效能[28] 。
综上所述,MRI常规扫描对关节软骨变性、半月板退变检出率较低,内侧髁T1值、内侧髁T2值、内侧髁T2*值、外侧髁T1值、外侧髁T2值、外侧髁T2*值及FF(%)值可用于膝关节退行性病变的诊断。因本研究为单中心研究,样本量有限,取得的结果可能存在一定的偏倚,后续也将采取多中心、大样本的研究,并进行长期跟踪随访及与其他诊断方法进行比较,以进一步凸显MRI定量指标对膝关节退行性病变的早期诊断价值。
参考文献:
[1] "Khurshedovna AS, Khazratkulovich RZ, Servetovna AA, et al. Radiation visualization of chronic joint diseases[J]. Cent Asian J Med Nat Sci, 2021, 2(2): 12-17.
[2] "Shan S, Rehman A, Ehsan J. Diagnostic value of dynamic ultrasonography in detection of meniscal injury in correlation with MRI knee findings keeping it as reference standard[J]. Pakistan J Med Res, 2023, 62(2): 49-52.
[3] "Li L, Yang XF, Yang LF, et al. Biomechanical analysis of the effect of medial meniscus degenerative and traumatic lesions on the knee joint[J]. Am J Transl Res, 2019, 11(2): 542-56.
[4] "Lee LS, Chan PK, Fung WC, et al. Imaging of knee osteoarthritis: a review of current evidence and clinical guidelines[J]. Musculoskeletal Care, 2021, 19(3): 363-74.
[5] "朱 "莉, 邹文远, 敖 锋. 三种MRI生理学定量技术对早期膝关节软骨损伤的诊断价值[J]. 陕西医学杂志, 2021, 50(3): 293-6.
[6] "Bodden J, Ok AH, Joseph GB, et al. Joint-adjacent adipose tissue by MRI is associated with prevalence and progression of knee degenerative changes: data from the osteoarthritis initiative[J]. J Magn Reson Imaging, 2021, 54(1): 155-65.
[7] "Sieroń D, Jabłońska I, Lukoszek D, et al. Knee diameter and cross-section area measurements in MRI as new promising methods of chondromalacia diagnosis-pilot study[J]. Medicina, 2022, 58(9): 1142.
[8] "Berton A, Longo UG, Candela V, et al. Quantitative evaluation of meniscal healing process of degenerative Meniscus lesions treated with hyaluronic acid: a clinical and MRI study[J]. J Clin Med, 2020, 9(7): 2280.
[9] "Nebelung S, Dötsch L, Shah D, et al. Functional MRI mapping of human Meniscus functionality and its relation to degeneration[J]. Sci Rep, 2020, 10(1): 2499.
[10] Huang GS, Peng YJ, Hwang DW, et al. Assessment of the efficacy of intra‑articular platelet rich plasma treatment in an ACLT experimental model by dynamic contrast enhancement MRI of knee subchondral bone marrow and MRI T2 "measurement of articular cartilage[J]. Osteoarthritis Cartilage, 2021, 29(5): 718-27.
[11] 李建安, 何 "卫, 汪青山, 等. MRI检查与X线平片对膝关节退行性骨关节病变中的诊断价值对比[J]. 吉林医学, 2019, 40(4): 739-41.
[12]Gao KT, Pedoia V, Young KA, et al. Multiparametric MRI characterization of knee articular cartilage and subchondral bone shape in collegiate basketball players[J]. J Orthop Res, 2021, 39(7): 1512-22.
[13] Linka K, Thüring J, Rieppo L, et al. Machine learning-augmented and microspectroscopy-informed multiparametric MRI for the non-invasive prediction of articular cartilage composition[J]. Osteoarthr Cartil, 2021, 29(4): 592-602.
[14] 王珊珊, 陈祖钦, 贺思健, 等. 磁共振化学位移成像联合体质指数评估青年骨量减少的价值[J]. 武警医学, 2020, 31(3): 233-6.
[15] Mohammed HT, Yoon S, Hupel T, et al. Unnecessary ordering of magnetic resonance imaging of the knee: a retrospective chart review of referrals to orthopedic surgeons[J]. PLoS One, 2020, 15(11): e0241645.
[16] Zhao Y, Zhu ZH, Chang J, et al. Predictive value of the morphology of proximal tibiofibular joint for total knee replacement in patients with knee osteoarthritis[J]. J Orthop Res, 2021, 39(6): 1289-96.
[17] Ciliberti FK, Guerrini L, Gunnarsson AE, et al. CT- and MRI-based 3D reconstruction of knee joint to assess cartilage and bone[J]. Diagnostics, 2022, 12(2): 279.
[18]Farag Abd El-Ati Mohamed AK, Farok Aggag M, Mohammed Zayed E, et al. Mri versus ultrasound in diagnosis of meniscal injury in the knee joint[J]. Al Azhar Med J, 2023, 52(2): 649-60.
[19] Kapustina I, Morcos G, Wieland M, et al. Worrisome and incidental signs on knee radiographs in clinical practice: traumatic and degenerative lesions[J]. Appl Radiol, 2023: 8-16.
[20]Ozeki N, Koga H, Sekiya I. Degenerative Meniscus in knee osteoarthritis: from pathology to treatment[J]. Life, 2022, 12(4): 603.
[21] Ramezanpour S, Kanthawang T, Lynch J, et al. Impact of sustained synovitis on knee joint structural degeneration: 4-year MRI data from the osteoarthritis initiative[J]. J Magn Reson Imaging, 2023, 57(1): 153-64.
[22]Uritani D, Koda H, Yasuura Y, et al. Factors associated with subjective knee joint stiffness in people with knee osteoarthritis: a systematic review[J]. Int J Rheum Dis, 2023, 26(3): 425-36.
[23] Małecki K, Niedzielski K, Korczyc-Stępnicka A, et al. A clinical, radiological and isokinetic evaluation in patients with recurrent patellar dislocation undergoing MPFL reconstruction according to Avikainen: a prospective study evaluating early degenerative changes after a minimum 10‑year follow‑up period[J]. BMC Musculoskelet Disord, 2023, 24(1): 147.
[24]Wang B, Wang L, Wang YY, et al. Clinical diagnostic value of magnetic resonance imaging in knee joint sports injury[J]. J Med Imaging Health Inform, 2021, 11(2): 453-61.
[25]Hung TNK, Vy VPT, Tri NM, et al. Automatic detection of Meniscus tears using backbone convolutional neural networks on knee MRI[J]. J Magn Reson Imaging, 2023, 57(3): 740-9.
[26] Rana S, Hossen M, Islamn A, et al. Interpretation of the common MRI findings in patients with painful knee joint[J]. Eur J Med Health Sci, 2021, 3(1): 19-26.
[27] Elshimy A, Osman AM, Awad MES, et al. Diagnostic accuracy of point-of-care knee ultrasound for evaluation of meniscus and collateral ligaments pathology in comparison with MRI[J]. Acta Radiol, 2023, 64(7): 2283-92.
[28]Ivanov S, Trizlov D. Painful anterior knee schwannoma: a case report[J]. JIMAB, 2023, 29(2): 4990-3.
(编辑:熊一凡)
