肝纤维化血清标志物与HBV-DNA联合检测在慢性乙肝疾病进程中的应用价值
2021-06-02任婷玉廖奕浪林芳楠宋春丽王大明周义文
任婷玉 廖奕浪 林芳楠 宋春丽 王大明 周义文
【摘要】 目的:探究肝纤维化标志物和HBV-DNA联合检测在慢性HBV感染后疾病进程中的应用价值。方法:回顾性分析2017年1月-2019年12月诊断为HBV携带者58例(对照组)、慢性乙型肝炎患者107例(慢性乙型肝炎组)、乙肝肝硬化患者34例(肝硬化组)的病历资料,检测并观察三组的肝纤维化标志物HA、PCⅢ、Ⅳ-C、LN和HBV-DNA载量,分析各指标之间及各指标与疾病进程的相关性,并绘制受试者工作特征(ROC)曲线。结果:肝纤维化四项指标HA、PCⅢ、Ⅳ-C、LN在对照组、慢性乙型肝炎组、肝硬化组中的含量依次增加,HBV-DNA载量在慢性乙型肝炎组中最高,其次是对照组;各指标在各组中的检测结果比较,差异均有统计学意义(P<0.05)。血清肝纤维化四项指标HA、PCⅢ、Ⅳ-C、LN之间均呈正相关关系(P<0.01),其中PCⅢ与Ⅳ-C之间为高度相关(rs=0.897,P<0.01)。血清肝纖维化四项指标HA、PCⅢ、Ⅳ-C、LN与HBV感染后疾病发展呈正相关(P<0.05),其中HA与HBV感染后疾病进程显著相关(rs=0.548,P<0.01)。HA、PCⅢ、Ⅳ-C、LN、HBV-DNA单一检测对应AUC分别为0.925、0.929、0.916、0.899、0.630,联合检测对应AUC为0.959。结论:HBV在慢性乙型肝炎患者中呈现较高水平的复制,在肝硬化阶段复制水平降低。肝纤维化四项指标在HBV感染后随着疾病发展含量升高,其含量与疾病发展呈正相关关系,HA、PCⅢ、Ⅳ-C、LN四项指标之间也具有正相关关系,其中PCⅢ与Ⅳ-C含量高度相关,HA含量与疾病进程明显相关。联合检测肝纤维化四项血清学标志物与HBV-DNA载量可提高肝纤维化的诊断效能。
【关键词】 乙型肝炎 肝纤维化 血清标志物
Application Value of Serum Liver Fibrosis Markers and HBV-DNA in Disease Progression after Chronic Hepatitis B Disease/REN Tingyu, LIAO Yilang, LIN Fangnan, SONG Chunli, WANG Daming, ZHOU Yiwen. //Medical Innovation of China, 2021, 18(10): 0-033
[Abstract] Objective: To explore the application value of HBV-DNA and serological markers for liver fibrosis on disease progression in chronic HBV infected patients. Method: From January 2017 to December 2019, the data of 58 patients with HBV carriers (control group), 107 patients with chronic hepatitis B (chronic hepatitis B group), 34 patients with chronic hepatitis B cirrhosis (cirrhosis group) were analyzed retrospectively, the levels of HA, PCⅢ, Ⅳ-C, LN in liver fibrosis markers and HBV-DNA of the three groups were detected and observed, the correlation between the indicators and the disease progression was analyzed, and the receiver operating characteristic (ROC) curve was drawn. Result: The four indexes of liver fibrosis HA, PCⅢ, Ⅳ-C and LN increased in the control group, chronic hepatitis B group and cirrhosis group successively, HBV-DNA load was the highest in the chronic hepatitis B group, followed by the control group. There were significant differences in the detection results among the indicators in each group (P<0.05). There was a positive correlation between four indexes of serum fibrosis HA, PCⅢ, Ⅳ-C and LN (P<0.01), PCⅢ was highly correlated with Ⅳ-C (rs=0.897, P<0.01). Serum liver fibrosis four indicators HA, PCⅢ, Ⅳ-C and LN were positively correlated with disease development after HBV infection (P<0.05), HA was significantly correlated with disease progression after HBV infection (rs=0.548, P<0.01). The AUC of HA, PCⅢ, Ⅳ-C, LN and HBV-DNA were 0.925, 0.929, 0.916, 0.899 and 0.630, respectively, the AUC of combined detection was 0.959. Conclusion: HBV replicates at a higher level in patients with chronic hepatitis B and decreases at the stage of cirrhosis.The four indexes of liver fibrosis increased with the development of the disease after HBV infection, and their content is positively correlated with the development of the disease. There is also a positive correlation between the four indexes of HA, PCⅢ, Ⅳ-C, and LN, among which the content of PCⅢ is highly correlated with the content of Ⅳ-C, and the content of HA is significantly correlated with the course of the disease. Combined detection of four serological markers of liver fibrosis and HBV-DNA load can improve the diagnostic efficiency of liver fibrosis.
[Key words] Hepatitis B Liver fibrosis Serum markers
First-authors address: Shenzhen Hospital of Southern Medical University, Shenzhen 518000, China
doi:10.3969/j.issn.1674-4985.2021.10.007
乙型肝炎病毒(HBV)属嗜肝DNA病毒科,是慢性乙型肝炎(CHB)的病原体[1],HBV感染已成为全球公共卫生问题[2],而中国是乙肝高发国家,据统计我国已有超过1亿人携带HBV[3]。HBV的持续感染是导致肝炎后肝硬化和肝细胞癌发生最主要的因素之一[4],慢性HBV感染者比未感染者发生肝癌的风险高出25~37倍[5]。部分HBV感染者将经历漫长的肝损伤,修复,再损伤,进而发生肝纤维化,如不及时干预,最终可能在肝硬化的基础上进展为肝细胞癌[6]。肝细胞癌是最常见的恶性肿瘤之一,恶性程度高,确诊后的5年生存率不到10%,其癌症相关死亡率已高居世界第二[7]。绝大部分肝炎病毒相关的肝细胞癌患者都经历了病毒性肝炎導致的肝损伤至肝纤维化,再到肝硬化的长期病程。一旦发展到肝细胞癌,最有效的方式只有手术治疗。由于早期诊断指标的缺乏,微小的肝癌病灶往往很难被发现,许多患者确诊时往往已经发生转移,失去手术的机会。因此定期动态评估乙肝患者感染HBV后病情的发展变化在慢性乙型肝炎的临床诊治中显得尤为重要。美国肝病学会(AASLD)2018年版慢性乙型肝炎预防、诊断和治疗指南强调了HBV-DNA连续监测和肝纤维化评估在慢性乙肝患者疾病控制中的重要性,并提出HBeAg阳性,HBV-DNA>20 000 IU/mL,且ALT<2倍正常值上限或HBeAg阴性,HBV-DNA>2 000 IU/mL,且ALT<2倍正常值上限的患者需要进行肝穿刺活检或进行肝纤维化评估来确定是否开始抗病毒治疗[8]。目前广泛应用的肝纤维化标志物即肝纤维化四项,是一种简便易行的肝纤维化评价指标[9],亚太肝病学会在2016年更新的指南中指出血清肝纤维化指标在诊断和排除肝纤维化和肝硬化方面中等可信[10]。本研究拟联合HBV-DNA载量与血清中肝纤维化标志物透明质酸(HA)、Ⅲ型前胶原蛋白(PCⅢ)、Ⅳ型胶原(Ⅳ-C)和层粘连蛋白(LN),观察其在乙肝相关疾病进程中的应用价值,现报道如下。
1 资料与方法
1.1 一般资料 选取2017年1月-2019年12月在南方医科大学深圳医院确诊的107例慢性乙型肝炎患者为慢性乙型肝炎组;34例乙肝肝硬化患者为肝硬化组;选取同期58例HBV携带者作为对照组。纳入标准:慢性乙型肝炎肝硬化诊断符合美国肝病学会(AASLD)2018年版慢性乙型肝炎预防、诊断和治疗指南。排除标准:(1)除HBV外的肝炎病毒感染以及其他原因导致的肝炎;(2)遗传代谢性疾病;(3)严重的血液疾病、脏器疾病及其他部位恶性肿瘤;(4)已实施抗病毒治疗;(5)病史及病例资料不明确。本研究通过医院伦理委员会批准。
1.2 方法 研究对象空腹抽取静脉血5 mL,
3 000 r/min离心10 min,分离血清。HBV-DNA载量测定采用荧光定量PCR法,试剂采用圣湘乙型肝炎病毒(HBV)核酸定量检测试剂盒(PCR-荧光探针法),检测结果做对数转换后进行统计分析。仪器为美国伯乐公司的CFX96型荧光定量PCR仪。HA、PCⅢ、Ⅳ-C、LN四项肝纤维化指标采用博奥赛斯化学发光免疫分析仪PETECK96-I及配套化学发光法试剂盒进行检测。严格按照试剂说明书和仪器标准操作规程检测。
1.3 观察指标与判定标准 (1)曲线下面积(AUC)评价标准:①AUC≤0.7的指标诊断价值较小;②0.7
1.4 统计学处理 采用SPSS 25.0软件对所得数据进行统计分析,偏态分布数据以M(P25,P75)表示,计量资料比较采用Kruskal-Wallis秩和检验。绘制受试者工作特征曲线(ROC曲线)并计算曲线下面积(AUC)来评价HBV-DNA载量与血清肝纤维化四项HA、PCⅢ、Ⅳ-C、LN的诊断效能,采用Spearman相关性分析了解血清肝纤维化四项指标与HBV-DNA载量之间的相关性及各项指标与HBV感染后疾病进程的相关性。以P<0.05为差异有统计学意义。
2 结果
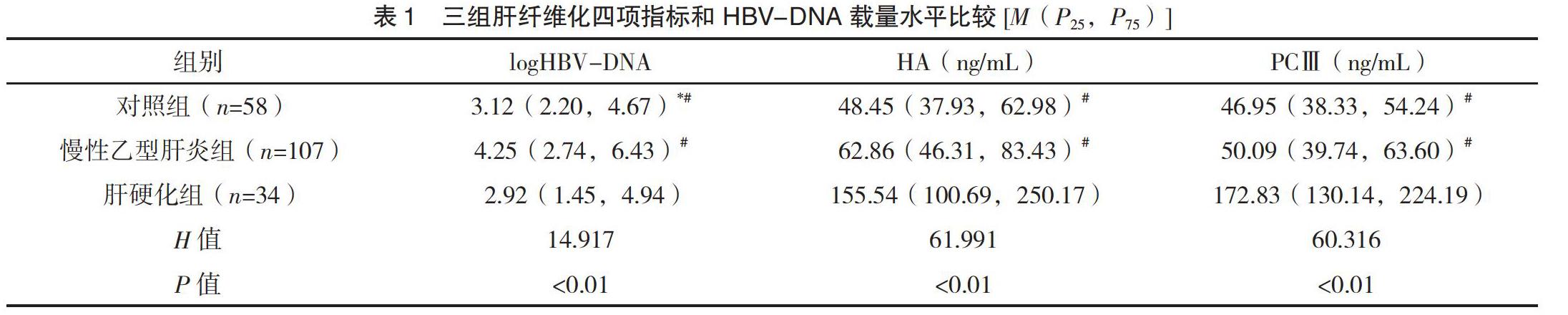
2.1 三组肝纤维化四项指标和HBV-DNA载量水平比较 肝纤维化四项指标HA、PCⅢ、Ⅳ-C、LN在对照组、慢性乙型肝炎组,肝硬化组中的含量依次增加,HBV-DNA载量在慢性乙型肝炎中最高,其次对照组;各指标在各组中的检测结果比较,差异均有统计学意义(P<0.05)。见表1。
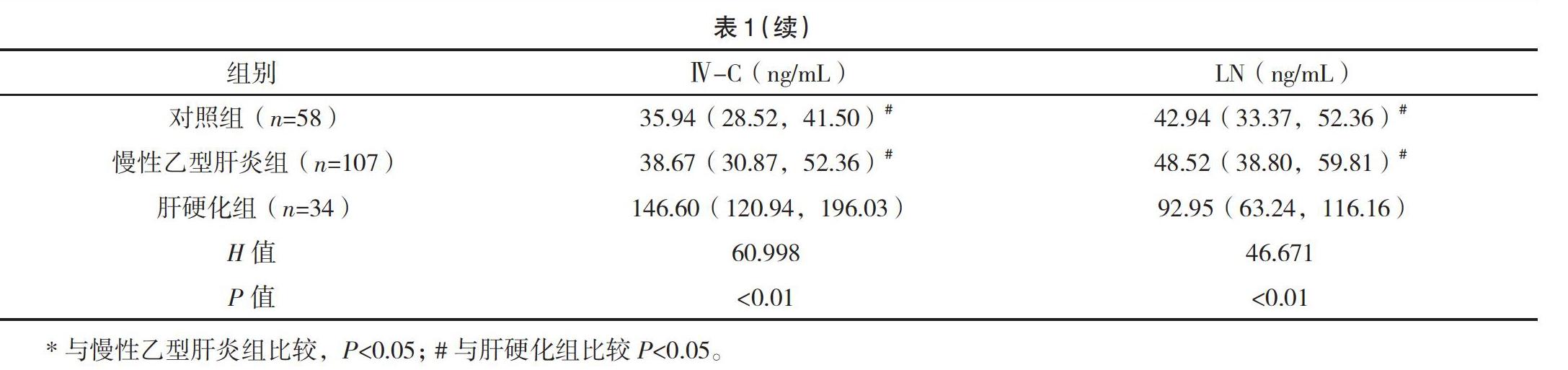
2.2 肝纤维化四项指标和HBV-DNA载量相关
性 血清肝纤维化四项指标HA、PCⅢ、Ⅳ-C、LN之间呈均呈正相关关系(P<0.01),其中PCⅢ与Ⅳ-C之间为高度相关(rs=0.897,P<0.01),但HBV-DNA载量与肝纤维化四项指标之间无相关性(P>0.05)。见表2。
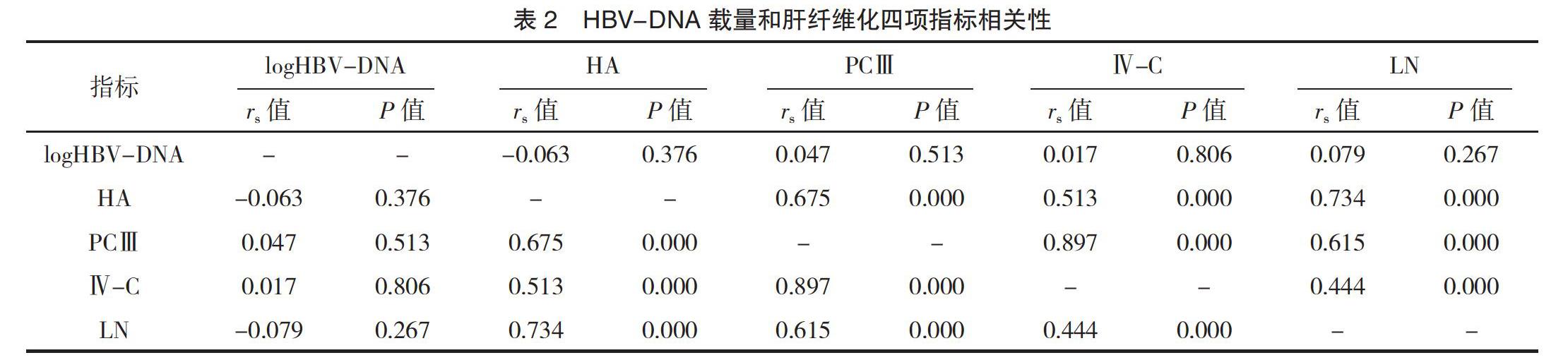
2.3 HBV-DNA载量、肝纤维化四项指标与慢性乙肝疾病发展的相关性 血清肝纤维化四项指标HA、PCⅢ、Ⅳ-C、LN与HBV感染后疾病发展呈正相关(P<0.05),其中HA与HBV感染后疾病进程明显相关(rs=0.548,P<0.01),见表3。
综上所述,肝纤维化四项指标具有较好的临床应用价值,尤其是HA与疾病进展有较好的相关性,但部分项目如PCⅢ和Ⅳ-C的特异度较差,受到的影响因素较多。HBV-DNA的检测稳定且可靠,受影响因素少,在乙型肝炎的疾病监测中发挥重要作用,但其单独应用在乙肝感染后疾病进展中的诊断作用有限,本研究发现将其与肝纤维化四项指标联合应用可提高检测的特异度,提高诊断效能,有利于实现乙肝相关肝纤维化的无创诊断。
参考文献
[1] Vittal A,Ghany M G.WHO Guidelines for Prevention,Care and Treatment of Individuals Infected with HBV:A US Perspective[J].Clin Liver Dis,2019,23(3):417-432.
[2]高春芳,吴孟超.乙型肝炎病毒感染标志物的检测现状和思考[J].中华检验医学杂志,2015,38(3):145-147.
[3] Schweitzer A,Horn J,Mikolajczyk R T,et al.Estimations of worldwide prevalence of chronic hepatitis B virus infection:a systematic review of data published between 1965 and 2013[J].Lancet,2015,386(10003):1546-1555.
[4]李海燕,孫静,杨亚娟,等.乙肝病毒X蛋白对肝星状细胞活化的影响及可能机制[J].中国老年学杂志,2018,38(13):3221-3224.
[5] Wang M,Xi D,Ning Q.Virus-induced hepatocellular carcinoma with special emphasis on HBV[J].Hepatology International, 2017,11(2):171-180.
[6] Baglieri J,Brenner D A,Kisseleva T.The Role of Fibrosis and Liver-Associated Fibroblasts in the Pathogenesis of Hepatocellular Carcinoma[J].Int J Mol Sci,2019,20(7):1723.
[7] Torre L A,Bray F,Siegel R L,et al.Global cancer statistics,2012[J].CA Cancer J Clin,2015,65(2):87-108.
[8] Terrault N A,Lok A S F,McMahon B J,et al.Update on prevention,diagnosis,and treatment of chronic hepatitis B:AASLD 2018 hepatitis B guidance[J].Hepatology,2018,67(4):1560-1599.
[9]王艳华,袁颖华.慢性乙型肝炎患者肝纤维化四项与肝炎症损伤相关生化指标的相关性分析[J].检验医学与临床,2019,16(16):2376-2380.
[10] Shiha G,Shiha G,Ibrahim A,et al.Asian-Pacific Association for the Study of the Liver (APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis:a 2016 update[J].Hepatology International,2017,11(1):1-30.
[11] Karsdal M A,Daniels S J,Holm N S,et al.Collagen biology and non-invasive biomarkers of liver fibrosis[J].Liver Int, 2020,40(4):736-750.
[12] Lu W,Zhang Y P,Zhu H G,et al.Evaluation and comparison of the diagnostic performance of routine blood tests in predicting liver fibrosis in chronic hepatitis B infection[J].Br J Biomed Sci,2019,76(3):137-142.
[13] Petitclerc L,Sebastiani G,Gilbert G,et al.Liver fibrosis:Review of current imaging and MRI quantification techniques[J].
J Magn Reson Imaging,2017,45(5):1276-1295.
[14] Xiao G,Yang J,Yan L.Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection:a systemic review and meta-analysis[J].Hepatology,2015,61(1):292-302.
[15]华琳,杨雅芸,孙维罗,等.乙型肝炎患者ALT水平与HBV血清标志物联合检测的应用价值[J].中华医院感染学杂志,2019,29(18):2746-2749,2753.
[16]沈崔琴,李万斌,雷洁雯,等.γ-谷氨酰转肽酶与血小板比率对慢性乙型肝炎肝纤维化的诊断效能[J].第二军医大学学报,2019,40(9):984-988.
[17]曾龙秀,肖朝文,孙江阳,等.慢性乙型肝炎患者炎症因子表达水平及IL-23/IL-17信号通路的活性变化[J].中华医院感染学杂志,2020,30(10):1512-1516.
[18] Polyzos S A,Slavakis A,Koumerkeridis G,et al.Noninvasive Liver Fibrosis Tests in Patients with Nonalcoholic Fatty Liver Disease:An External Validation Cohort[J].Horm Metab Res,2019,51(2):134-140.
[19] Dong H,Xu C,Zhou W,et al.The combination of 5 serum markers compared to FibroScan to predict significant liver fibrosis in patients with chronic hepatitis B virus[J].Clin Chim Acta,2018,483:145-150.
[20] Younesi S,Parsian H.Diagnostic accuracy of glycoproteins in the assessment of liver fibrosis:A comparison between laminin,fibronectin,and hyaluronic acid[J].The Turkish Journal of Gastroenterology,2019,30(6):524-531.
[21] Maurizio S L G M.Non invasive tools for the diagnosis of liver cirrhosis[J/OL].世界胃腸病学杂志:英文版(电子版),2014,20(48):18131-18150.
[22]李慧萍,郑雪琴,赵群,等.Ⅲ型前胶原、Ⅳ型胶原、层黏连蛋白和透明质酸酶在诊断肝纤维化程度中的应用[J].检验医学与临床,2019,16(5):666-668.
[23]李丹丹,杜燕娥,段亮,等.肝硬化相关血清学指标与Child-Pugh分级的关系[J].重庆医科大学学报,2019,44(3):336-339.
[24]陈琼,陈蓉,曾艺馨,等.乙型肝炎病毒感染患者HBV-DNA载量与血清及肝纤维化标志物的关系[J].中华医院感染学杂志,2017,27(15):3487-3489.
[25] Liu C,Wang L,Xie H,et al.The relationship between serum hepatitis B virus DNA level and liver histology in patients with chronic HBV infection[J].PLoS One,2018,13(11):e206060.
[26]张宇,唐世孝.血清肝纤维化指标对肝纤维化的诊断价值[J].临床肝胆病杂志,2019,35(11):2466-2471.
(收稿日期:2020-12-30) (本文编辑:刘蓉艳)
