Role of routine check-up in the prognosis of patients with pancreatic cancer: A puzzling phenomenon
2021-03-05CongYingSongYnShenYunQingLu
Cong-Ying Song , , , Yn Shen , Yun-Qing Lu , , ,
a Department of Emergency Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
b Department of Geriatric Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
c Zhejiang Provincial Key Laboratory for Diagnosis and Treatment of Aging and Physic-chemical Injury Diseases, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
d Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
Keywords:Pancreatic cancer Routine check-up Early detection Survival rate
ABSTRACT Background: The high coverage of annual routine health check-up in China is a unique phenomenon throughout the world. However, its clinical value is controversial. In this cohort study, we chose pancreatic cancer as a disease model to explore the role of routine check-up in the prognosis of patients with pancreatic cancer.Methods: Data from 157 patients who were diagnosed with pancreatic cancer between January 2010 and April 2014 were collected. Patients were divided into two groups depending on how their disease was detected. Group A ( n = 85): Patients were diagnosed with pancreatic cancer in clinic visits. Group B ( n = 72): Patients were diagnosed with pancreatic cancer in routine check-ups. We compared their prognosis.Results: The tumor stage in group B was earlier than that in group A. The 1-year survival rate in group B was significantly higher than that in group A (74.6% vs. 42.4%, P < 0.001), while the 3- and 5-year survival rates of the two groups showed no significant difference ( P > 0.05). The difference of overall survival time between the two groups was not significant (22.0 vs. 9.0 months, P = 0.078).Conclusions: The stage of pancreatic cancer diagnosed in routine check-ups was earlier and therefore, the intervention was earlier which improved short-term survival rate. However, early intervention did not improve overall survival in the long-term.
Introduction
At the beginning of this century, the Chinese government has proposed a health management project, which suggested that citizens should have routine health check-up at least once a year. Relevant legal provisions have been passed and massive investments have been made to carry out this big project. Its main aim is to detect diseases early enough to cure the patients when feasible. Now the annual routine check-up is widely accepted. The routine medical check-ups include routine blood examination, tumor marker examination, liver and kidney function, electrocardiogram, echocardiogram, abdominal ultrasound, computed tomography (CT) scans,and so on. Although routine check-up has little value in identifying acute diseases [ 1 , 2 ], increasing evidence has shown the effects of early detection on some diseases, such as diabetes,cardiovascular diseases, liver diseases, gynecological diseases and malignancy [3–7]. However, can a routine check-up bring benefits to patients’ prognosis, and what effect it has on the final prognosis? Does it have equal value for different diseases? Several questions regarding the clinical value of routine check-ups have not been answered yet and no consensus reached on these issues.Hence, it is urgent to estimate its value in early detection of diseases and improving clinical outcomes.
Pancreatic cancer is one of the deadliest malignancies, and the overall mortality to incidence ratio is 0.98 [8]. In the United States, pancreatic cancer is expected to rank from the fourth to the second leading cause of cancer-related death by 2020 [9].Like most countries, the incidence of pancreatic cancer in China is increasing [10]. Although there have been dramatic improvements in treatment strategies used for malignant tumors, pancreatic cancer has not benefited from these medical advances. Due to the rapid progression of this disease and the lack of effective tests for early diagnosis, pancreatic cancer remains a great health burden worldwide.

Fig. 1. Flowchart of patients screening.
Both early, accurate diagnosis and early intervention are important for individuals with pancreatic cancer. Receiving routine check-up may be the most effective way to detect pancreatic cancer at an early stage. However, early pancreatic cancer detection by imaging tests is difficult because of the pancreas location, which makes it hidden from the view. Besides, patients with pancreatic cancer are frequently asymptomatic at an early stage, and most patients are diagnosed at the advanced stages. Currently, the only curative treatment option is surgery. Unfortunately, less than 20%of the patients are considered for surgery because most of them are at an advanced stage at the time of diagnosis [11–13]. Even so, the benefit of surgery is still limited, since the 5-year survival rate of patients who undergo surgery is approximately 20% due to the high-risk of disease recurrence after surgery [ 14 , 15 ]. Considering these characteristics, the benefits of early intervention in improving overall survival in patients with pancreatic cancer remains controversial. Therefore, we performed this study to explore the value of routine check-up for pancreatic cancer and to determine whether it can prolong patients’ survival time.
Patients and methods
Study population
We enrolled patients who were diagnosed with pancreatic cancer and admitted to the First Affiliated Hospital, Zhejiang University School of Medicine between January 2010 and April 2014.Fig. 1 showed the concrete procedures of screening patients. We excluded patients who had other malignancies or those who had received therapy for pancreatic cancer in other hospitals. Patients with an unknown month of diagnosis or other important information missing were also excluded. Finally, 157 patients were included in this study. The patients were divided into two groups based on whether they had their disease detected by routine check-ups or on clinic visits. Patients in group A (n= 85) were diagnosed in clinic visits because of obvious symptoms. Others diagnosed from routine check-ups were assigned to group B (n= 72).
Data collection
We collected patient demographics and clinical characteristics,including age at diagnosis, sex, smoking and drinking status, primary tumor site, type of therapy, and other relevant data. The time to hospital visit was defined as the period between detecting cancer by screening or having symptoms and the first visit to hospital for pancreatic cancer. The tumor-node-metastasis (TNM) stage was determined according to the 8th edition of staging system for pancreatic cancer published by the American Joint Committee on Cancer (AJCC) [16]. All laboratory and imaging data were the first test results after admission. The follow-up data of patients were obtained either through hospital records or by contacting their family members. Overall survival was defined as the time from the diagnostic date to death or the day of last follow-up.
Statistical analysis
SPSS statistical software package (version 20.0, SPSS Inc., IBM,Chicago, IL, USA) was used for statistical analysis. Continuous variables were presented as median with interquartile range (IQR).Categorical variables were expressed as number and percentage of the group from which they were derived. Independent samplet-test or Mann-WhitneyUtest was used to evaluate continuous data and Chi-square test was used to analyze categorical variables. Survival curves were plotted by the Kaplan-Meier method and compared by the log-rank test. Variables withP<0.05 were selectedto perform Cox regression analysis to identify the prognostic factors for pancreatic cancer. APvalue<0.05 was considered statistically significant.
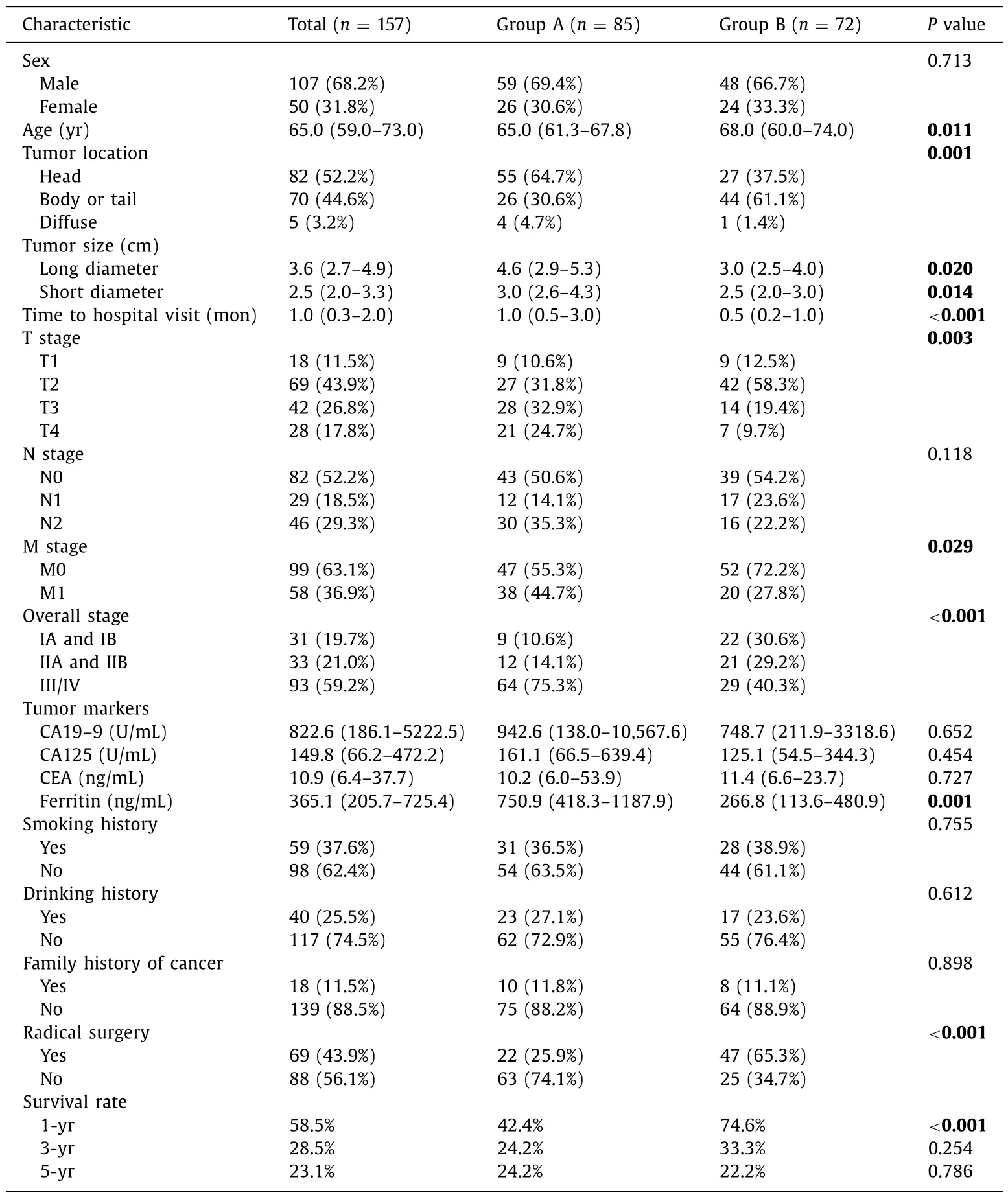
Table 1 Patients characteristics.
Results
Baseline characteristics
A total of 157 patients were included in our study, which comprised 107 (68.2%) males and 50 (31.8%) females. The median age of all patients was 65.0 years (IQR 59.0–73.0). Patients in group B were older than those in group A (68.0 vs. 65.0 years,P= 0.011).Most patients (64.7%) in group A had a tumor at the head of the pancreas, while the majority of those (61.1%) in group B had a tumor at the body or tail of the pancreas. The tumor stage in group B was earlier than that in group A. Patients who had abnormal signals detected by routine check-up usually went to hospital earlier than those who hadn’t, with the median time to hospital of 0.5 month and 1 month, respectively (P<0.001), thus group B got earlier diagnosis and received timely therapy. In addition, the tumor size in group B was smaller than that in group A. Comparing tumor markers, we found that ferritin level was lower in group B than that in group A (266.80 vs. 750.90 ng/mL,P= 0.001), while the levels of carbohydrate antigen 19–9 (CA19–9), carbohydrate antigen 125 (CA125), and carcinoembryonic antigen (CEA) were not significantly different between the two groups. There were no significant differences in sex, smoking history, drinking history, or family history of cancer between the two groups ( Table 1 ). The main clinical characteristics of patients in group A were listed in Table 2 . The considerable part of patients had abdominal pain (97.6%) and abdominal distension (52.9%). Some of them had symptoms of yellow urine (23.5%), jaundice (18.8%), nausea and vomiting (18.8%), and anorexia (16.5%). Other symptoms like low back pain, emaciation,hypodynamia, and diarrhea were also observed.
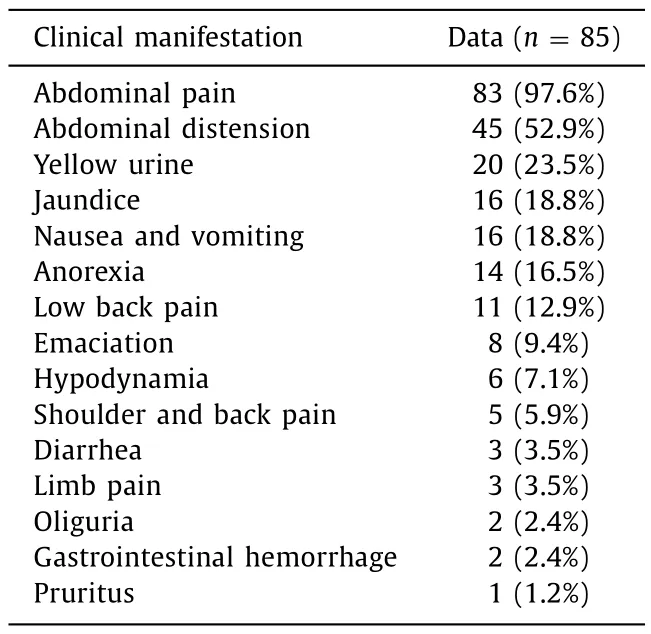
Table 2 The main clinical manifestations of patients were diagnosed with pancreatic cancer in clinic visits.
Routine check-up procedures
Of 72 patients in group B, none had a family history of pancreatic cancer or hereditary pancreatitis, thus they may not be considered as individuals at high-risk of pancreatic cancer. In 49 patients(68.1%) in group B, space-occupying lesions in the pancreas were detected by imaging methods, among these by ultrasonic imaging in 33 patients, by CT in 15 patients, and by magnetic resonance imaging (MRI) in 1 patient. In the rest of 23 patients (31.9%), elevated levels of cancer biomarkers (CA19–9) were found during routine check-up.
Pancreatic cancer patients diagnosed in routine check-up received treatment at an earlier stage
We further explored the value of routine check-up in the early detection of pancreatic cancer. More patients in group B had T1 or T2 stages compared with those in group A (70.8% vs. 42.4%,P= 0.003), while more patients in group A had distant metastases than those in group B (44.7% vs. 27.8%,P= 0.029). According to the classification, IA and IB were considered to be early stages, IIA and IIB intermediate stages, and III/IV the late stage. More patients in group B than in group A were at early stage (30.6% vs. 10.6%),while more patients in the group A than in group B were at late stage (75.3% vs. 40.3%). These results indicated that routine checkup helped patients with earlier diagnosis and early intervention.Not surprisingly, patients in group B had a higher radical surgery rate than those in group A (65.3% vs. 25.9%,P<0.001).
Early intervention improves 1-year survival rate but not the long-term survival rate
To explore the influence of early intervention on overall survival, we calculated the survival rate at different time points. Patients in group B had a significantly higher 1-year survival rate than those in group A (74.6% vs. 42.4%,P<0.001), while 3- and 5-year survival rates of the two groups showed no significant differences ( Table 1 ). Thus, we inferred that early intervention improved the short-term survival rate of patients with pancreatic cancer but not the long-term overall survival even if they were at an earlier tumor stage at the time of diagnosis.
Kaplan-Meier survival curves were shown in Fig. 2 . Patients in group A had the median survival time of 9.0 months and those in group B of 22.0 months ( Fig. 2 A). However, no statistically significant difference in survival was detected using the log-rank test (P= 0.078). Since different treatments would affect prognosis, stratification was performed according to whether patients received radical surgery or not ( Fig. 2 B, C). Among patients who received radical surgery, the median survival time was 20.0 months for group A and 35.0 months for group B (P= 0.354). Among patients who received other treatments, group A had median survival time of 6.0 months and group B of 9.0 months (P= 0.556). Interestingly, when we performed a survival analysis for patients based on whether they had undergone radical surgery or not, we found that receiving radical surgery could improve survival time (29 vs.6 months,P<0.001) ( Fig. 2 D).
Cox regression analysis was performed to find the prognostic factors for pancreatic cancer. As shown in Table 3 , overall stage and receiving radical surgery were the factors affecting the prognosis of patients. However, receiving or not receiving routine check-up seemed to have limited influence on the overall survival.
Complications and tumor recurrence or metastasis after surgery
A total of 69 patients received radical surgery, including 22 patients in group A and 47 patients in group B. None of them received neoadjuvant chemotherapy, and 15 patients (21.7%) received adjuvant chemotherapy. Since postoperative complications and recurrence could affect the patient’s prognosis, we noticed that for 69 patients who received radical surgery, postoperative complications occurred in 25 (36.2%) patients, among which, 10 patients(40.0%) had pancreatic fistula. Other complications included intraabdominal bleeding, gastrointestinal hemorrhage, gastroparesis, incisional infection, and secondary diabetes. Moreover, 8 patients(11.6%) had metastasis, and 5 patients (7.2%) had tumor recurrence.
Discussion
The present study found that detecting cancer by routine checkup prompted the patients to go to hospital sooner and get an early diagnosis. In addition, the earlier tumor stage always gave them more chance of surgery, which suggested that early detection and early diagnosis gain more time for early aggressive therapy. It might explain why patients who had pancreatic cancer detected by routine check-up had a higher 1-year survival rate.
However, our study suggested that early intervention had no significant influences in patients’ overall survival in the long-term.Early detection helped patients receive early treatment. However,the long-term survival benefit was limited. There are a few possible reasons for that. Firstly, the detection of pancreatic cancer by routine check-up was not done early enough. According to the data collected, 40.3% of the patients in group B were at the stage III or IV, which are advanced tumor stages. This proportion is still quite high. Considering the rapid progression of the disease, the extra time gained by routine check-up seemed insignificant. Meanwhile,although routine check-up could increase the surgery rate, postoperative complications are common, cancer metastasis and recurrence rates after curative resection are still high. The 5-year survival rate of patients who underwent surgery remained low, indicating that the occult metastatic disease or tumor recurrence after surgery may have affected the prognosis of pancreatic cancer patients [ 14 , 15 , 17 ]. Considering all of the above, we concluded that routine check-up helped detect the disease in patients at an earlier stage, but did not improve long-term survival.

Fig. 2. Kaplan-Meier survival curves by utility of routine check-up and undergoing radical surgery. A: Survival analysis of patients based on whether they detected pancreatic cancer by routine check-ups or not; B: survival analysis of patients received radical surgery based on whether they detected pancreatic cancer by routine check-ups or not;C: survival analysis of patients who did not received radical surgery based on whether they detected pancreatic cancer by routine check-ups or not; D: survival analysis of patients based on whether they had undergone radical surgery or not.
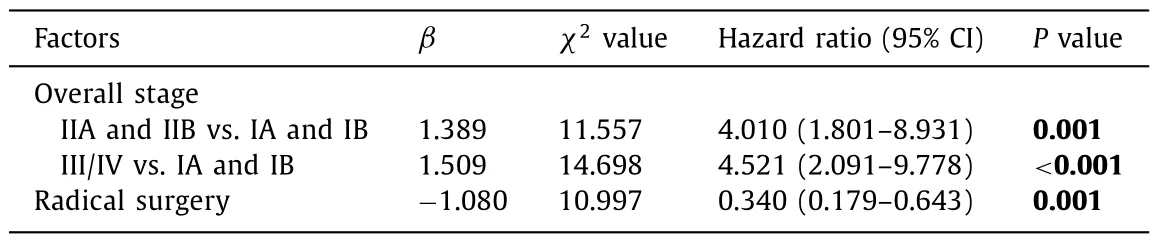
Table 3 Cox regression analysis of prognostic factors for pancreatic cancer.
A puzzling phenomenon was found in our study: radical surgery enhanced the overall survival time of patients with pancreatic cancer. However, when we divided all patients who underwent radical surgery into two groups according to whether they had routine check-up or not, we found no significant difference in the survival time between the two groups. We suspected that the psychological state of patients might have also had a great influence on the final prognosis. People who opted for regular routine check-up were more concerned about their health, and they were more likely to have anxiety or depression-related personality traits [18]. That means that if they obtained unfavorable test results from routine check-up, they had more psychological burden. A diagnosis of cancer always caused extensive emotional suffering for patients and challenged their psychological defenses. Most people experienced severe fear, anxiety, and depression during that period [ 18 , 19 ]. A previous study reported that participants in the pancreatic ductal adenocarcinoma surveillance program had high cancer worry scale (CWS) scores, and 13.3% of them did have cancerspecific worries with a CWS-score higher than 14, which was considered to be moderate to high cancer worries [20]. It was reported that prolonged perceived stress and worries were biologically detrimental [21]. Many studies have suggested that persistent psychological distress was associated with a substantially poor prognosis [22–24]. Thus, the psychological condition of pancreatic cancer patients is also a concern that needs to take care of. Therefore, a psychological intervention should be considered at the same time when the diagnosis is made [ 25 , 26 ].
Until now, there have been no consensus reached on a specific approach for pancreatic cancer screening because all presently available tests based on imaging and biomarkers seemed inadequate to detect cancer at early stage [27]. In China, the routine screening methods for pancreatic cancer are cancer biomarkers, ultrasonic imaging, and CT. Further testing, including MRI, positron emission tomography CT (PET-CT), or endoscopic ultrasound (EUS),is recommended when abnormalities are detected in the preliminary examination. CA19–9 is the only marker of efficacy evaluation approved by FAD in the United States by now, which is often used as a screening tool for pancreatic cancer detection. However, there are also problems associated with screening for pancreatic cancer with CA19–9 as a marker. For example, increased CA19–9 level can also be found in some benign diseases, such as pancreatitis, liver cirrhosis, acute cholecystitis, and other types of malignant tumors including gastric, uterine, and urothelial cancers [27]. It was reported that only 65% of patients with pancreatic cancer who were resectable, presented increased level of CA19–9 in the serum [28].These results suggested that CA19–9 had limited value in screening for pancreatic cancer. Previous studies have proven that EUS,MRI, or magnetic resonance cholangiopancreatography (MRCP) is more sensitive than CT, the first three of which are recommended screening methods [29–31]. EUS can detect small pancreatic lesions (<1 cm), and MRI or MRCP enables good visualization of the pancreatic duct, ductal dilation, and cyst formation [32]. However,regular health check-up in China do not include these screening programs, while routine ultrasound and CT included have difficulty in detecting small pancreatic lesions, which are not conducive to early detection of this disease. Hence, changes in the screening modalities in our country need to be considered.
It was reported that screening of individuals at high-risk for pancreatic cancer could detect early lesions [ 29–31 , 33 , 34 ]. In other countries, some specific screening programs have been put forward: patients with high-risk for pancreatic cancer should be enrolled in the testing procedures for clinical screening to follow the evolution of the disease in order to detect pancreatic cancer at an early stage [ 35 , 36 ]. However, screening/surveillance programs for pancreatic cancer are conducted mostly for high-risk individuals.In fact, population-based screening is not cost-effective due to the low incidence; therefore, screening in the general population was not commended [37]. Recent available screening methods for pancreatic cancer applied in general population might have a lower positive predictive value and a higher rate of false-positive results,which could cause overtreatment [38]. Considering the high costs of the routine check-up and the great psychological stress for the participants, a population-based screening for pancreatic cancer is not feasible [39]. As for high-risk individuals, although routine screening may help detect the disease early, its impact on survival remains unclear [ 31 , 33 ]. Some researchers compared among four strategies for managing first-degree relatives from familial pancreatic cancer kindred, and they found that the most effective strategy is to do nothing, which was the lowest costing and provided the greatest quality-adjusted remaining life years [40]. In addition,if routine screening does benefit the prognosis of high-risk population, the risk assessment methods and the definition including criteria for surveillance programs should be conducted [ 35 , 36 , 41 ].
Inevitably, there were some limitations in our study. Firstly, the sample size was not large enough, which may have caused the sampling bias. Secondly, the time of death might be not accurate for some patients since the information was received via telephone conversation with their family members. Finally, this was a single-center study. We plan to implement a multicenter prospective study with a larger sample size to further validate the conclusions of this study.
In conclusion, the role of routine check-up in the prognosis of patients with pancreatic cancer can be complex. Although routine check-up helps detect pancreatic cancer at early stage and the patients receive treatment earlier, it did not provide a significant long-term survival benefit.
Acknowledgments
We thank Jiao-Jiao Yang (the First Affiliated Hospital, Zhejiang University School of Medicine) for providing assistance with language editing.
CRediT authorship contribution statement
Cong-Ying Song:Data curation, Formal analysis, Investigation,Methodology, Writing - original draft.Yan Shen:Formal analysis,Validation, Writing - review & editing.Yuan-Qiang Lu:Conceptualization, Funding acquisition, Methodology, Project administration,Supervision, Writing - review & editing.
Funding
The study was supported by grants from the National Natural Science Foundation of China (81272075 and 81801572), the Medical and Health Science Foundation of Zhejiang Province (2019327552),the Foundation of Key Research Project of Zhejiang Province for Traditional Chinese Medicine (2019ZZ014), and the Foundation of Key Discipline Construction of Zhejiang Province for Traditional Chinese Medicine (2017-XKA36).
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (No.2019639).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Liver transplantation and BCLC classification: Limitations impede optimum treatment
- Do the existing staging systems for primary liver cancer apply to combined hepatocellular carcinoma-intrahepatic cholangiocarcinoma?
- Overlap of concurrent extrahepatic autoimmune diseases is associated with milder disease severity of newly diagnosed autoimmune hepatitis
- Aggressive surgical approach in patients with adrenal-only metastases from hepatocellular carcinoma enables higher survival rates than standard systemic therapy
- Integrating transcriptomes and somatic mutations to identify RNA methylation regulators as a prognostic marker in hepatocellular carcinoma
- The utility of two-dimensional shear wave elastography and texture analysis for monitoring liver fibrosis in rat model