Primary lymphomas of the genitourinary tract: A population-based study
2021-01-11CrlottPlumoElioMzzoneFrncescoMistrettSophieKnipperZheTinPulPerrotteFrncescoMontorsiShhrokhShritFredSdCludioSimeoneAlertoBrintiAlessndroAntonelliPierreKrkiewicz
Crlott Plumo , Elio Mzzone ,Frncesco A. Mistrett , Sophie Knipper , Zhe Tin ,Pul Perrotte , Frncesco Montorsi ,Shhrokh F. Shrit , Fred Sd ,, Cludio Simeone ,Alerto Brinti , Alessndro Antonelli ,*,Pierre I. Krkiewicz ,
a Cancer Prognostics and Health Outcomes Unit, University of Montreal Health Center, Montreal,Quebec, Canada
b Urology Unit, ASST Spedali Civili of Brescia, Department of Medical and Surgical Specialties,Radiological Science and Public Health, University of Brescia, Brescia, Italy
c Division of Experimental Oncology, Unit of Urology, Urological Research Institute (URI), IRCCS San Raffaele Scientific Institute, Milan, Italy
d Vita-Salute San Raffaele University, Milan, Italy
e Department of Urology, European Institute of Oncology, Milan, Italy
f Martini Klinik, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
g Division of Urology, University of Montreal Hospital Center (CHUM), Montreal, Quebec, Canada
h Department of Urology,Comprehensive Cancer Center,Medical University of Vienna,Vienna,Austria
i Department of Urology, Weill Cornell Medical College, New York, NY, USA
j Department of Urology, University of Texas Southwestern, Dallas, TX, USA
k Department of Urology, Second Faculty of Medicine, Charles University, Prag, Czech Republic
l Institute for Urology and Reproductive Health, I.M. Sechenov First Moscow State Medical University,Moscow, Russia
KEYWORDS Bladder lymphoma;Genitourinary neoplasm;Genitourinary;Primary extranodal lymphoma;Prostate lymphoma;Renal lymphoma;Testis lymphoma;Survival
Abstract Objective: We performed a population-based analysis focusing on primary extranodal lymphoma of either testis, kidney, bladder or prostate (PGUL). Methods: We identified all cases of localized testis, renal, bladder and prostate primary lymphomas (PL) versus primary testis, kidney, bladder and prostate cancers within the Surveillance, Epidemiology, and End Results database (1998-2015). Estimated annual proportion change methodology (EAPC), multivariable logistic regression models, cumulative incidence plots and multivariable competing risks regression models were used. Results: The rates of testis-PL,renal-PL,bladder-PL and prostate-PL were 3.04%,0.22%,0.18%and 0.01%,respectively.Patients with PGUL were older and more frequently Caucasian.Annual rates significantly decreased for renal-PL (EAPC: -5.6%; p=0.004) and prostate-PL (EAPC:-3.6%; p=0.03). In multivariable logistic regression models, older ager independently predicted testis-PL (odds ratio [OR]: 16.4; p<0.001) and renal-PL (OR: 3.5; p<0.001), while female gender independently predicted bladder-PL (OR: 5.5; p<0.001). In surgically treated patients, cumulative incidence plots showed significantly higher 10-year cancer-specific mortality(CSM)rates for testis-PL,renal-PL and prostate-PL versus their primary genitourinary tumors. In multivariable competing risks regression models, only testis-PL (hazard ratio [HR]:16.7; p<0.001) and renal-PL (HR: 2.52; p<0.001) independently predicted higher CSM rates.
Conclusion: PGUL rates are extremely low and on the decrease in kidney and prostate but stable in testis and bladder. Relative to primary genitourinary tumors, PGUL are associated with worse CSM for testis-PL and renal-PL but not for bladder-PL and prostate-PL,even after adjustment for other-cause mortality.
1. Introduction
Non-Hodgkin lymphomas (NHLs) account for about 90% of all lymphomas and they hold the seven highest incidence rank. Men and elderly (>65 years) are predominantly affected [1]. Approximately one-third of NHLs arise from sites other than lymph nodes, spleen or the bone marrow.Primary extranodal lymphomas are defined as lymphomas with no or only minor nodal involvement associated with a clinically dominant extranodal component. They can virtually originate in almost every organ [2].
The origin of primary extranodal lymphoma within the genitourinary (GU, PGUL) tract is extremely rare. Of all PGUL, testicular primary lymphoma (testis-PL) is the most common type [3]. Conversely, those originating from the kidney (renal-PL), the bladder (bladder-PL) and the prostate (prostate-PL) cumulatively account for less than 0.5%of all tumors affecting these three organs[4].To date,only one population-based study comprehensively focused on the PGUL [5]. However, the study did not include testis-PL and prostate-PL. One study examined testis-PL within a population-based database [6], while only case reports are available on prostate-PL [7].
Despite the availability of these studies, no direct comparisons can be made between PGUL and primary GU tumors. Moreover, all the previous studies considered both localized and systemic disease, making difficult to assess whether the extranodal involvement of the GU tract was indeed primary or just secondary. However, at least occasionally patients are surgically treated for a primary GU tumor but eventually are found to harbor PGUL. From this perspective, the lack of direct comparison represents an unmet need. Therefore, we investigated rates, temporal trends, demographics and survival outcomes of patients with primary lymphoma of testis, kidney, bladder or prostate relative their counterparts of primary GU, within the Surveillance, Epidemiology, and End Results (SEER) database from 1998 to 2015.
2. Methods
2.1. Data source and patient selection
Within the SEER database (1998-2015) [8], we focused on patients aged 18 years or older, diagnosed with histologically confirmed malignancy of the genitourinary tract (International Classification of Disease for Oncology [ICD-O]site codes C62.1/C62.9,C.64.9,C67.0/C67.9 and C61.9,for testis,kidney,bladder and prostate,respectively).We also relied on the International Classification of Diseases ninth edition codes to identify NHL[9],tumor of the testis(GCTT,both seminomatous [SGCT] and non seminomatous[NSGCT]), renal cell carcinoma (RCC), transitional cell carcinoma of the bladder(TCC)and adenocarcinoma of the prostate (PCa) cases [10]. Lymphomas were classified as either low or high grade, based on World Health Organization classification system [11]. All autopsy or death certificate cases were excluded. In order to identify only PGUL and therefore exclude secondary extranodal involvement,we included only patients with localized disease (SEER stage code). Consequently, all patients with either clinical or pathological lymph-node involvement, as well as those with metastatic disease, were excluded. Covariates included age at diagnosis,gender,race,marital status,year of diagnosis, residence area, socioeconomic status and surgical treatment.
2.2. Statistical analysis
Statistical analyses consisted of four analytical steps and applied to all four groups. First, rates of PGUL were estimated. Second, we examined the estimated annual percentage changes (EAPCs) of surgically-treated testis-PL,renal-PL, bladder-PL and prostate-PL. The EAPC is calculated using a generalized linear model under the assumption of linearity on the log scale, which is equivalent to a constant change assumption [12]. Third, multivariable logistic regression models predicting the risk of diagnosis of PGUL were fitted. Co-variates consisted of age, gender,marital status, race and year of diagnosis. Fourth, cumulative incidence plots depicted the cancer-specific mortality(CSM)and other-cause mortality(OCM)rates in testis-PL vs.GCT,renal-PL vs.RCC,bladder-PL vs.TCC and prostate-PL vs.PCa.Finally,multivariable competing risks regression(CRR)models were tested for CSM after adjustment for OCM in all the four groups. Adjustment variables consisted of histological type, age, gender, race and year of diagnosis.
All statistical tests were two-sided with a level of significance set at p <0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 3.4.1; http://www.r-project.org/).
3. Results
3.1. General characteristics and temporal trends
The rate of PGUL was 3.04% (470 out of 15 452 cases) for testis-PL, 0.22% (249 out of 111 955) for renal-PL, 0.18%(169 out of 93 780) for bladder-PL and 0.01% (83 out of 721 734) for prostate-PL. Table 1 summarizes the descriptive characteristics of PGUL versus primary GU malignancies according to sites of origin. Specifically, PGUL patients exhibited significantly higher age at presentation relative to GCTT, TCC and PCa patients (all p<0.01).Conversely, renal-PL patients exhibited significant lower age at presentation relative to RCC patients (p<0.001).Additionally, the proportion of female was significantly higher in bladder-PL patients, relative to TCC (64.5 vs.23.5%, p<0.001).Surgery was performed in 97.4% of testis-PL (100% orchiectomy), in 38.6% of renal-PL (64.2% partial and 36.8% radical nephrectomy), in 68.8% of bladder-PL(98.3% transurethral resection and 1.7% radical cystectomy) and in 55.4% of prostate-PL (97.9% transurethral resection of the prostate and 2.1% radical prostatectomy).
The most common histological subtype of primary extranodal lymphoma was diffuse large B-cell lymphoma(DLBCL), followed by mantle cell lymphoma. Testis-PL,renal-PL and bladder-PL were more often high grade(86.4%, 48.2% and 43.2%, respectively). Conversely,prostate-PL mostly showed low grade (45.8%) (Table 2).
No changes in EAPC were recoded for testis-PL (EAPC:-1.6%; p=0.06) and bladder-PL (EAPC: -3.6%; p=0.12).Conversely, renal-PL and prostate-PL EAPC showed a significant decrease over time (EAPC: -5.6%; p=0.004 and EAPC: -3.6%; p=0.03, respectively).
3.2. Multivariable logistic regression models predicting primary lymphoma
In multivariable logistic regression analyses (Table 3), independent predictors of higher testis-PL were older age(odds ratio [OR]: 16.4; p<0.001), African-American (OR:3.1;p<0.001)and other race(OR:2.4;p<0.001)relative to Caucasian, while of lower rates were more contemporary years(OR:0.6;p<0.001)relative to 1998-2003 period,and never married status(OR:0.7;p=0.02),relative to married status. Independent predictors of higher renal-PL were older age(OR:3.5;p<0.001),other race(OR:1.6;p=0.03)relative to Caucasian and never married (OR: 1.7; p=0.03)relative to married status.Independent predictors of higher bladder-PL were female(OR:5.5;p<0.001)relative to male gender and other race (OR: 2.1; p=0.005) relative to Caucasian, while of lower rates was older age (OR: 0.6;p=0.04). Independent predictor of higher prostate-PL rates was other race (OR: 2.6; p=0.002) relative to Caucasian,while of lower rates was age(OR:0.4;p=0.04).
3.3. Survival analyses
At cumulative incidence plots (Fig. 1), 10-year CSM rates were 28.3%vs.0.9%for testis-PL vs.GCTT(p<0.001),15.3%vs.8.3%for renal-PL vs.RCC(p=0.009),23.2%vs.23.0%for bladder-PL vs. TCC (p=0.37) and 35.6% vs. 2.5% for prostate-PL vs. PCa (p<0.001).
In separate multivariable competing risks regression models predicting CSM after adjusting for OCM (Table 4),testis-PL (hazard ratio [HR]: 17.3; p<0.001) and prostate-PL (HR: 6.3; p<0.001) independently predicted higher CSM relative to their primary GU tumor. Conversely, renal-PL and bladder-PL did not predict different CSM than their primary GU tumors.
4. Discussion
Approximately one-third of NHL arise from sites other than lymph nodes,spleen or the bone marrow[2].However,only a small proportion of primary extranodal lymphoma affects in the GU tract and may be incidentally diagnosed after surgery for a suspected primary GU tumor.We analyzed the SEER database to assess rates and variability over time as well as survival outcomes of patients with localized PGUL,relative to their primary GU tumor.Our analyses resulted in several noteworthy findings.
First, we confirmed that localized PGUL are extremely rare entities,involving 3.04%,0.22%,0.18%and 0.01%of all localized neoplasms of testis,kidney,bladder and prostate,respectively. In consequence a primary lymphoma within kidney,bladder and prostate will be encountered in one out of 10 000 patients.This rate is substantially higher in testis-PL, nonetheless only one in 33 such patients will harbor primary lymphoma among testis patients. This rates are slightly inferior to those previously reported by Lontos et al. [5] that considered all stages. Advanced age represented the most important indicator of PGUL in both testis-PL and renal-PL, while female gender was the most important indicator of PGUL in bladder-PL. Although a female predominance was also previously recorded [13], due to rarity as well as absence of pathognomonic features of renal-PL, bladder-PL and prostate-PL the discrimination between primary lymphoma versus primary GU origin is virtually impossible. Conversely, more advanced age in addition to characteristics that could not be examined within the current study, such as appearance on imaging and absence of tumor markers elevation, may help clinicians to distinguish between testis-PL and primary germ cell tumor.

Table 1 Descriptive characteristics of primary lymphoma versus genitourinary malignancies according to sites of origin: Identified within the Surveillance, Epidemiology and End Results database from 1998 to 2015.Testicular tumors (n=
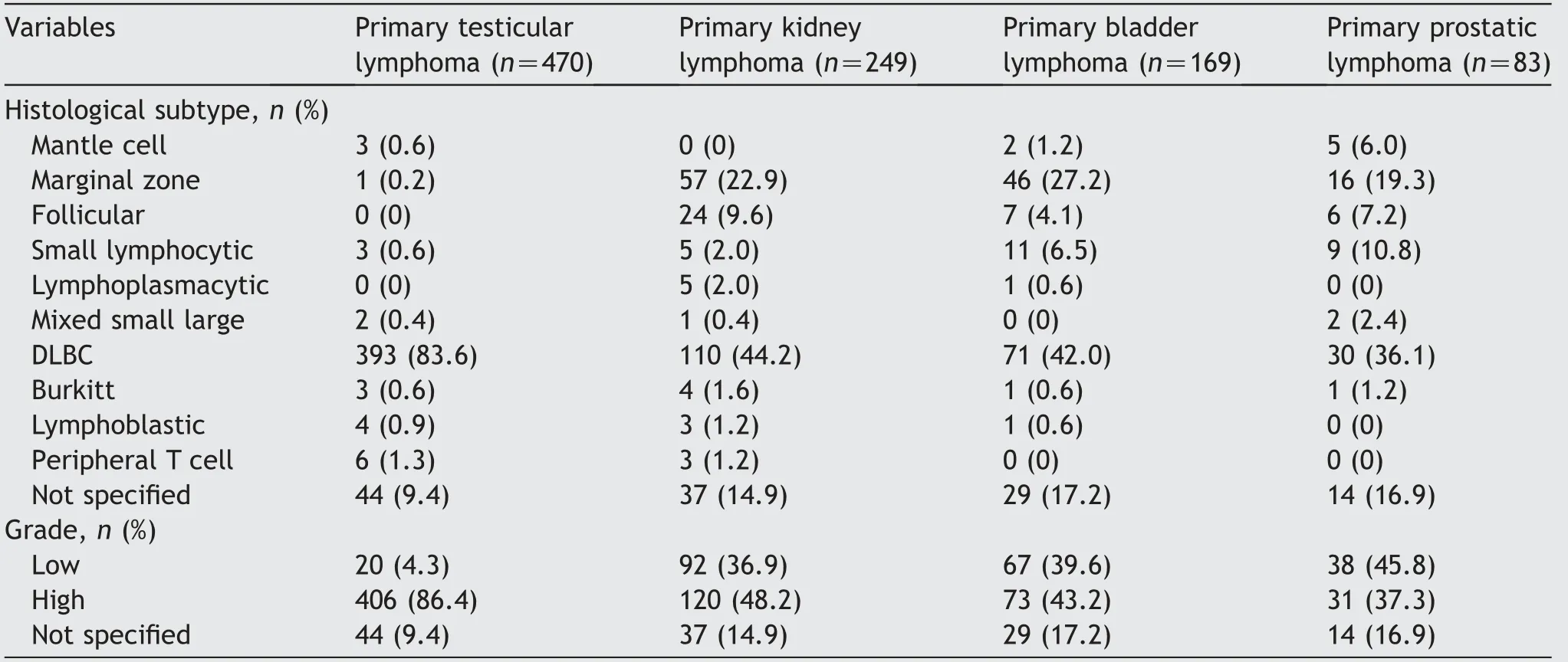
Table 2 Descriptive characteristics of patients diagnosed with primary testicular lymphoma, primary renal lymphoma, primary bladder lymphoma or primary prostate lymphoma, identified within the Surveillance, Epidemiology and End Results database from 1998 to 2015.
Second, our analysis of PGUL according to histological subtype showed variability according to the organ of origin(testis, kidney, bladder or prostate). However, DLBCL was the more frequent histological subtype, followed by marginal zone lymphomas and follicular lymphomas. These distribution patterns are in agreement with more historic reports from the SEER database where diagnosis were made from 1978 to 1995, where the rate of DLBCL was about 40% [14,15].
Third, among surgically treated patients, annual trend rates significantly decreased for both renal-PL and prostate-PL (EAPC: -5.6%; p=0.004 and EAPC: -3.6%;p=0.03, respectively), while no significant differences were identified for both testis-PL and bladder-PL.Recently,imaging criteria pertaining to ultrasound and computedtomography were proposed to distinguish betweenprimary lymphomas and other tumor origins [16,17]. These criteria may have resulted in recommendation for renal biopsy in case of suspected renal-PL instead of upfront surgery. Regarding testis-PL, orchiectomy may still be required, even when testis-PL is clinically suspected with the intent of eradicating a potential chemotherapy sanctuary site due to the presence of the blood-testis barrier [18]. Regarding bladder-PL and prostate-PL,clinical presentation may include gross hematuria and/or other urinary symptoms. In virtually all instance, transurethral resection is necessary for diagnostic purpose.
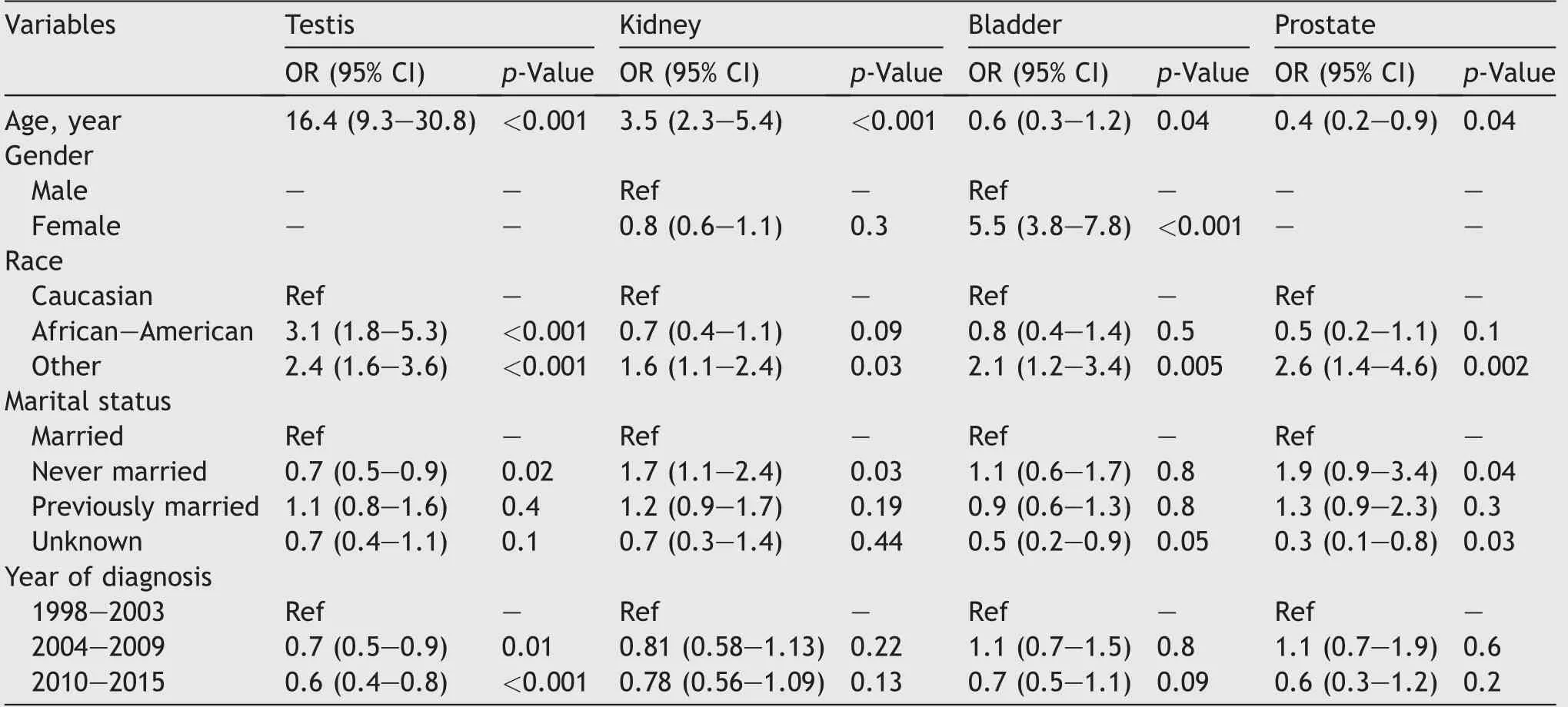
Table 3 Multivariable logistic regression analyses predicting localized primary extranodal lymphoma of either testis(n=470),kidney (n=249), bladder (n=169) or prostate (n=83), identified within the Surveillance, Epidemiology, and End Results database from 1998 to 2015.
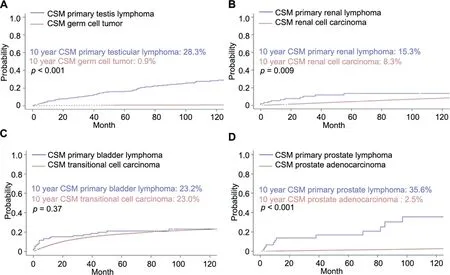
Figure 1 Cumulative incidence plots depicting cancer specific mortality (CSM) adjusted for other cause mortality (OCM) in (A)primary testicular lymphoma vs. germ cell tumor, (B) renal cell carcinoma vs. primary renal lymphoma, (C) transitional cell carcinoma of the bladder vs. primary bladder lymphoma and (D) prostate adenocarcinoma vs. primary prostatic lymphoma.
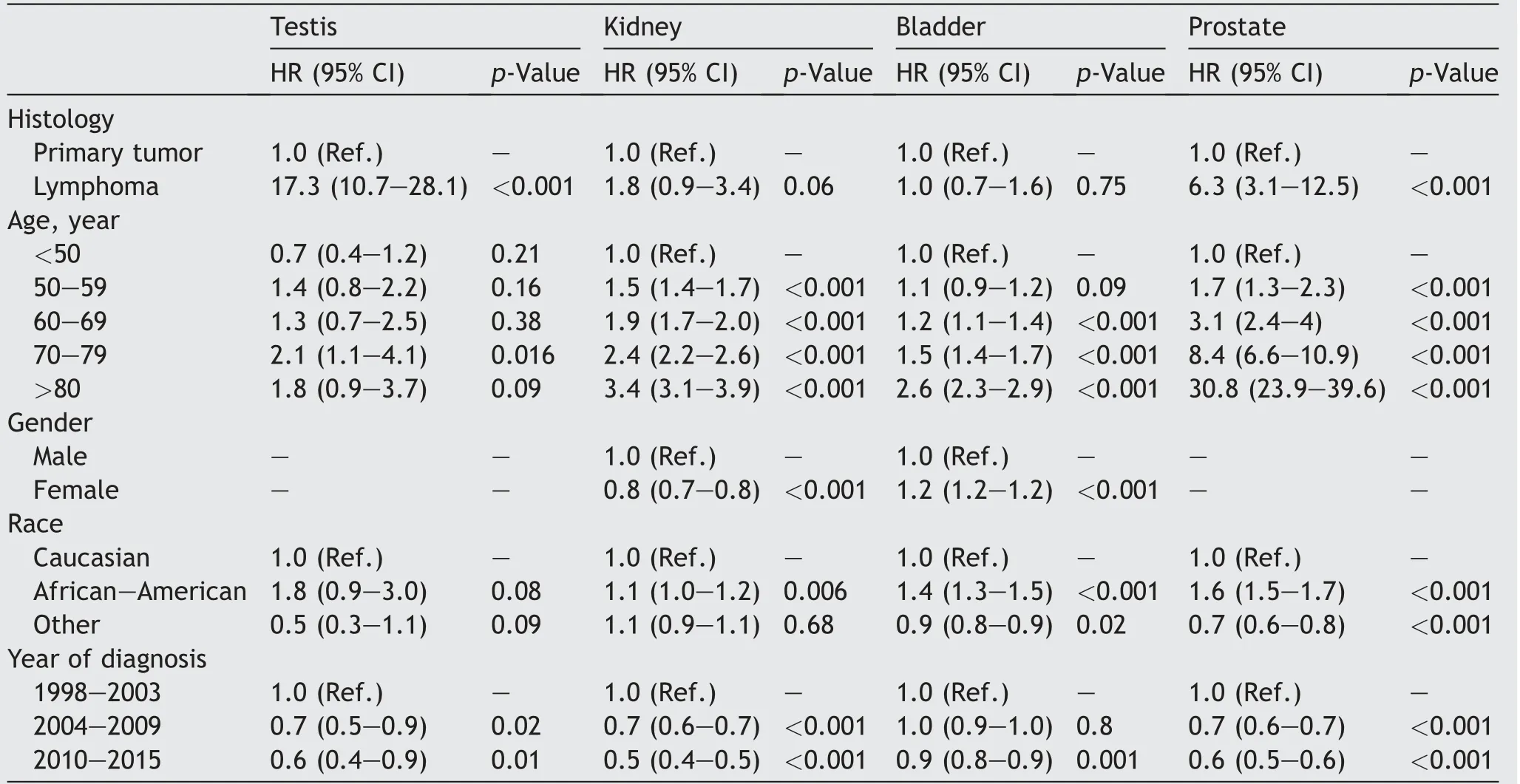
Table 4 Multivariable competing risks regression models predicting cancer-specific mortality according to presence or absence of lymphoma in testis, kidney, bladder and prostate cancer patients. All models are also adjusted for other-cause mortality.
Fourth, unlike any previous study, we tested CSM rates after adjustment for OCM, since OCM may have an important effect on CSM in all four examined GU organs with the exception of testis. Ten-year CSM rates were significantly higher for testis-PL, renal-PL and prostate-PL than for primary GU tumors, while no CSM differences were recorded for bladder-PL vs. TCC. However, in multivariable competing risks analyses, the survival disadvantage was only confirmed for testis-PL (HR: 17.3; p<0.001) and prostate-PL (HR: 6.3; p<0.001). These findings confirm the higher aggressiveness of PGUL in testicular and prostatic locations, even when diagnosed at localized stage. However, these differences may be also attributable to the good prognosis of localized GCTT and PCa. To the best of our knowledge, we are the first to perform a formal comparison between primary lymphoma and primary GU tumor origin within testis, kidney, bladder and prostate. Moreover, we also adjusted for OCM, which is particularly important in renal-PL, bladder-PL and prostate-PL since they affect elderly patients who are at a significant higher risk of OCM.
Despite its strengths,significant limitations of this study need to be acknowledged. First, this study represents a retrospective analysis with high potential for selection biases. Second, the definition of primary extranodal lymphoma relied only on stage summary “localized” provided by SEER database, with possible inclusion of secondary extranodal involvement. Third, no standardized specimen handling,as well as no central review regarding histological subtype, was applied within the SEER database. Fourth, no propensity score adjustment was performed while comparing survival outcomes. To address this, the survival analyses were performed only in surgically treated subgroup. Moreover, data regarding earlier cancer control endpoints, such as progression-free survival, are unavailable in the SEER database and these represent additional weaknesses. Finally, types and timing of administered chemotherapy, as well as other systemic therapies, could not be assessed in the SEER database. This limitation may have led to selection biases and may limit the generalizability of our findings.
Conclusion
PGUL rates are extremely low and on the decrease in kidney and prostate but stable in testis and bladder. Relative to primary genitourinary tumors, PGUL are associated with worse CSM for testis-PL and renal-PL but not for bladder-PL and prostate-PL, even after adjustment for other-cause mortality.
Author contributions
Study concept and design:Carlotta Palumbo, Pierre I.Karakiewicz.
Data acquisition:Carlotta Palumbo, Elio Mazzone, Francesco A. Mistretta, Sophie Knipper.
Data analysis:Carlotta Palumbo, Elio Mazzone, Francesco A. Mistretta, Sophie Knipper, Zhe Tian, Pierre I.Karakiewicz.
Statistical analysis:Carlotta Palumbo, Zhe Tian
Drafting of manuscript:Carlotta Palumbo, Pierre I.Karakiewicz.
Critical revision of the manuscript:Paul Perrotte, Francesco Montorsi, Shahrokh F. Shariat, Fred Saad, Claudio Simeone, Alberto Briganti, Alessandro Antonelli.
Conflicts of interest
The authors declare no conflict of interest.
杂志排行
Asian Journal of Urology的其它文章
- Xanthogranulomatous prostatitis:Impressive MRI appearance of a rare entity
- Giant pyogenic granuloma on the glans penis
- Huge urinoma caused by spontaneous ureteral rupture secondary to ureteral obstruction due to prostate cancer
- Cystoscopic extraction of an inadvertently placed ureteral stent in inferior vena cava
- Ambiguous clear cell carcinoma in medullary sponge kidney: A case report
- Investigation of confocal microscopy for differentiation of renal cell carcinoma versus benign tissue. Can an optical biopsy be performed?