右美托咪定联合丙泊酚全身麻醉对颅内动脉瘤栓塞术老年患者术后早期认知功能的影响
2021-03-27蔡少彦魏旸张蕾李嘉琳郑良杰郭春明
蔡少彦 魏旸 张蕾 李嘉琳 郑良杰 郭春明

【关键词】 右美托咪定 丙泊酚 颅内动脉瘤 术后认知功能障碍 老年患者
[Abstract] Objective: To investigate the effects of Dexmedetomidine combined with Propofol general anesthesia on hemodynamics, postoperative recovery and early cognitive function in middle-aged and elderly patients undergoing intracranial aneurysm embolization. Method: A total of 60 elderly patients who underwent intracranial aneurysm embolization under general anesthesia in our hospital from January to July in 2020 were selected. The patients were randomly divided into Dexmedetomidine group (group D) and control group (group C), 30 cases in each group. Group D was injected with Dexmedetomidine 0.8 μg/kg by microinjection pump before surgery, group C was injected with 0.9% Sodium Chloride Solution by micro injection pump before surgery. Blood pressure (BP), heart rate (HR) and pulse oxygen saturation (SpO2) were recorded before anesthesia induction (T0), at the beginning of surgery (T1), 10 min after surgery (T2), at the end of surgery (T3), at recovery (T4). Anesthesia time, dosage of Propofol, recovery time, recovery time of orientation and postoperative adverse reactions such as delirium, hypotension, bradycardia, respiratory depression, body movement and shivering were recorded. The simple mental state examination scale (MMSE) was used to assess the cognitive function before and after surgery between the two groups. Result: The SBP of T1 to T3 in group D were higher than those in group C, the differences were statistically significant (P<0.05). Comparison of SBP between the two groups at T0 and T4, there were no significant differences (P>0.05). HR from T1 to T4 in group D were lower than those in group C, the differences were statistically significant (P<0.05). Comparison of DBP and SpO2 of T0 to T4 between the two groups, there were no significant differences (P>0.05). The incidence of postoperative delirium in group D was significantly lower than that in group C, the difference was statistically significant (P<0.05). Comparison of the incidences of hypotension, bradycardia, respiratory depression, body motion and chills between the two groups, there were no significant differences (P>0.05). 1 d before surgery, comparison of MMSE scores between the two groups, there was no significant difference (P>0.05). 1 h, 1 d, 2 d after surgery, the MMSE scores of group D were higher than those of group C, the differences were statistically significant (P<0.05). Conclusion: During intracranial aneurysm embolization, Dexmedetomidine combined with Propofol general anesthesia can effectively maintain the hemodynamic stability of elderly patients and improve the cognitive function of elderly patients in the early stage after operation.
[Key words] Dexmedetomidine Propofol Intracranial aneurysm Postoperative cognitive dysfunction Elderly patients
First-author’s address: Shantou Central Hospital, Shantou 515031, China
doi:10.3969/j.issn.1674-4985.2021.26.011
颅内动脉瘤是蛛网膜下腔出血的首要原因,是脑血管意外发生率第三位的疾病。我国社会老龄化正日益加剧,老年患者脑血管疾病增多,需要进行颅内动脉瘤栓塞术治疗的患者也逐渐增多。颅内动脉瘤介入栓塞术由于创伤小,并发症少,术后恢复快等显著优势,已经逐渐取代传统的开颅动脉瘤夹闭术,成为急性动脉瘤破裂的首选治疗方法[1]。老年患者大脑功能减退,更易受手术创伤应激和麻醉药物的影响,导致早期术后认知功能障碍(postoperative cognitive dysfunction,POCD)。POCD发生在20%~50%的术后患者中[2],老年患者发病率较高,可高达60%[3],其可导致患者术后恢复延迟及一系列的并发症发生。研究认为,术中持续静脉泵注右美托咪定(Dexmedetomidine,DEX)能使老年患者术中低血压和术后谵妄发生率显著降低,同时对术后认知功能障碍有明显的改善作用[4],然而对右美托咪定能否改善老年患者颅内动脉瘤栓塞术术后的认知功能方面的研究,国内尚无相关报道。因此,本研究拟对老年患者颅内动脉瘤栓塞手术中应用右美托咪定复合丙泊酚全身麻醉的临床效果及术后早期认知功能的影响进行临床研究,评价其有效性及安全性,以对临床用药的选择提供参考。现报道如下。
1 资料与方法
1.1 一般资料 选择2020年1-7月在本院行全身麻醉下颅内动脉瘤栓塞术的老年患者60例。纳入标准:年龄≥60岁;ASA Ⅱ、Ⅲ级;行全身麻醉下颅内动脉瘤栓塞术。排除标准:既往严重冠心病、严重心律失常、精神疾病、昏迷或其他原因不能配合检查。将患者随机分为右美托咪定组(D组)和对照组(C组),每组30例。患者术前均签署书面知情同意书,本研究经汕头市中心医院伦理委员会许可。
1.2 方法 所有患者术前常规禁食,术前不用药。入手术室后开放上肢静脉通路,面罩吸氧5 L/min,使用M8004A型心电监护仪(Philips公司,德国)监测SBP、DBP、HR、SpO2、ECG。D组于手术开始前10 min静脉泵注盐酸右美托咪定注射液[生产厂家:扬子江药业集团有限公司,批准文号:国药准字H20183219,规格:2 mL︰0.2 mg(按右美托咪定计)]0.8 μg/kg,10 min内泵完,随后以0.2~0.5 μg/(kg·h)的速度维持泵注,手术结束前15 min停止输注;C组同样方法静脉泵注等量0.9%氯化钠溶液。麻醉诱导采用丙泊酚中/长链脂肪乳注射液(生产厂家:Fresenius Kabi Austria GmbH,注册证号:国药准字J20160098,规格:50 mL︰0.5 g)血浆浓度靶控模式,初始靶控浓度为3 mg/L,使用CP-800TCI型注射泵(思路高,中国北京),同时静脉推注枸橼酸舒芬太尼注射液[生产厂家:宜昌人福药业有限责任公司,批准文号:国药准字H20054171,规格:1 mL︰50 μg(按C22H30N2O2S计)]0.2~0.3 μg/kg、注射用苯磺酸阿曲库铵(生产厂家:上海恒瑞医药有限公司,批准文号:国药准字H20061298规格:25 mg)0.8 mg/kg。诱导插管后行机械通气控制呼吸,设置潮气量为5~6 mL/kg,呼吸频率为12~18次/min,吸呼时间比为1︰2,维持PETCO2在35~45 mmHg。术中根据麻醉深度及手术操作调节丙泊酚浓度,舒芬太尼及阿曲库铵按需间断追加。
1.3 观察指标 (1)比较两组的临床资料,包括麻醉诱导前(T0)、手术开始时(T1)、手术进行10 min时(T2)、手术结束时(T3)、苏醒时(T4)的SBP、DBP、HR、SpO2,比较两组麻醉时间、丙泊酚用量、苏醒时间、定向力恢复时间。(2)比较两组不良反应发生情况,记录两组低血压(SBP<90 mmHg)、心动过缓(HR<55次/min)及呼吸抑制(SpO2<90%)、谵妄、体动、寒战的发生情况。(3)比较两组不同时间点认知功能,在术前1 d和术后1 h、1 d、2 d由同一麻醉医生采用简易精神状态检查量表(mini-mental state examination,MMSE)评定患者认知功能。MMSE量表由30个问题组成,包含回忆能力、语言能力、定向力、记忆力、注意力及计算力等方面内容,总分为30分。
1.4 统计学处理 采用SPSS 22.0软件对所得数据进行统计分析,计量资料用(x±s)表示,比较采用t检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 两组性别、ASA分级、年龄、体重、麻醉时间、丙泊酚用量、苏醒时间、定向力恢复时间比较,差异均无统计学意义(P>0.05),具有可比性,见表1。
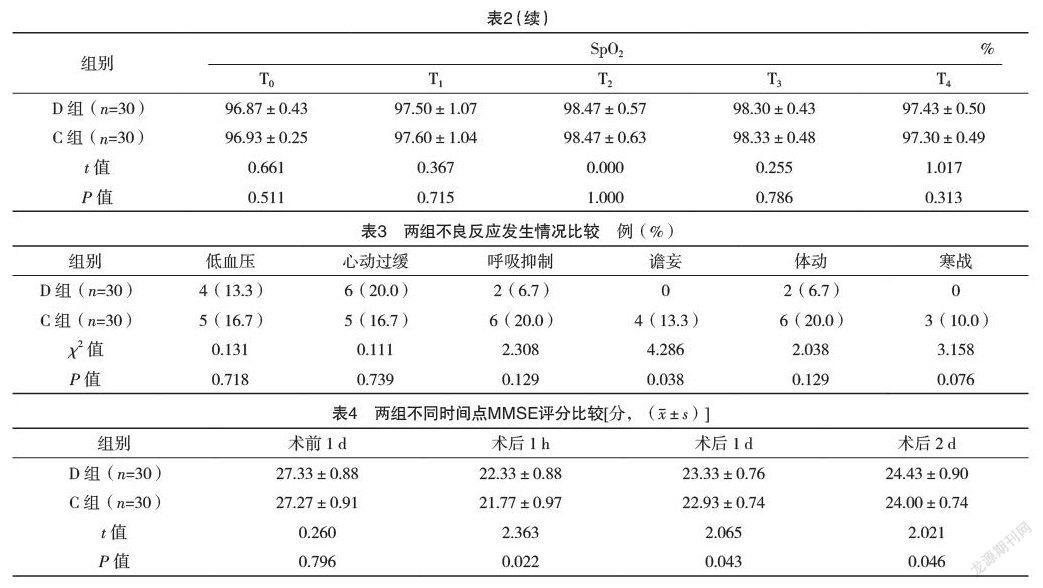
2.2 两组SBP、DBP、HR及SpO2水平比较 D组T1~T3的SBP均高于C组,差异均有统计学意義(P<0.05);两组T0、T4时的SBP比较,差异均无统计学意义(P>0.05)。D组T1~T4的HR均低于C组,差异均有统计学意义(P<0.05);两组T0~T4的DBP、SpO2比较,差异均无统计学意义(P>0.05)。见表2。
2.3 两组不良反应发生情况比较 D组术后谵妄发生率显著低于C组,差异有统计学意义(P<0.05);两组低血压、心动过缓、呼吸抑制、体动、寒战发生率比较,差异均无统计学意义(P>0.05)。见表3。
2.4 两组不同时间点MMSE评分比较 术前1 d,两组MMSE评分比较,差异无统计学意义(P>0.05);术后1 h和术后1、2 d,D组MMSE评分均高于C组,差异均有统计学意义(P<0.05)。见表4。
3 讨论
老年患者由于自身呼吸功能减退,呼吸抑制和缺氧的发生率往往很高[5]。研究表明,在全身麻醉中全麻药联合应用右美托咪定,可以减轻机体应激反应,使麻醉期间血流动力学更加平稳,同时还可以减少其他麻醉药的用量[6]。
POCD是术后发生的一种以认知功能缺损为主的中枢神经系统并发症,表现为焦虑、精神错乱、记忆减退或人格改变,影响术后患者的康复,甚至造成其他并发症,导致老年性痴呆[7]。POCD的发病原因尚不明确,高龄、手术、麻醉药物的使用、术后疼痛、激素水平及炎症反应均与POCD的发生关系密切,且在老年患者和伴有血管疾病及心力衰竭的患者中发病率较高[8]。老年患者由于脑血管退行性病变,脑神经细胞数量减少及中枢神经系统的功能储备下降,POCD发生率更高。目前POCD尚无效果确切的治疗方法,术后POCD的防治已然成为国内外学者研究的热点。右美托咪定属于咪唑类衍生物,是一种新兴的高度选择性α2受体激动剂,能发挥抗交感活性、镇静、镇痛及神经保护等效应[9],对术后POCD的发生具有潜在防治作用,但其是否可以预防颅内动脉瘤栓塞术老年患者POCD的发生尚不明确。
报道显示,右美托咪定对POCD的干预作用可能与减少脑细胞凋亡、改善脑神经功能有关[10];右美托咪定的應用同时也加强了镇痛、镇静作用,降低了疼痛引起POCD发生的风险。右美托咪定可减轻老年微创冠状动脉搭桥术患者单肺通气时SpO2的下降,改善术后认知功能,降低POCD的发生率[11]。右美托咪定能明显改善老年结直肠癌患者术后认知功能障碍,认知功能障碍的发生受年龄、麻醉时间、术中出血量及IL-6和S-100β高表达的影响[12]。也有学者认为右美托咪定可降低老年患者术后早期认知功能障碍的发生率,与改善术后镇痛效果和改善脑氧代谢有关[13]。Cheng等[14]研究发现,右美托咪定能减轻65岁或65岁以上患者术后立即出现的谵妄和术后3 d出现的认知功能障碍,同时可降低在择期开腹手术7 d后的认知功能障碍率,认知能力优于安慰剂,最多可达术后1个月;同时还指出右美托咪定降低了新发心律失常及肺部感染的发生率。术后血清脑源性神经营养因子的减少与认知功能障碍呈相关性,提示脑神经营养因子浓度降低。右美托咪定可逆转麻醉所致脑源性神经营养因子在血液中的浓度降低,这与右美托咪定的神经保护作用相关。与绝对血清脑源性神经营养因子水平相比,基线下降的相对值是一个与神经保护作用更相关的预测因素,对评估POCD具有良好的敏感性和特异性[15]。研究表明给予右美托咪定使观察组的精神错乱、昏迷等发生率显著低于对照组,且生存时间延长[16]。对于非心脏手术后入住ICU的老年人,小剂量右美托咪定输注不会显著改变3年总生存期,但可将生存期提高到2年,并改善3年生存者的认知功能和生活质量[17]。
关于POCD的诊断,临床上应用最广的是神经心理学测定。MMSE是目前最常应用的检测认知功能的量表,其简单易行,应用范围较广。该量表总分共30分,共30项题目,每项回答正确得1分,分数越高表示认知功能越好[18]。本研究结果显示,D组T1~T3的SBP均高于C组,差异均有统计学意义(P<0.05);两组T0、T4时的SBP比较,差异均无统计学意义(P>0.05)。D组T1~T4的HR均低于C组,差异均有统计学意义(P<0.05);两组T0~T4的DBP、SpO2比较,差异均无统计学意义(P>0.05)。D组术后谵妄发生率显著低于C组,差异有统计学意义(P<0.05)。术前1 d,两组MMSE评分比较,差异无统计学意义(P>0.05);术后1 h和术后1、2 d,D组MMSE评分均高于C组,差异均有统计学意义(P<0.05),即D组术后1 h到2 d的术后认知功能均较对照组高。此结果提示,右美托咪定能够改善术后早期老年患者的认知功能。
综上所述,颅内动脉瘤栓塞患者应用右美托咪定联合丙泊酚全身麻醉,可使老年患者血流动力学更平稳,降低患者围术期心血管不良事件的发生率,同时可改善术后早期MMSE评分,改善老年患者术后早期认知功能,有利于颅内动脉瘤栓塞术后患者认知功能的恢复。
参考文献
[1] Jabbarli R,Dinger T F,Darkwah Oppong M,et al.Risk Factors for and Clinical Consequences of Multiple Intracranial Aneurysms: A Systematic Review and Meta-Analysis[J].Stroke,2018,49(4):848-855.
[2] Li X,Yang J,Nie X L,et al.Impact of dexmedetomidine on the incidence of delirium in elderly patients after cardiac surgery: A randomized controlled trial[J/OL].PLoS One,2017,12(2):e0170757.
[3] Deiner S,Luo X,Lin H M,et al.Intraoperative Infusion of Dexmedetomidine for Prevention of Postoperative Delirium and Cognitive Dysfunction in Elderly Patients Undergoing Major Elective Noncardiac Surgery: A Randomized Clinical Trial[J/OL].JAMA Surg,2017,152(8):e171505.
[4]尹红吴健,陈卫民.小剂量右美托咪啶持续输注对全麻高血压患者血流动力学的影响[J].临床麻醉学杂志,2013,29(12):1181-1183.
[5] Zhang J,Chen L,Sun Y,et al.Comparative effects of fentanyl versus sufentanil on cerebral oxygen saturation and postoperative cognitive function in elderly patients undergoing open surgery[J].Aging Clin Exp Res,2019,31(12):1791-1800.
[6] Nair A S.Benefits of using dexmedetomidine during carotid endarterectomy: A review[J].Saudi J Anaesth,2014,8(2):264-267.
[7]孟海兵,来伟,帅君.右美托咪定对老年患者全麻术后认知功能及炎症因子的影响[J].实用医学杂志,2014,30(14):2300-2301.
[8] Pysyk C L.Factors for perioperative delirium[J].Br J Anaesth,2014,112(3):577-578.
[9]李跃祥,戴华春.右美托咪定对老年患者全麻术后认知功能障碍的影响[J].临床麻醉学杂志,2014,30(10):964-967.
[10] Kose E A,Bakar B,Kasimcan O,et al.Effects of intracisternal and intravenous dexmedetomidine on ischemia-induced brain injury in rat: a comparative study[J].Turk Neurosurg,2013,23(2):208-217.
[11] Gao Y,Zhu X,Huang L,et al.Effects of dexmedetomidine on cerebral oxygen saturation and postoperative cognitive function in elderly patients undergoing minimally invasive coronary artery bypass surgery[J].Clin Hemorheol Microcirc,2020,74(4):383-389.
[12] Zhang J,Liu G,Zhang F,et al.Analysis of postoperative cognitive dysfunction and influencing factors of dexmedetomidine anesthesia in elderly patients with colorectal cancer[J].Oncol Lett,2019,18(3):3058-3064.
[13] Lu J,Chen G,Zhou H,et al.Effect of parecoxib sodium pretreatment combined with dexmedetomidine on early postoperative cognitive dysfunction in elderly patients after shoulder arthroscopy: A randomized double blinded controlled trial[J].J Clin Anesth,2017,41:30-34.
[14] Cheng X Q,Mei B,Zuo Y M,et al.A multicentre randomised controlled trial of the effect of intra-operative dexmedetomidine on cognitive decline after surgery[J].Anaesthesia,2019,74(6):741-750.
[15] Chen J,Yan J,Han X.Dexmedetomidine may benefit cognitive function after laparoscopic cholecystectomy in elderly patients[J].Exp Ther Med,2013,5(2):489-494.
[16] Kazmierski J,Banys A,Latek J,et al.Raised IL-2 and TNF-α concentrations are associated with postoperative delirium in patients undergoing coronary-artery bypass graft surgery[J].Int Psychogeriatr,2014,26(5):845-855.
[17] Zhang D F,Su X,Meng Z T,et al.Impact of Dexmedetomidine on Long-term Outcomes after Noncardiac Surgery in Elderly: 3-Year Follow-up of a Randomized Controlled Trial[J].Ann Surg,2019,270(2):356-363.
[18] Pendlebury S T,Markwick A,de Jager C A,et al.Differences in cognitive profile between TIA, stroke and elderly memory research subjects: a comparison of the MMSE and MoCA[J].Cerebrovasc Dis,2012,34(1):48-54.
(收稿日期:2020-11-27) (本文編辑:姬思雨)
