老年血管性痴呆患者血清微小RNA-206和微小RNA-186表达与病情严重程度及预后的相关性
2024-01-01邓勇陈忠军祁恒旭孙小鹏李迪







摘要:目的" 探究老年血管性痴呆(VD)患者血清微小RNA(miR)-206和miR-186表达与病情严重程度及预后的相关性。方法" 选取2020年10月至2023年5月在大连市中心医院接受治疗的104例老年VD患者为VD组,104例同期体检健康的志愿者为对照组。收集VD组和对照组基线资料;荧光定量PCR法检测血清miR-206、miR-186表达;根据VD严重程度分为:轻度VD组、中度VD组、重度VD组;老年VD患者出院后随访6个月,根据预后情况分为:良好及中等预后组和不良预后组。比较对照组和VD组基线资料及血清miR-206、miR-186水平,不同严重程度老年VD患者血清miR-206、miR-186水平,良好及中等预后组和不良预后组基线资料及血清miR-206、miR-186水平;分析老年VD患者血清miR-206、miR-186水平与简易精神状态量表(MMSE)评分的相关性,影响老年VD患者发生不良预后的因素,血清miR-206、miR-186对老年VD患者发生不良预后的预测价值。结果" VD组糖尿病史(P=0.021)、高血压史(P<0.001)、高脂血症史比例(P<0.001),血清miR-206(P<0.001)、miR-186(P<0.001)水平均显著高于对照组,日常生活能力量表评分显著低于对照组(P<0.001);轻度、中度、重度VD组血清miR-206、miR-186水平两两比较差异均有统计学意义(P均<0.001),趋势检验结果显示,血清miR-206、miR-186水平在轻度、中度、重度VD组中呈显著上升趋势(P均<0.001);老年VD患者血清miR-206、miR-186均与MMSE评分呈负相关(P均<0.001);不良预后组MMSE评分显著低于良好及中等预后组,血清miR-206、miR-186水平显著高于良好及中等预后组(P均<0.001);MMSE评分是影响老年VD患者发生不良预后的保护因素(P=0.005),miR-206、miR-186是影响老年VD患者发生不良预后的危险因素(P=0.001,P=0.007);血清miR-206和miR-186二者联合预测老年VD患者发生不良预后的曲线下面积为0.963,显著高于血清miR-206、miR-186各自单独预测的曲线下面积(0.866、0.878)(P=0.010,P=0.020)。结论" 老年VD患者血清miR-206、miR-186均呈高表达,二者与VD严重程度及预后密切相关,二者联合对评估老年VD患者的预后有较高效能。
关键词:老年血管性痴呆;微小RNA-206;微小RNA-186;严重程度;预后
中图分类号: R749.13" 文献标识码: A" 文章编号:1000-503X(2024)06-0883-07
DOI:10.3881/j.issn.1000-503X.16043
基金项目:辽宁省科学技术计划项目(2022-NLTS-11-02)
Correlations of Expression Levels of microRNA-206 and microRNA-186 in the Serum With Disease Severity and Prognosis of Elderly Patients With Vascular Dementia
DENG Yong,CHEN Zhongjun,QI Hengxu,SUN Xiaopeng,LI Di
Department of Neurological Intervention and Neurological Intensive Care,Dalian Municipal Central Hospital,Dalian,Liaoning 116033,China
Corresponding author:LI Di" Tel:0411-84412001,E-mail:jzlidi@126.com
ABSTRACT:Objective" To investigate the correlations of the expression levels of microRNA (miR)-206 and miR-186 in the serum with the disease severity and prognosis of elderly patients with vascular dementia (VD).Methods" A total of 104 elderly patients with VD treated in Dalian Municipal Central Hospital from October 2020 to May 2023 were selected into the VD group and 104 healthy volunteers who underwent physical examinations were enrolled in the control group.Baseline data of both groups were collected,and fluorescence quantitative PCR was used to measure the expression levels of miR-206 and miR-186 in the serum.According to the severity of VD,the patients were assigned into mild,moderate,and severe VD groups.The elderly patients with VD were followed up for 6 months after discharge.According to the prognosis,the patients were assigned into good/moderate and poor prognosis groups.The baseline data and the serum levels of miR-206 and miR-186 were compared between the control and VD groups as well as between the good/moderate and poor prognosis groups.The serum levels of miR-206 and miR-186 were compared between the mild,moderate,and severe VD groups.The correlations of serum miR-206 and miR-186 levels with mini-mental state examination (MMSE) score in elderly patients with VD were analyzed,on the basis of which the factors affecting the poor prognosis of elderly patients with VD were predicated.Furthermore,the predictive values of serum levels of miR-206 and miR-186 on the poor prognosis of elderly patients with VD were evaluated.Results" The VD group had higher proportions of diabetes history (P=0.021),hypertension history (Plt;0.001),and hyperlipidemia history (Plt;0.001),higher serum levels of miR-206 (Plt;0.001) and miR-186 (Plt;0.001),and lower score of activity of daily living (Plt;0.001) than the control group.The serum miR-206 and miR-186 levels varied between the mild,moderate,and severe VD groups (all Plt;0.001).The trend test results showed that serum miR-206 and miR-186 levels presented a rising trend in mild,moderate,and severe VD groups (all Plt;0.001).The serum miR-206 and miR-186 levels in elderly VD patients were negatively correlated with the MMSE score (all Plt;0.001).The poor prognosis group had lower MMSE score and higher serum levels of miR-206 and miR-186 than the good/moderate prognosis group (all Plt;0.001).The MMSE score was a protective factor and miR-206 and miR-186 were risk factors for poor prognosis in elderly patients with VD (P=0.005,P=0.001,P=0.007).The area under curve of combined serum miR-206 and miR-186 levels in predicting poor prognosis in the elderly patients with VD was 0.963,which was higher than those (0.866 and 0.878) of serum miR-206 and miR-186 levels separately (P=0.010,P=0.020).Conclusions" The serum levels of miR-206 and miR-186 in elderly patients of VD are high and closely related to the severity and prognosis of VD.The combination of the two demonstrates high performance in predicting the prognosis of elderly patients with VD.
Key words:vascular dementia of the elderly;microRNA-206;microRNA-186;severity;prognosis
Acta Acad Med Sin,2024,46(6):883-889
血管性痴呆(vascular dementia,VD)是一组由脑部血管病变引起的智力和认知功能障碍综合征,属于常见的痴呆性疾病[1]。引起VD发病的因素较多,有高血压史者比健康者更易患VD[2-3]。有报道微小RNA(microRNA,miR)-206可调节脑源性神经营养因子(brain derived neurotrophic factor,BDNF)的表达,抑制miR-206可使BDNF的水平升高从而促进脑缺血大鼠认知功能恢复[4]。有研究指出,有氧运动使miR-186表达降低,从而上调BDNF活性,影响海马神经元凋亡,抑制血管性认知障碍的病理发展,最终改善认知功能[5]。BDNF通过介导突触可塑性的多种功能,在改善认知功能、神经发生以及神经元分化等方面发挥作用[6]。可见miR-206、miR-186均参与大脑损伤过程,在改善认知功能方面发挥重要作用。目前,miR-206、miR-186与VD的关系尚不清晰,因此,本研究拟分析老年VD患者血清miR-206、miR-186与病情严重程度及预后的关系,以期帮助改善VD患者预后。
1" 资料和方法
1.1" 资料来源
选取2020年10月至2023年5月在大连市中心医院接受治疗的104例老年VD患者为VD组,年龄60~85岁。纳入标准:(1)符合VD相关诊断标准[7];(2)年龄≥60岁,临床资料完整,病情稳定;(3)均是初次确诊的患者;(4)无颅脑相关手术史;(5)病程大于6个月;(6)小学及以上文化程度。排除标准:(1)其他非血管原因引起的认知功能障碍;(2)有严重精神障碍、抑郁及自杀倾向;(3)有药物及酒精依赖史;(4)伴有各脏器功能不全者;(5)伴有恶性肿瘤及免疫性疾病者;(6)合并血液系统、全身感染性疾病者。选取104例同期于本院体检健康的志愿者为对照组,年龄60~85岁,对照组神经功能及认知功能均正常[简易精神状态量表(mini mental state examination,MMSE)[8]和日常生活能力量表(activity of daily living,ADL)[9]评分均正常]。收集VD组和对照组基线资料,包括:性别、年龄、体重指数、受教育年限、糖尿病史、高血压史、高脂血症史、吸烟史、饮酒史及入院后即刻ADL评分。本研究通过大连市中心医院伦理委员会批准(伦理审查编号:2020LC伦理第49号),受试对象均签署知情同意书。
1.2" 荧光定量PCR法检测血清miR-206、miR-186表达
VD患者入院后第2天清晨、对照组体检当天采集5 mL空腹静脉血,离心分离血清。按照RNA提取试剂盒(批号AKAC009D,北京盒子生工科技公司)操作说明书提取血清总RNA,对提取的总RNA进行含量、纯度检测后将RNA逆转录成cDNA,采用荧光定量PCR仪(型号FQD-16A,大连知微生物科技公司)进行扩增。20 μL反应体系:10 μL的PCR试剂,上下游引物各0.5 μL,cDNA(50 ng/μL)2 μL,加ddH2O至20 μL。反应程序:96 ℃预处理135 s;96 ℃ 21 s,74 ℃ 24 s,69 ℃ 18 s,共35个循环。引物由大连知微生物科技公司合成,引物序列见表1。miR-206、miR-186(内参均是U6)的相对表达水平采用2-ΔΔCt法计算。
1.3" VD患者严重程度分组及预后评估
入院后即刻对老年VD患者进行MMSE[8]评估,总分为30分,根据VD严重程度将患者分为:轻度VD组(MMSE评分在21分及以上)(32例)、中度VD组(9分<MMSE评分<21分)(39例)、重度VD组(MMSE评分在9分及以下)(33例)。老年VD患者出院后随访6个月,进行ADL[9]评分(包括10个项目,总分为100分),将患者分为:良好预后(ADL评分≥61分)(29例)、中等预后(40分<ADL评分<61分)(41例)、不良预后(ADL评分≤40分)(34例)[10]。以此为标准将患者分为:良好及中等预后组(70例)和不良预后组(34例)。
1.4" 统计学处理
使用SPSS 25.0软件分析数据,计量资料经检验均符合正态分布,以均数±标准差表示,t检验用于两组间比较,单因素方差分析及趋势检验用于3组间比较,进一步两两比较行LSD-t检验;以例数(%)表示计数资料,行χ2检验;用广义线性Logistic回归模型分析miR-206、miR-186与MMSE评分的相关性;采用多因素Logistic回归模型分析影响老年VD患者发生不良预后的因素;受试者工作特征(receiver operating characteristic,ROC)曲线对miR-206、miR-186评估老年VD患者发生不良预后的最佳诊断阈值进行选择,得出最佳截断值,Delong检验用于曲线下面积(area under curve,AUC)比较。P<0.05为差异有统计学意义。
2" 结果
2.1" 对照组和VD组基线资料比较
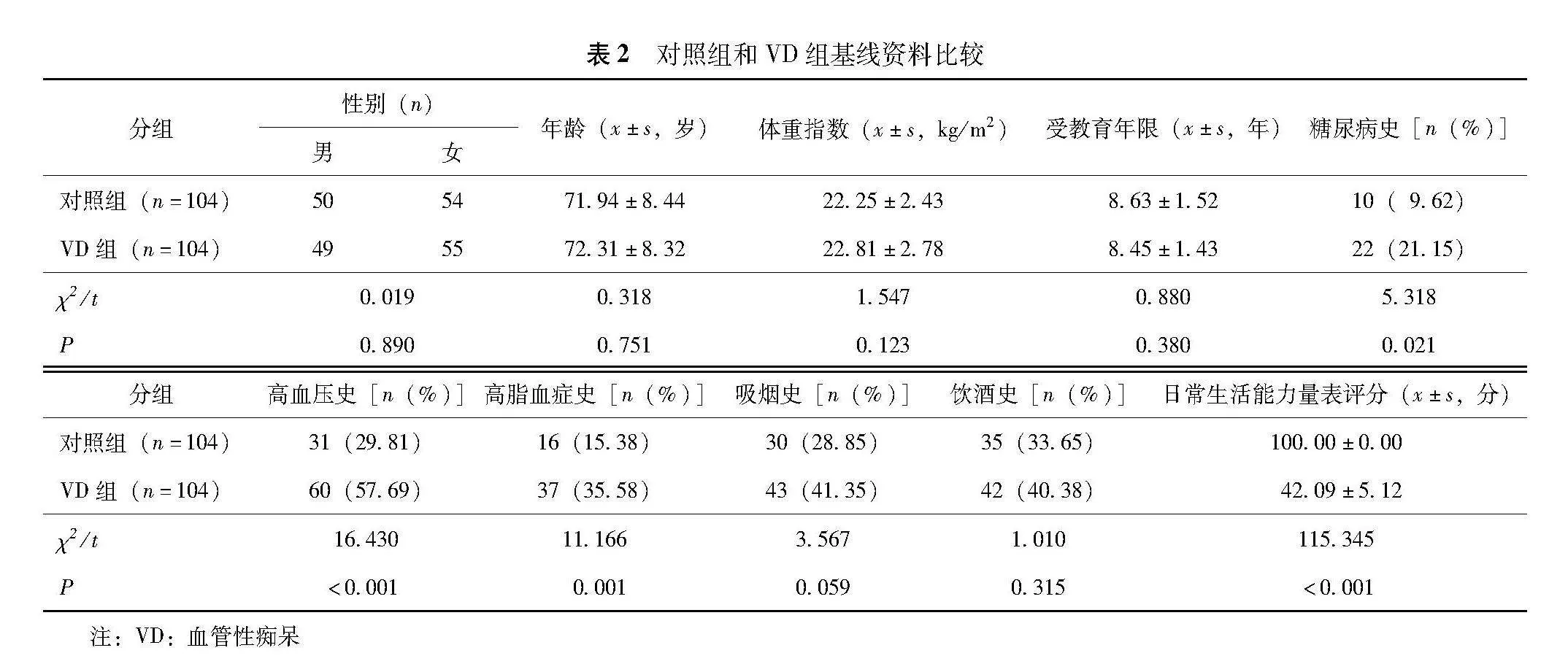
对照组性别、年龄、体重指数、受教育年限、吸烟史、饮酒史与VD组比较差异均无统计学意义(P均>0.05);VD组糖尿病史(P=0.021)、高血压史(P<0.001)、高脂血症史比例(P=0.001)均显著高于对照组,ADL评分显著低于对照组(P<0.001)(表2)。
2.2" 对照组和VD组血清miR-206、miR-186水平比较
VD组血清miR-206(2.41±0.32)、miR-186(3.27±0.61)水平均显著高于对照组(1.00±0.07、1.00±0.05)(t=43.897,t=37.823;P均<0.001)。
2.3" 血清miR-206、miR-186在不同严重程度患者中的比较
轻度、中度、重度VD组血清miR-206、miR-186水平两两比较差异均有统计学意义(P均<0.001),趋势检验结果显示,血清miR-206、miR-186水平在轻度、中度、重度VD组中呈显著上升趋势(P均<0.001)(表3)。
2.4" 血清miR-206、miR-186与MMSE评分的相关性
老年VD患者血清miR-206、miR-186与MMSE评分均呈显著负相关(β=-0.367,β=-0.027;P均<0.001)(表4)。
2.5" 良好及中等预后组和不良预后组基线资料比较
良好及中等预后组性别、年龄、体重指数、受教育年限、糖尿病史、高血压史、高脂血症史、吸烟史、饮酒史与不良预后组差异均无统计学意义(P均>0.05),不良预后组MMSE评分显著低于良好及中等预后组(P<0.001)(表5)。
2.6" 良好及中等预后组和不良预后组血清miR-206、miR-186水平比较
不良预后组血清miR-206(3.28±0.59)、miR-186(5.24±1.19)水平均显著高于良好及中等预后组(1.99±0.19、2.31±0.33)(t=16.670,t=19.220;P均<0.001)。
2.7" 老年VD患者发生不良预后的影响因素
以老年VD患者是否发生不良预后为因变量(不良预后=1,良好及中等预后=0),调整混杂因素后,进行多因素Logistic回归分析,结果显示MMSE评分是影响老年VD患者发生不良预后的保护因素(P=0.005),miR-206、miR-186是影响老年VD患者发生不良预后的危险因素(P=0.001,P=0.007)(表6)。
2.8" 血清miR-206、miR-186对老年VD患者发生不良预后的预测价值
绘制血清miR-206、miR-186及二者联合预测老年VD患者发生不良预后的ROC曲线,结果显示血清miR-206、miR-186及二者联合预测老年VD患者发生不良预后的AUC分别为0.866、0.878、0.963,miR-206、miR-186二者联合的AUC显著高于血清miR-206、miR-186各自单独预测的AUC(Z=2.559,P=0.010;Z=2.324,P=0.020)(表7、图1)。
3" 讨论
VD是指由血管性脑损伤引起的认知障碍或痴呆,是仅次于阿尔茨海默病的第二大常见痴呆形式。血管性脑损伤是指脑实质的损伤,最常见的原因是缺血、梗死和出血[11]。神经系统损伤与VD的发病关系密切,VD无法根治,只能改善及延缓病情进展[12-13]。评估VD患者病情严重程度并及时干预是改善患者预后的关键点。
miRNA通过与mRNA的3’非翻译区结合,在转录或翻译后调控基因表达[14]。miRNA可调控神经元凋亡及炎症反应参与神经元损伤过程,其表达水平与缺血性神经损伤导致的认知功能障碍有关[15]。有研究指出,慢性间歇乙醇和强迫游泳应激小鼠miR-206表达上调,可通过负性调控BDNF的表达导致神经损伤[16]。BDNF是生物体神经营养蛋白家族的重要成员,在促进神经元修复、神经元再生和改善轴突修复方面发挥重要作用[17-18]。Shao等[19]报道miR-206在阿尔茨海默病小鼠脑组织中高表达,抑制miR-206可促进BDNF高表达从而对阿尔茨海默病小鼠的神经元发挥保护作用。本研究显示,与健康者相比,miR-206在老年VD患者血清中升高,随着VD严重程度的加重,miR-206水平逐渐升高,提示miR-206参与VD发病和进展过程,其水平越高预示着VD病情越重。分析其可能原因为miR-206通过对下游靶基因BDNF的调控促进神经元损伤,参与VD发病和进展过程。
miR-186与神经功能密切相关,抑制miR-186-5p可上调神经系统发育所必需的胰岛素样生长因子-1的表达,减弱炎症因子和氧化应激,从而缓解创伤性脑损伤[20]。lncRNA锌指核转录因子反义链1通过靶向miR-186-5p/髓细胞白血病因子-1轴,在缺血性卒中细胞模型中发挥减轻氧气和葡萄糖剥夺介导损伤的作用[21]。抑制miR-186可直接靶向调控缺氧诱导因子1α,通过下调缺氧诱导因子1α减少神经元的缺血性损伤[22]。本研究显示,与健康者相比,miR-186在老年VD患者血清中升高,随着VD严重程度的加重miR-186逐渐升高,表明miR-186可能会影响VD发病,miR-186水平升高会导致VD病情加重。可能原因是miR-186可通过对下游靶基因的调控促进炎症反应及氧化应激,从而加重VD引起的神经元损伤。
临床上常用MMSE评分评估VD患者病情严重度和认知功能障碍程度。本研究显示,老年VD患者血清miR-206、miR-186均与MMSE评分呈负相关,提示老年VD患者血清miR-206、miR-186水平和认知功能有关,二者升高使VD患者脑损伤加重,导致认知功能减弱。预后分析显示,不良预后组血清miR-206、miR-186水平显著高于良好及中等预后组,且miR-206、miR-186是影响老年VD患者发生不良预后的危险因素,提示血清miR-206、miR-186升高的老年VD患者往往病情较重,对于此类患者需重点关注,以改善其预后。ROC曲线显示,血清miR-206和miR-186二者联合预测老年VD患者发生不良预后的AUC高于血清miR-206、miR-186各自单独预测的AUC,提示血清miR-206、miR-186有望成为预测老年VD患者预后的有效标志物,二者联合具有较高的预测效能。
综上,老年VD患者血清miR-206、miR-186均呈高表达,二者与VD严重程度及预后密切相关,二者联合对评估老年VD患者预后有较高效能。但本研究并未探究miR-206、miR-186影响VD发病的具体作用机制,这是临床研究的局限性所致,接下来将通过动物实验分析二者影响VD的具体机制,并探讨二者是否是VD的治疗靶点。
利益冲突" 所有作者声明无利益冲突
作者贡献声明" 邓勇:设计实验方案、论文撰写、修改;陈忠军、祁恒旭、孙小鹏:实施研究过程、病例收集和整理、数据统计;李迪:指导写作、审阅和修订论文
参" 考" 文" 献
[1]Yang X,Chen C,Wang A,et al.Imaging,genetic,and pathological features of vascular dementia[J].Eur Neurol,2023,86(4):277-284.DOI:10.1159/000531088.
[2]Liu C,Ma Y,Hofman A,et al.Educational attainment and dementia:mediation by mid-life vascular risk factors[J].Ann Neurol,2023,94(1):13-26.DOI:10.1002/ana.26647.
[3]Guan J,Li Q,Dai Z,et al.Quantitative morphometric changes in vascular mild cognitive impairment patients:early diagnosis of dementia[J].Cereb Cortex,2023,33(9):5501-5506.DOI:10.1093/cercor/bhac437.
[4]Shi G,Zeng P,Zhao Q,et al.The regulation of miR-206 on BDNF:a motor function restoration mechanism research on cerebral ischemia rats by meridian massage[J].Evid Based Complement Alternat Med,2022,2022:8172849.DOI:10.1155/2022/8172849.
[5]Niu Y,Wan C,Zhang J,et al.Aerobic exercise improves VCI through circRIMS2/miR-186/BDNF-mediated neuronal apoptosis[J].Mol Med,2021,27(1):4-15.DOI:10.1186/s10020-020-00258-z.
[6]Nikolac Perkovic M,Borovecki F,Filipcic I,et al.Relationship between brain-derived neurotrophic factor and cognitive decline in patients with mild cognitive impairment and dementia[J].Biomolecules,2023,13(3):570-583.DOI:10.3390/biom13030570.
[7]中国痴呆与认知障碍指南写作组,中国医师协会神经内科医师分会认知障碍疾病专业委员会.2018中国痴呆与认知障碍诊治指南(一):痴呆及其分类诊断标准[J].中华医学杂志,2018,98(13):965-970.DOI:10.3760/cma.j.issn.0376-2491.2018.13.003.
[8]黄妍,王洁,张军,等.老年血管性痴呆患者血清Lp-PLA2、S100β及尿液AD7C-NTP与认知功能的相关性[J].国际检验医学杂志,2021,42(10):1246-1249.DOI:10.3969/j.issn.1673-4130.2021.10.021.
[9]Ishimaru D,Tanaka H,Nagata Y,et al.Impact of disturbed rest-activity rhythms on activities of daily living in moderate and severe dementia patients[J].Alzheimer Dis Assoc Disord,2021,35(2):135-140.DOI:10.1097/WAD.0000000000000423.
[10]钟文清,陈晓瑜,刘丹丹.血管性痴呆患者血清神经调节蛋白1、神经元正五聚蛋白2的表达及临床意义[J].临床神经病学杂志,2023,36(1):28-33.DOI:10.3969/j.issn.1004-1648.2023.01.007.
[11]Chang Wong E,Chang Chui H.Vascular cognitive impairment and dementia[J].Continuum (Minneap Minn),2022,28(3):750-780.DOI:10.1212/CON.0000000000001124.
[12]Yu W,Li Y,Hu J,et al.A study on the pathogenesis of vascular cognitive impairment and dementia:the chronic cerebral hypoperfusion hypothesis[J].J Clin Med,2022,11(16):4742-4763.DOI:10.3390/jcm11164742.
[13]Linh TTD,Hsieh YC,Huang LK,et al.Clinical trials of new drugs for vascular cognitive impairment and vascular dementia[J].Int J Mol Sci,2022,23(19):11067-11083.DOI:10.3390/ijms231911067.
[14]Fu P,Zhao Y,Dong C,et al.An integrative analysis of miRNA and mRNA expression in the brains of Alzheimer’s disease transgenic mice after real-world PM2.5 exposure[J].J Environ Sci (China),2022,122(1):25-40.DOI:10.1016/j.jes.2021.10.007.
[15]Reinhold AK,Krug SM,Salvador E,et al.MicroRNA-21-5p functions via RECK/MMP9 as a proalgesic regulator of the blood nerve barrier in nerve injury[J].Ann N Y Acad Sci,2022,1515(1):184-195.DOI:10.1111/nyas.14816.
[16]Solomon MG,Griffin WC,Lopez MF,et al.Brain regional and temporal changes in BDNF mRNA and microRNA-206 expression in mice exposed to repeated cycles of chronic intermittent ethanol and forced swim stress[J].Neuroscience,2019,406(1):617-625.DOI:10.1016/j.neuroscience.2019.02.012.
[17]Xi B,Fu J,Wan D,et al.Ginsenoside Rg1 attenuation of neurogenesis disorder and neuronal apoptosis in the rat hippocampus after spinal cord injury may involve brain-derived neurotrophic factor/extracellular signal-regulated kinase signaling[J].Neuroreport,2023,34(5):290-298.DOI:10.1097/WNR.0000000000001891.
[18]Sharma V,Singh TG,Kaur A,et al.Brain-derived neurotrophic factor:a novel dynamically regulated therapeutic modulator in neurological disorders[J].Neurochem Res,2023,48(2):317-339.DOI:10.1007/s11064-022-03755-1.
[19]Shao Y,Xu T.A study on the neuroprotective effect of miR-206-3p on Alzheimer’s disease mice by regulating brain-derived neurotrophic factor[J].Ann Transl Med,2022,10(2):85-93.DOI:10.21037/atm-21-6601.
[20]Nie Y,Wang F.Inhibiting miR-186-5p relieves traumatic brain injury by regulating insulin-like growth factor-I-NLRP3/ASC/caspase-1 signaling pathway[J].Neuroreport,2023,34(3):156-164.DOI:10.1097/WNR.0000000000001873.
[21]Shen B,Wang L,Xu Y,et al.Long non-coding RNA ZFAS1 exerts a protective role to alleviate oxygen and glucose deprivation-mediated injury in ischemic stroke cell model through targeting miR-186-5p/MCL1 axis[J].Cytotechnology,2021,73(4):605-617.DOI:10.1007/s10616-021-00481-4.
[22]Li S,Wang Y,Wang M,et al.MicroRNA-186 alleviates oxygen-glucose deprivation/reoxygenation-induced injury by directly targeting hypoxia-inducible factor-1α[J].J Biochem Mol Toxicol,2021,35(6):1-11.DOI:10.1002/jbt.22752.
(收稿日期:2024-02-18)
