Resection of a retrohepatic leiomyosarcoma of the inferior vena cava combined with caudate lobectomy and reconstruction with an allogenic vein
2021-03-05XinXueZhangJiQiaoZhuHuiZhangJianTaoKouJunMaQiangHe
Xin-Xue Zhang , Ji-Qiao Zhu , Hui Zhang, Jian-Tao Kou, Jun Ma, Qiang He
Department of Hepatobiliary and Pancreaticosplenic Surgery, Beijing Chaoyang Hospital, Capital Medical University, Beijing 10 0 020, China
Primary leiomyosarcoma of the inferior vena cava (IVC) is a rare disease, accounting for 0.5% of soft tissue sarcomas in adults [1]. A diversity of therapeutic methods have been applied to treat this type of tumor. The average survival time of patients who are not treated is merely 3-4 months [2]. The effect of radiotherapy and chemotherapy remains unclear and controversial [3]. On the other hand, theen-blocresection with negative margins may be the only potentially curative treatment and therefore, can contribute to the long-term survival of the patients [4]. During the operation, a reconstruction graft for the defected IVC needs to be chosen [5]as the graft-related complications are the surgeons’ major concern,which include graft thrombosis and infection [6]. Growing evidence has suggested that an allogeneic vein from donation after brain death or cardiac death is a better choice to avoid these complications [7]. An allogeneic vein has been reported to be safely used in patients with pancreatic cancer in case of the portal vein and/or superior mesenteric vein invasion [8]. A cryopreserved allograft can even be applied in the management of native and prosthetic aortic infections [7]. Herein, we present a case of resection of a retrohepatic leiomyosarcoma of the IVC combined with partial caudate lobectomy and reconstruction with an allogeneic vein.
A 44-year-old woman presented to our hospital with a sevenmonth history of discontinuous back pain in the right scapular region, aggravated by emotion and alleviated by rest. There were no other symptoms. Physical examination was normal. Serum aspartate aminotransferase was increased to 113 IU/L (reference range,15 to 40 IU/L) and serum alanine aminotransferase to 103 IU/L (reference range, 9 to 50 IU/L). Other laboratory data were within normal ranges. No abnormalities were found in electrocardiography and chest X-ray. A contrast-enhanced computed tomography (CT)scan for further evaluation was performed. Distant metastasis was not detected. An irregular soft-tissue lesion filled the IVC and extended from the right renal vein to the middle hepatic vein, measuring approximately 5 cm in length and 3 cm in diameter with heterogeneous enhancement in dual-phase ( Fig. 1 ).

Fig. 1. Anterior view of 3-dimensional reconstructed image of pre-operative CT. The mass was located at the retrohepatic portion of IVC. IVC: inferior vena cava; CT:computed tomography.
The patient underwent the surgery with an inverted “L” incision. On exploration, there was no evidence of metastasis or peritoneal nodularity. The tumor appeared to arise from the posterior wall of the cava and was mainly located within the lumen ( Fig. 2 ).To fully expose the IVC, the left lobe of the liver was mobilized off the IVC by dividing and ligating the perihepatic ligament and the caudate lobe was then resected for IVC resection and reconstruction. After that, the IVC was occluded using a vena cava clamp.The retrohepatic IVC along with the tumor was totally resected and removed. The IVC was reconstructed without veno-venous bypass using a 6.5 cm cryopreserved iliac vein ( Fig. 3 ) which had the matched diameter. The time of IVC clamping was 48 minutes and the operative time was 465 minutes. The intraoperative blood loss was 400 mL without blood transfusion. The excised specimens were sent to the pathology department for further diagnosis. 40 0 0 Axa IU low-molecular-weight heparin calcium was injected subcutaneously once a day for the first 2 weeks after surgery when there was no sign of bleeding. After that, 100 mg oral aspirin was taken per day to prevent venous thrombosis. The postoperative CT imaging showed that IVC was patent ( Fig. 4 ). The patient had a satisfactory postoperative recovery. The histology result revealed that an R0 resection was achieved. The patient did not develop metastases or any recurrence over a 2-year follow-up.

Fig. 2. The surgical field before removal of the tumor.
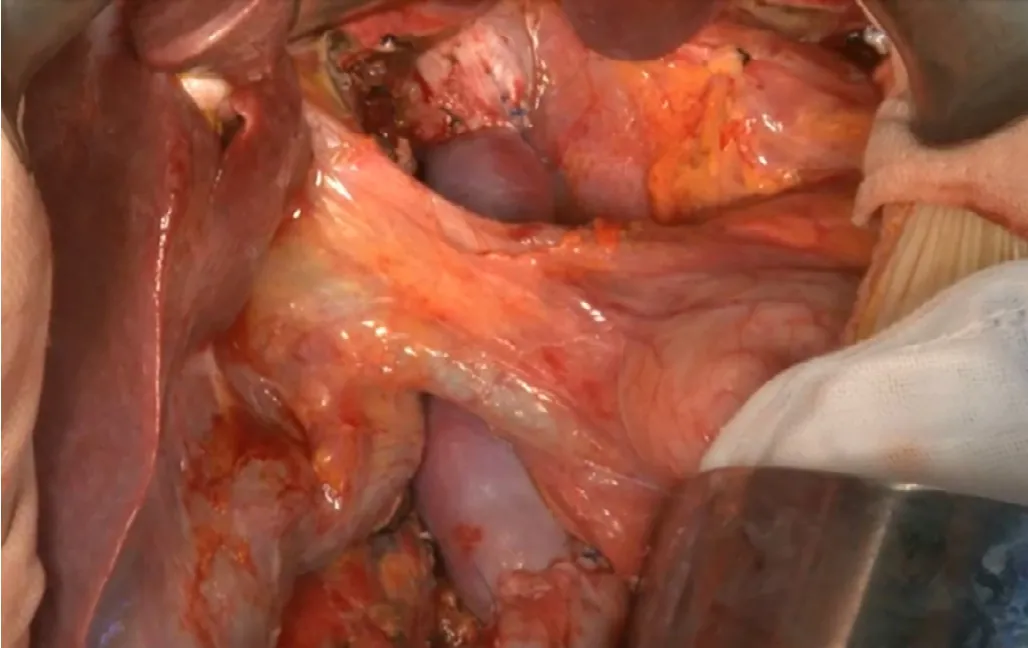
Fig. 3. The IVC was reconstructed using a cryopreserved iliac vein. IVC: inferior vena cava.

Fig. 4. Anterior view of 3-dimensional reconstructed image of post-transplant CT.The retrohepatic IVC was patent. CT: computed tomography.
Radical resection may be the only chance to prolong the survival time of patients with primary leiomyosarcoma of the IVC [4].After resection whether to reconstruct the IVC depends on the establishment of collateral circulation. A study has reported that it is not necessary to reconstruct the IVC, when a retroperitoneal flow has already been established [9]. In contrast, there were not any preoperative or intraoperative data indicating a collateral circulation in our case. Therefore, we performed reconstruction with allogeneic vein during the surgery.
Presently, several materials can be used for IVC reconstruction, including 1) autologous grafts, i.e. a saphenous vein or a peritoneum [10]; 2) a xenograft, i.e. a bovine pericardium; and 3) a prosthetic graft [5]. However, these materials all have some disadvantages. The effect of a saphenous vein on repairing the large-scale defected IVC is limited because of the insufficient caliber [10]. The bovine pericardium is often used for recurrent vascular stenosis but the primary patency at 2 years is reported to be only 54% [11]. Although polytetrafluoroethylene (PTFE) is most commonly used, the incidence of venous thrombosis and infection after reconstruction is high [4]. Hardwigsen et al. found that the occlusion rate of PTFE could reach as high as 25% following resection and reconstruction of the IVC [12]. Guntani et al. reported that the patency rate of PTFE with a distal vein cuff, which was used in the femorotibial artery bypass for patients with critical limb ischemia, was only 35.8% at 3 years [13].
Various studies [ 7 , 8 ]have proved that an allogeneic vessel can be used safely in this specific setting with an excellent outcome.A fresh venous allograft was used for patch closure in patients undergoing pancreaticoduodenectomy with no graft thrombosis or stenosis [8]. In our center, an allogeneic vein has been applied in patients with pancreatic cancer for the reconstruction of the portal vein and/or superior mesenteric vein. The long-term patency rate of the graft was 90% [14]. In this case, we also used the allogeneic vein to reconstruct the defected IVC in the absence of an extracorporeal bypass. No graft-related complications occurred. It is possible that poor survival may limit the occurrence of thrombosis. However, there have been numerous reports that thrombosis after allovascular reconstruction ranged from 2 days to 8 months [ 14 , 15 ], while our patient did not develop thrombosis,metastases or any recurrence over a 2-year follow-up. We believe that reconstruction with an allogeneic vein is safe based on our researches.
Full exposure of the surgical field is an important step during resection of leiomyosarcoma of the retrohepatic IVC because the failure to obtain a negative margin can inevitably increase the incidence of tumor recurrence [15]. Normally, a hemihepatectomy combined with caudate lobectomy is performed to fully expose the operative field [1]. However, in a bid to reduce liver function damage only the caudate lobe was resected in this case. Therefore,postoperative liver function was not significantly affected. Moreover, postoperative pathology confirmed a negative surgical margin. This method is helpful for patient recovery.
In conclusion, resection of a retrohepatic leiomyosarcoma of the IVC combined with caudate lobectomy and reconstruction with an allogeneic vein is safe and feasible. It can serve as an alternative treatment.
Acknowledgments
None.CRediT authorship contribution statement
Xin-Xue Zhang:Writing - original draft.Ji-Qiao Zhu:Writing -original draft.Hui Zhang:Data curation.Jian-Tao Kou:Data cura-tion.Jun Ma:Data curation.Qiang He:Conceptualization, Writing- review & editing.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient, as required by the Institutional Review Board of Beijing Chaoyang Hospital. The consent was obtained from the patient for publication of this report.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Liver transplantation and BCLC classification: Limitations impede optimum treatment
- Do the existing staging systems for primary liver cancer apply to combined hepatocellular carcinoma-intrahepatic cholangiocarcinoma?
- Overlap of concurrent extrahepatic autoimmune diseases is associated with milder disease severity of newly diagnosed autoimmune hepatitis
- Aggressive surgical approach in patients with adrenal-only metastases from hepatocellular carcinoma enables higher survival rates than standard systemic therapy
- Integrating transcriptomes and somatic mutations to identify RNA methylation regulators as a prognostic marker in hepatocellular carcinoma
- The utility of two-dimensional shear wave elastography and texture analysis for monitoring liver fibrosis in rat model