妊娠晚期脐动脉收缩末期与舒张末期峰值比与子代早期生长发育的相关性
2023-07-10胡月娇陈文玲
胡月娇 陈文玲
【摘要】 目的:探討妊娠晚期脐动脉收缩末期与舒张末期峰值比(S/D值)变化与子代早期生长发育的相关性。方法:回顾性分析2021年1-8月在中国解放军联勤保障部队第九〇八医院进行系统产检并能完整随访的83例产妇为研究对象,根据子代是否出现早期生长发育异常分组,将出现早期生长发育异常者纳入研究组,将早期生长发育正常者纳入对照组,回顾性分析比较两组一般临床资料,并探讨妊娠晚期脐动脉S/D值变化与子代早期生长发育的相关性。结果:研究组空腹血糖(FPG)水平高于对照组,新生儿出生后1 min Apgar评分低于对照组,差异均有统计学意义(P<0.05);两组孕晚期搏动指数(PI)、阻力指数(RI)、S/D值均明显低于孕中期,但研究组孕晚期PI值、RI值、S/D值均高于对照组,差异均有统计学意义(P<0.05)。logistic回归分析显示,孕晚期PI、RI、S/D值、FPG水平是子代早期生长发育的危险因素(P<0.05),新生儿出生后1 min Apgar评分是子代早期生长发育的保护因素(P<0.05)。结论:孕晚期PI、RI、S/D值及FPG和新生儿出生后1 min Apgar评分均会对子代早期生长发育产生影响,且随着孕期增加,脐带PI值、RI值、S/D值均明显降低,临床可针对以上因素对妊娠晚期妇女进行干预,以降低子代早期生长发育异常的发生率。
【关键词】 妊娠晚期 脐动脉S/D值 子代 早期生长发育 相关性
[Abstract] Objective: To explore the correlation between end-systolic peak flow velocity to end-diastolic peak flow velocity (S/D) ratio of umbilical artery in late pregnancy and early growth and development of offspring. Method: This study retrospectively reviewed 83 puerperae who received systematic antenatal examination in the 908th Hospital of Joint Logistics Support Force of the Chinese PLA and completed follow-up from January to August 2021. According to the presence or absence of early growth and development abnormality of offspring, the subjects were divided into study group (early growth and development abnormality of offspring) and control group (normal early growth and development of offspring). The general clinical data of the two groups were compared. The correlation between the change of umbilical artery S/D value in late pregnancy and the early growth and development of the offspring was discussed. Result: Fasting plasma glucose (FPG) level in the study group was higher than that in the control group, and neonatal Apgar score at 1 min after birth was lower than that in the control group, with statistically significant differences (P<0.05). Pulsatility index (PI), resistance index (RI) and S/D values in the two groups in late pregnancy were significantly lower than those in mid pregnancy. Meanwhile, PI, RI and S/D value in the study group in late pregnancy were higher than those in the control group, with statistically significant differences (P<0.05). logistic regression analysis showed that PI, RI, S/D and FPG levels in the third trimester were risk factors for early growth of offspring (P<0.05), and Apgar score 1 min after birth was protective factor for early growth and development of offspring (P<0.05). Conclusion: PI, RI, S/D value and FPG in late pregnancy, and neonatal Apgar score at 1 min after birth affect the early growth and development of the offspring. With the prolongation of pregnancy, umbilical PI, RI and S/D are significantly decreased. The above indicators are significantly positively correlated with early growth and development abnormality of offspring, suggesting that clinical interventions can be conducted for the women in late pregnancy based on the above factors to reduce the incidence of early growth and development abnormality of offspring.
[Key words] Late pregnancy Umbilical artery S/D value Offspring Early growth and development Correlation
First-author's address: The 908th Hospital of Joint Logistics Support Force of the Chinese PLA, Nanchang 330000, China
doi:10.3969/j.issn.1674-4985.2023.13.034
任何宮内外不良因素都可能影响胎儿的生长发育,将会导致在基因、酶、细胞、组织、器官等层面发生“程序化”的改变,并由此产生一系列儿童期、成年期疾病[1]。现有技术还无法直接实时监测宫内环境,而胎儿脐动脉血流速度波形可反映胎儿胎盘血流动力学的变化,与胎盘循环密切相关,在监测胎盘血灌注状况方面具有不可替代的作用,且与胎儿早期循环系统和酸碱平衡紊乱有显著关系,可间接反应宫内环境[2]。脐动脉收缩末期与舒张末期峰值(S/D)比值检测具有无创伤、可重复性,且测定不受声束、血管面积及角度的影响,可作为监测宫内环境的有效可靠指标[3]。目前国内外关于早期宫内环境不良与子代早期生长发育的相关性研究尚不多,缺乏早期对高危儿童的监测、干预方法,本研究回顾性分析83例患者一般临床资料,探讨影响子代早期生长发育影响因素,并分析脐带血流指标与子代早期生长发育相关性,旨在为子代早期生长发育异常早期预警及干预提供有效依据,结果如下。
1 资料与方法
1.1 一般资料 回顾性分析2021年1-8月在中国解放军联勤保障部队第九〇八医院进行系统产检并能完整随访的83例产妇为研究对象,纳入标准:(1)自然受孕;(2)单胎;(3)孕龄明确;(4)入组孕周32~41周;(5)有完整产前检查资料;(6)孕妇能坚持随访。排除标准:(1)孕期感染性疾病、代谢性疾病、甲状腺疾病等;(2)遗传性疾病史;(3)随访期间出现影响代谢及正常生长发育的疾病或外伤。根据子代是否出现早期生长发育异常分组,将出现早期生长发育异常者42例纳入研究组,将早期生长发育正常者41例纳入对照组。本研究符合赫尔辛基宣言相关准则,经本院医学伦理委员会批准。
1.2 早期生长发育异常标准 于3、6、12月龄由监护人根据实际情况在专业人员的指导下完成年龄与发育进程问卷中文版(ages and stages questionnaires chinese version,ASQ-C),进行神经行为测试和体格发育测试,共包含个人-社会、解决问题、精细动作、大动作、沟通5个能区,各能区共6个项目,每个项目包括“是”“有时是”和“否”3个选项,评分标准分别10、5和0分,6个项目的总得分为该能区的最终得分。ASQ-C界值标准参照姚国英等[4]的研究结果,采用各年龄段各能区的P15为界值,得分≤P15界定为早期生长发育异常,得分>P15为早期生长发育正常。
1.3 方法 分析比较两组一般临床资料,包括产妇年龄、产妇孕周、搏动指数(PI)、阻力指数(RI)、S/D、新生儿出生后1 min Apgar评分、空腹血糖(FPG)、甘油三酯(TG)、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)。采用彩色多普勒超声(型号为GE Voluson E8)检测羊膜腔中游离脐带段搏动指数(PI)、阻力指数(RI)、收缩期最大血流速度与舒张末期血流速度比(S/D值)。
1.4 统计学处理 采用SPSS 20.0软件处理数据,无序分类资料以率(%)表示,采用字2检验,计量资料以(x±s)表示,行t检验,采用logistic回归分析影响子代早期生长发育的因素,P<0.05为差异有统计学意义。
2 结果
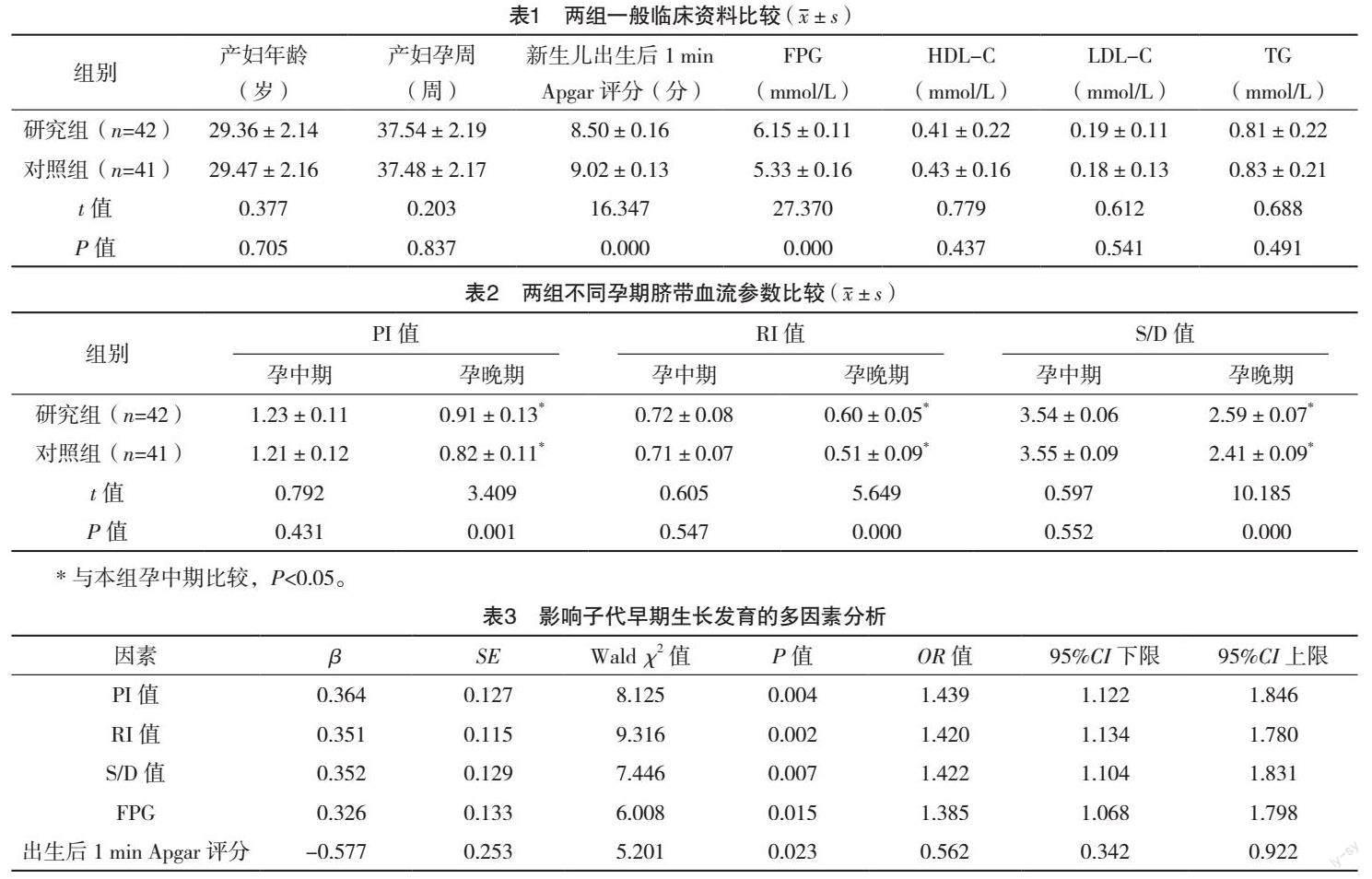
2.1 两组一般临床资料比较 研究组FPG水平高于对照组,新生儿出生后1 min Apgar评分低于对照组,差异均有统计学意义(P<0.05),两组产妇年龄、产妇孕周、HDL-C、LDL-C、TG比较,差异均无统计学意义(P>0.05),见表1。
2.2 两组不同孕期脐带血流参数比较 两组孕晚期PI值、RI值、S/D值均明显低于孕中期,但研究组孕晚期PI值、RI值、S/D值均高于对照组(P<0.05),两组孕中期PI值、RI值、S/D值比较差异均无统计学意义(P>0.05),见表2。
2.3 影响子代早期生长发育的多因素分析 以子代早期生长发育为因变量(正常=0,异常=1),以孕晚期PI、RI、S/D值及FPG和新生儿出生后1 min Apgar评分为自变量,logistic回归分析显示,孕晚期PI值、RI值、S/D值、FPG是子代早期生长发育的危险因素(P<0.05),新生儿出生后1 min Apgar评分是子代早期生长发育的保护因素(P<0.05),见表3。
3 讨论
脐带动脉血流变化既能反映胎盘灌注情况,也能反映孕期胎儿的血供情况[9-10]。在其他条件基本稳定的情况下,一方面脐动脉内的血流量、血流阻力大小直接受胎盘循环灌注情况影响,螺旋动脉重铸障碍或胎盘绒毛血管发育不良都将使脐动脉血流减少、流速下降;另一方面脐动脉内的血流量、血流阻力大小可直接影响到胎儿与母血的营养物质交换,从而进一步影响到胎儿在宫内的生长发育情况[11-12]。正常妊娠期间,随妊娠进展,脐动脉S/D值呈逐渐下降趋势,临床上妊娠晩期脐动脉S/D>3.0,或S/D值高于相应孕周第95个百分位数为异常,往往预示胎儿血供不足,处于缺氧状态[13]。目前国内外对脐动脉S/D的研究大多集中于对胎儿宫内窘迫、围产儿结局的预测,均肯定了脐动脉S/D是预测胎儿宫内窘迫早期、准确、高敏感的指标,可以降低围产儿出生的不良结局[14-15]。本研究发现,生长发育异常者与早期生长发育正常者产妇孕晚期PI值、RI值、S/D值均明显低于孕中期,但研究组孕晚期PI值、RI值、S/D值均高于对照组,正常晚期妊娠时,脐动脉的PI、RI、S/D值比较平稳,当胎盘血管发生病理性改变时脐血流阻力升高,脐动脉PI、RI、S/D值增高,胎儿与胎盘间的循环血流阻力增大,胎盘的有效交换面积减少,胎盘血液有效灌注不足,引起缺氧缺血,使母体与胎儿间营养物质供给减少,这时候往往胎儿处于缺氧代偿期,早于其他异常监测指标出现[16-18]。故妊娠晚期脐动脉PI、RI、S/D值升高,可间接反应早期宫内环境不良,临床应及时给予针对性治疗。
logistic回归分析显示,孕晚期PI、RI、S/D值、FPG水平是子代早期生长发育的危险因素,新生儿出生后1 min Apgar評分是子代早期生长发育的保护因素,宫内环境不良,胎儿生长受影响,可使胰岛β细胞减少复制,降低分化,导致β细胞数量减少,分泌胰岛素的能力下降,使得他们成年时对导致肥胖应激的抵抗能力降低,增加胰岛素抵抗及非胰岛素依赖性糖尿病发生。FPG则是反映机体糖尿病生成的有效指标,其水平的异常升高明显增加了妊娠期糖尿病风险,亦会影响子代早期发育[19-20]。正常妊娠中,胎盘滋养细胞的浸润能力大小会影响母胎血管网络发育程度,一旦母胎血管网络出现障碍,则会明显降低胎盘血流灌注量,影响宫内环境,宫内环境与出生后慢性疾病具有相关性,宫内窘迫及发育迟缓引起的胎儿的器官损伤或发育期间器官细胞绝对数的减少及代谢机制失调是引儿童发育期间并发代谢综合征的主要原因[21-22]。
综上所述,孕晚期PI、RI、S/D值、FPG水平是子代早期生长发育的危险因素,新生儿出生后1 min Apgar评分是子代早期生长发育的保护因素,可为临床治疗方案提供参考。
参考文献
[1] GU W,LIN J,HOU Y Y,et al.Effects of low-dose aspirin on the prevention of preeclampsia and pregnancy outcomes: a randomized controlled trial from Shanghai,China[J].Eur J Obstet Gynecol Reprod Biol,2020,248(7):156-163.
[2] TRAN D,COOKE S,ILLINGWORTH P J,et al.Deep learning as a predictive tool for fetal heart pregnancy following time-lapse incubation and blastocyst transfer[J].Hum Reprod,2019,34(6):1011-1018.
[3] KONWAR R,BASUMATARI B,DUTTA M,et al.Role of Doppler waveforms in pregnancy-induced hypertension and its correlation with perinatal outcome[J/OL].Cureus,2021,13(10):e18888.https://pubmed.ncbi.nlm.nih.gov/34820216/.
[4]姚国英,卞晓燕,JANE S,等.年龄与发育进程问卷中文版的婴幼儿发育筛查界值标准研究[J].中华儿科杂志,2010,48(11):824-828.
[5] KAUR K,ACHARYA G,CHEN H,et al.Impact of fetal trisomy 21 on umbilical artery Doppler indices[J].J Matern Fetal Neonatal Med,2021,27(12):1-8.
[6]程昇,沈晓燕.胎儿动脉指数与脐带绕颈压迹深度的相关性[J].中国妇幼健康研究,2019,30(10):1201-1204.
[7]李文杰,连帅,徐彬,等.产前母体应激对子代生长发育的影响[J].生理科学进展,2019,50(4):285-288.
[8] PAULES C,DANTAS A P,MIRANDA J,et al.Premature placental aging in term small-for-gestational- age and growth-restricted fetuses[J].Ultrasound Obstet Gynecol,2019,53(5):615-622.
[9] STOENESCU M,SERBANESCU M S,DIJMARESCU A L,et al.Doppler uterine artery ultrasound in the second trimester of pregnancy to predict adverse pregnancy outcomes[J].Curr Health Sci J,2021,47(1):101-106.
[10] YAKUT K,?CAL D F,?ZT?RK F,et al.Turkish reference ranges for the left fetal modified myocardial performance index[J].Turk J Pediatr,2021,63(6):1038-1047.
[11] LIU H,NIU H,ZENG W.Doppler ultrasound under image denoising algorithm in the diagnosis and treatment of fetal growth restriction using Aspirin combined with Low-Molecular-Weight Heparin[J].J Healthc Eng,2021,2021(Pt.10):9697962.
[12] I?IKALAN M M,YENI?ERI H,TOPRAK E,et al.Effect of previous cesarean sections on second-trimester uterine artery Doppler[J].J Obstet Gynaecol Res,2020,46(9):1766-1771.
[13]刘彦超,赵鑫,赵彩雯,等.子痫前期孕妇胎儿血流频谱与早產儿脑发育的相关性[J].中国医学影像技术,2020,36(5):720-725.
[14]邵晴荷,杨洁,周玉珊,等.妊娠期糖尿病患者血清Cys C、Hcy以及胎儿脐动脉血流动力学指标对胎儿妊娠结局的影响[J].广东医学,2019,40(20):2867-2871.
[15]龚儒杰,姚莉萍,朱向明,等.超声评估妊娠期高血压疾病孕妇左心功能改变及其与子宫动脉阻力指数的相关性[J].中国医学影像学杂志,2019,27(9):709-713.
[16]王立娟,勇强,包晶晶,等.胎儿脐带绕颈程度与胎儿左心室Tei指数及脐动脉S/D值相关性研究[J].中国超声医学杂志,2019,35(5):447-450.
[17] NNAMANI A O,IBEWUIKE C U,OKERE P C,et al.Comparative analysis of umbilical artery Doppler indices of normal and suspected IUGR fetuses in the third trimester[J].Niger J Clin Pract,2021,24(12):1793-1799.
[18] XU R,ZHU Z,TANG W,et al.Zone-specific reference ranges of fetal adrenal artery Doppler indices:a longitudinal study[J].BMC Pregnancy Childbirth,2020,20(1):774.
[19]彭燕霞,陈平.妊娠期糖尿病孕妇胎儿脐动脉血流S/D值随孕周变化情况及其与胎儿窘迫的相关性[J].中国妇幼保健,2019,34(10):2221-2224.
[20]王琴晓,林希,焦岩,等.彩色多普勒超声综合评估在胎儿生长受限诊断中的应用价值[J].浙江医学,2020,42(10):1014-1017,1021.
[21] STEFOPOULOU M,HERLING L,JOHNSON J,et al.Reference ranges of fetal superior vena cava blood flow velocities and pulsatility index in the second half of pregnancy: a longitudinal study[J].BMC Pregnancy Childbirth,2021,21(1):158.
[22]任秀娥,王卓,郑晓芳,等.高危妊娠晚期胎儿脐动脉、大脑中动脉血流多普勒参数变化与不良妊娠结局的关系[J].影像科学与光化学,2020,38(3):447-452.
(收稿日期:2022-11-15) (本文编辑:何玉勤)
