血清S-100β、NSE及TCD等指标在脓毒症相关性脑病患者中的变化及意义
2022-04-02王晶晶
王晶晶
【摘要】 目的:探讨血清S-100β、NSE及TCD等指标在脓毒症相关性脑病(SAE)患者中的变化及意义。方法:选择2019年1月-2021年1月佳木斯市中心医院收治的80例脓毒症患者,其中45例SAE患者为SAE组,35例无SAE的患者为对照组。统计分析两组一般临床资料;于患者入院第1天未治疗时和对症治疗后的第3天检测并记录血清S-100β、NSE水平,同时进行TCD检查,记录并比较两组舒张末期血流速度(Vd)、收缩期峰值血流速度(Vs)、平均血流速度(Vm),通过测得数值计算搏动指数(PI)及阻力指数(RI)。结果:SAE组APACHEⅡ评分、SOFA评分及休克比例均高于对照组(P<0.05)。SAE组入院第1、3天血清NSE、S-100β均明显高于对照组,两组入院第3天血清NSE、S-100β均低于第1天,差异均有统计学意义(P<0.05)。两组入院第1天及第3天的Vs比较,差异均无统计学意义(P>0.05);入院第1、3天,对照组的Vd、PI、RI均优于SAE组,差异均有统计学意义(P<0.05);对照组入院第1天的Vm高于SAE组,差异有统计学意义(P<0.05);两组入院第3天PI、RI均优于入院第1天(P<0.05)。结论:SAE患者病情较重,血清S-100β、NSE及Vd、Vm、PI、RI變化明显,动态监测上述指标变化有助于病情及治疗效果的判断。
【关键词】 脓毒症相关性脑病 S-100β 神经元特异性烯醇化酶 经颅多普勒超声
Changes and Significance of Serum S-100β, NSE and TCD in Patients with Sepsis Associated Encephalopathy/WANG Jingjing. //Medical Innovation of China, 2022, 19(05): 0-026
[Abstract] Objective: To investigate the changes and significance of serum S-100β, NSE and TCD in patients with sepsis associated encephalopathy (SAE). Method: A total of 80 sepsis patients admitted to Jiamusi Central Hospital from January 2019 to January 2021 were selected, including 45 patients with SAE as the SAE group and 35 patients without SAE as the control group. The general clinical data of the two groups were statistically analyzed; serum S-100β, NSE were detected and recorded on the first day of admission without treatment and the third day after symptomatic treatment. The end diastolic blood flow velocity (Vd), peak systolic blood flow velocity (Vs) and mean blood flow velocity (Vm) were recorded and compared between the two groups, the pulsatility index (PI) and resistance index (RI) were calculated by the measured values. Result: The APACHEⅡ score, SOFA score and shock rate of SAE group were higher than those of the control group (P<0.05). Serum NSE and S-100β in SAE group were significantly higher than those in control group on the 1st and 3rd day of admission, and serum NSE and S-100β in SAE group on the 3rd day of admission were lower than those in the 1st day of admission, the differences were statistically significant (P<0.05). There were no significant differences in Vs between the two groups on the 1st and 3rd day of admission (P>0.05); on the 1st and 3rd day of admission, Vd, PI and RI in the control group were better than those in the SAE group, the differences were statistically significant (P<0.05); the Vm of the control group on the 1st day of admission was higher than that of the SAE group, the difference was statistically significant (P<0.05); PI and RI on the 3rd day of admission in both groups were better than those on the 1st day (P<0.05). Conclusion: Patients with SAE are in severe condition, serum S-100β, NSE and Vd, Vm, PI, RI changed significantly in patients with SAE, dynamic monitoring the changes of these indexes is helpful to judge patients condition and therapeutic effect.
[Key words] Sepsis associated encephalopathy S-100β Neuron specific enolase Transcranial Doppler ultrasound
First-author’s address: Jiamusi Central Hospital, Heilongjiang Province, Jiamusi 154002, China
doi:10.3969/j.issn.1674-4985.2022.05.006
脓毒症相关性脑病(SAE)是脓毒症患者脑功能障碍的一种常见临床表现,症状从谵妄到昏迷不等,其发病率和死亡率较高,约为50%[1]。由于SAE对幸存者的长期神经认知功能影响很大,给患者造成较大经济负担并严重影响患者生活质量[2]。镇静和机械通气的脓毒性休克患者因无法沟通及配合检查,影响SAE的早期和准确的临床诊断,因此生物学标志物成為SAE监测与检查的重要工具[3-4]。血清S-100β蛋白、神经元特异性烯醇化酶(NSE)均为脑损伤的生物标志物,但其在SAE筛查和监测方面的价值仍存在争议[5-7]。经颅多普勒超声(TCD)由于其可移动性及床旁实时检测脑血管血流动力学的变化,可能为脓毒症患者的脑血流动力学变化提供有价值的信息[8-9]。本研究就血清S-100β、NSE及TCD在SAE患者中价值进行研究,现报道如下。
1 资料与方法
1.1 一般资料 选择2019年1月-2021年1月佳木斯市中心医院收治的80例脓毒症患者,其中45例SAE患者为SAE组,另外35例无SAE的患者为对照组。纳入标准:符合脓毒症诊断标准[10],SAE经神经系统查体、实验室检查、脑电图等做排除性诊断[11]。排除标准:(1)既往神经系统疾病患者,如脑卒中、感染等;(2)凝血功能障碍的患者;(3)恶性肿瘤患者。患者或家属同意并配合研究,该研究经本院伦理委员会批准。
1.2 方法 于患者入院第1天未治疗时和对症治疗后的第3天抽取空腹外周静脉血,送至检验科离心保存血清,电化学发光免疫分析法检测血清NSE含量,双抗体夹心法检测血清S-100β水平;同时,于患者入院第1、3天对患者进行TCD检查,探头直接经过颞骨窗检测两侧大脑中动脉,检测并记录舒张末期血流速度(Vd)、收缩期峰值血流速度(Vs)及平均血流速度(Vm),通过测得数值计算搏动指数(PI)及阻力指数(RI),PI=(Vs-Vd)/Vm,RI=(Vs-Vd)/Vs。
1.3 观察指标 记录比较两组一般临床资料,包括年龄、性别、创伤、急性生理与慢性健康状况评分系统(APACHEⅡ)、序贯器官衰竭评分(SOFA)、休克、动脉血二氧化碳分压(PaCO)、平均动脉压(MAP);记录比较两组入院第1、3天血清NSE、S-100β及TCD检查指标Vs、Vd、Vm、PI、RI。
1.4 统计学处理 采用SPSS 23.0对所得数据进行统计学处理与分析。计量资料中,符合正态分布者采用(x±s)表示,比较用t检验,不符合正态分布者以M(Q,Q)表示,比较则用Mann-Whitney U检验;计数资料用例(%)表示,比较采用χ检验。P<0.05为差异有统计学意义。
2 结果
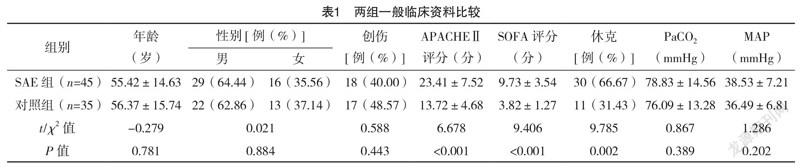
2.1 两组一般临床资料比较 两组年龄、性别、创伤率、PaCO、MAP比较,差异均无统计学意义(P>0.05);SAE组APACHEⅡ评分、SOFA评分及休克比例均高于对照组(P<0.05)。见表1。
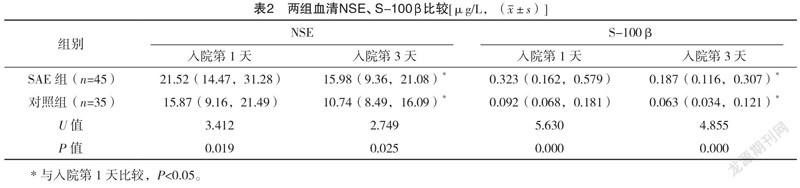
2.2 两组血清NSE、S-100β比较 SAE组入院第1、3天血清NSE、S-100β均明显高于对照组,两组入院第3天血清NSE、S-100β均低于第1天,差异均有统计学意义(P<0.05),见表2。
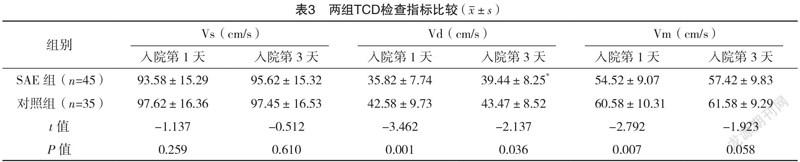
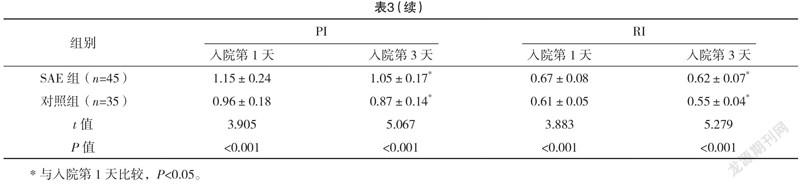
2.3 两组TCD检查指标比较 入院第1、3天,两组的Vs比较,差异均无统计学意义(P>0.05);入院第1、3天,对照组Vd、PI、RI均优于SAE组,差异均有统计学意义(P<0.05);入院第1天,对照组Vm高于SAE组,差异有统计学意义(P<0.05);两组入院第3天PI、RI均优于第1天(P<0.05)。见表3。
3 讨论
脓毒症及其并发症是ICU最常见的死亡原因之一,死亡率在10%~50%,如果患者出现意识障碍,则死亡率显著升高[12]。中枢神经系统(CNS)是脓毒症最早受累的器官之一,其临床表现即SAE,SAE的病理生理学复杂,可能涉及神经递质功能障碍、炎症、血管改变、小胶质细胞活化和血脑屏障功能障碍。SAE是ICU最常见的脑病类型,发病率约为50%[13],研究表明,APACHEⅡ、SOFA越高SAE发生可能性越大[14],与本研究中SAE组APACHEⅡ、SOFA评分均高于对照组的结果一致。SAE组由于其症状的多样性缺乏特异性,不易被发现,目前SAE诊断主要依据为结合症状、脑电图、生物标志物、体感诱发电位等进行排除性诊断[15]。
S-100β和NSE被认为是SAE发生的重要生物标志物[13]。S-100β是一种钙结合蛋白,主要由中枢神经系统中星形胶质细胞产生,其不易通过血脑屏障,脑损伤后血清和脑脊液中的含量增加可能由于这些细胞分泌活性增加及血脑屏障的破坏,提示该指标可作为脑缺血和脑损伤后不良神经认知结局的指标,是脑屏障破坏的标志[16]。NSE是胞浆内糖化酶,在神经元和神经内分泌组织中发现,当这些细胞死亡增加后,血循环中NSE即升高。Yao等[1]比较了SAE与非SAE患者血清S100β和NSE水平,发现SAE患者血清S100β和NSE水平均明显更高,与本研究结果一致。NSE和S-100β在脑损伤中的价值及诊断意义已得到较多研究证实,但对不同时间点其动态变化缺乏相应研究,本研究中两组入院第3天NSE和S-100β均较入院第1天下降,但SAE组仍高于对照组,提示NSE和S-100β与脑损伤有一定关系,且治疗后有一定程度下降,动态监测其血清水平变化有助于判断治疗效果及预后。
血管运动功能障碍常导致脑血流量失调,直接影响脑功能和脑血液循环,被认为是引起SAE的主要原因[17]。脑微循环受损(灌注微血管密度降低)和脑血流紊乱被认为是SAE的可能机制,而灌注微血管密度的降低可能与脑血管阻力的增加有关[18]。TCD是重要、无创且可床旁进行的脑血流动力学检测方法,当SAE患者脑血流发生变化时,TCD参数亦会发生相应变化[19]。TCD检查可以得到三个主要参数:血流方向、流速和动脉阻力指数,Vs、Vd、Vm均是血流速度指标,Vs可间接反映体循环总血流量,其降低提示进入脑循环的血流量不足,本研究中SAE组入院第1天Vs略低,但与对照组及本组入院第3天的数据相比,差异均无统计学意义(P>0.05),可能与脑自动调节功能有关;Vd与远端血管阻力成反比,本研究中SAE组入院第1天Vd低于对照组及入院第3天,提示SAE患者脑微循环障碍更明显,治疗后病情得到一定改善;Vm=(Vs+2Vd)/3,影响Vs及Vd的因素均可影响Vm,因此其更能反映脑灌注情况,SAE组入院第1天Vm低于对照组(P<0.05),入院第3天略改善,但差异无统计学意义(P>0.05),可能与时间较短有关。PI、RI为动脉阻力指数指标,PI升高可能代表较高的脑血管阻力,与谵妄和昏迷发生相关[9],其可能受高颅内压、与全身血栓相关的低舒张压、PaCO变化的影响[19],而本研究中患者无高颅内压且两组PaCO2比较,差异无统计学意义(P>0.05)。既往研究静态TCD参数PI、RI在SAE患者中明显升高,提示SAE患者脑灌注不足,对于SAE诊断亦有较高特异性[20],本研究进行动态监测,SAE组入院第1天PI、RI均高于对照组及入院第3天,与谈鹰等[21]研究结果一致,提示SAE患者血管顺应性更差、阻力更大,治疗后情况改善。
综上所述,SAE患者血清NSE、S-100β、Vd、Vm、PI、RI等指标存在明显变化,但治疗后有所改善,动态监测上述指标有利于了解病情变化及治疗效果。
参考文献
[1] YAO B,ZHANG L N,AI Y H,et al.Serum S100β is a better biomarker than neuron-specific enolase for sepsis-associated encephalopathy and determining its prognosis: a prospective and observational study[J].Neurochem Res,2014,39(7):1263-1269.
[2] FRASER G L,RIKER R R,COURSIN D C.Long-term cognitive impairment after critical illness[J].N Engl J Med,2014,370(2):184.
[3] EHLER J,SALLER T,WITTSTOCK M,et al.Diagnostic value of NT-proCNP compared to NSE and S100B in cerebrospinal fluid and plasma of patients with sepsis-associated encephalopathy[J].Neurosci Lett,2019,692:167-173.
[4] HALL R J,WATNE L O,CUNNINGHAM E,et al.CSF biomarkers in delirium: a systematic review[J].Int J Geriatr Psychiatry,2018,33(11):1479-1500.
[5] FENG Q,WU L,AI Y H,et al.The diagnostic value of neuron-specific enolase, central nervous system specific protein and interleukin-6 in sepsis-associated encephalopathy[J].Zhonghua Nei Ke Za Zhi,2017,56(10):747-751.
[6] ZENAIDE P V, GUSMAO-FLORES D.Biomarkers in septic encephalopathy: a systematic review of clinical studies[J].Rev Bras Ter Intensiva,2013,25(1):56-62.
[7]李康,劉博,段颖,等.血清NSE、S100β、IL-6对脓毒症相关性脑病发生率及脓毒症患者预后的影响[J].临床医学研究与实践,2019,4(1):81-82.
[8] PIERRAKOS C,ATTOU R,DECORTE L,et al.Transcranial Doppler to assess sepsis-associated encephalopathy in critically ill patients[J].BMC Anesthesiol,2014,14:45.
[9] DE AZEVEDO D S,SALINET A S M,DE LIMA OLIVEIRA M,et al.Cerebral hemodynamics in sepsis assessed by transcranial Doppler: a systematic review and meta-analysis[J].J Clin Monit Comput,2017,31(6):1123-1132.
[10]中国医师协会急诊医师分会,中国研究型医院学会休克与脓毒症专业委员会,于学忠,等.中国脓毒症/脓毒性休克急诊治疗指南(2018)[J].临床急诊杂志,2018,19(9):567-588.
[11]李德渊,王杨.脓毒症相关性脑病的诊断与治疗[J].中华实用儿科临床杂志,2017,32(6):404-408.
[12] MOLNÁR L,FÜLESDI B,NÉMETH N,et al.Sepsis-associated encephalopathy: A review of literature[J].Neurol India,2018,66(2):352-361.
[13] MAZERAUD A,RIGHY C,BOUCHEREAU E,et al.Septic-Associated Encephalopathy: a Comprehensive Review[J].Neurotherapeutics,2020,17(2):392-403.
[14]冯清,吴龙,艾宇航,等.神经元特异性烯醇化酶、中枢神经特异蛋白与白细胞介素-6在脓毒症相关性脑病中的诊断价值[J].中华内科杂志,2017,56(10):747-751.
[15] YAN S,GAO M,CHEN H,et al.Expression level of glial fibrillary acidic protein and its clinical significance in patients with sepsis-associated encephalopathy[J].Zhong Nan Da Xue Xue Bao Yi Xue Ban,2019,44(10):1137-1142.
[16] COTENA S,PIAZZA O.Sepsis-associated encephalopathy[J].Transl Med UniSa,2012,2:20-27.
[17] ALGEBALY H,ELSHERBINI S,GALAL A,et al.
Transcranial Doppler Can Predict Development and Outcome of Sepsis-Associated Encephalopathy in Pediatrics with Severe Sepsis or Septic Shock[J].Front Pediatr,2020,20(8):450.
[18] MENG L,GELB A W.Regulation of cerebral autoregulation by carbon dioxide[J].Anesthesiology,2015,122(1):196-205.
[19] RIVA N D,BUDOHOSKI K P,SMIELEWSKI P,et al.
Transcranial Doppler Pulsatility Index: What it is and What it isn’t[J].Neurocritical Care,2012,17(1):58-66.
[20]艾美林,黄立,冯清,等.经颅多普勒超聲在早期诊断脓毒症相关性脑病中的临床意义[J].中华内科杂志,2019,58(11):814-818.
[21]谈鹰,熊伟律.TCD在脓毒症患者脑循环监测中的应用及对其转归的预测价值[J].中华急诊医学杂志,2020,29(8):1087-1092.
(收稿日期:2021-06-23) (本文编辑:张爽)
