Xanthogranulomatous prostatitis:Impressive MRI appearance of a rare entity
2020-12-28SmpiMehtSpyridonKmpntisKonrdWolfeSidthLiynge
Smpi Meht , Spyridon Kmpntis ,*, Konrd Wolfe ,Sidth H. Liynge
a Department of Urology, Southend University Hospital, Southend on Sea, Essex, UK
b Department of Histopathology, Southend University Hospital, Southend on Sea, Essex, UK
c Department of Radiology, Southend University Hospital, Southend on Sea, Essex, UK
A 60-year-old man, with a background history of insulin dependent diabetes, after a treated Escherichia coli urinary tract infection (Amoxicillin-Clavulanic acid for 10 days), experienced symptom recurrence. His main symptoms included feeling unwell, burning in urination and pelvic pain. A digital rectal examination revealed a tender swelling in the pelvic area. His prostate-specific antigen(PSA)was 0.8 ng/mL,while the 2-glass Meares-Stamey test was negative. A magnetic resonance imaging (MRI) of his pelvis identified a large unusual appearing mass replacing both the prostate and seminal vesicles (Fig. 1). Rest of the imaging (computed tomography of chest, abdomen, pelvis and bone scan)showed a few small volume pelvic side-wall lymph nodes and no evidence of lung or other distant metastases. Given the imaging appearances, a prostatic sarcoma, such as a leiomyosarcoma, was felt to be more likely than a prostate adenocarcinoma. The mass was biopsied treansrectally with the histology showing xanthogranulomatous prostatitis (Supplementary Fig. 1). Repeat MRI performed 10 months later following antibiotic treatment(Ciprofloxacin for 6 weeks) showed dramatic resolution of the mass with almost normal appearance of the prostate gland (Fig. 2).
Xanthogranulomatous prostatitis is a rare form of nonspecific granulomatous prostatitis that can simulate prostate cancer [1]. As it is difficult to suspect in clinical settings, a histopathological diagnosis is almost always essential [2]. Conservative treatment should be considered in principle, with antibiotics to be the first choice [1].
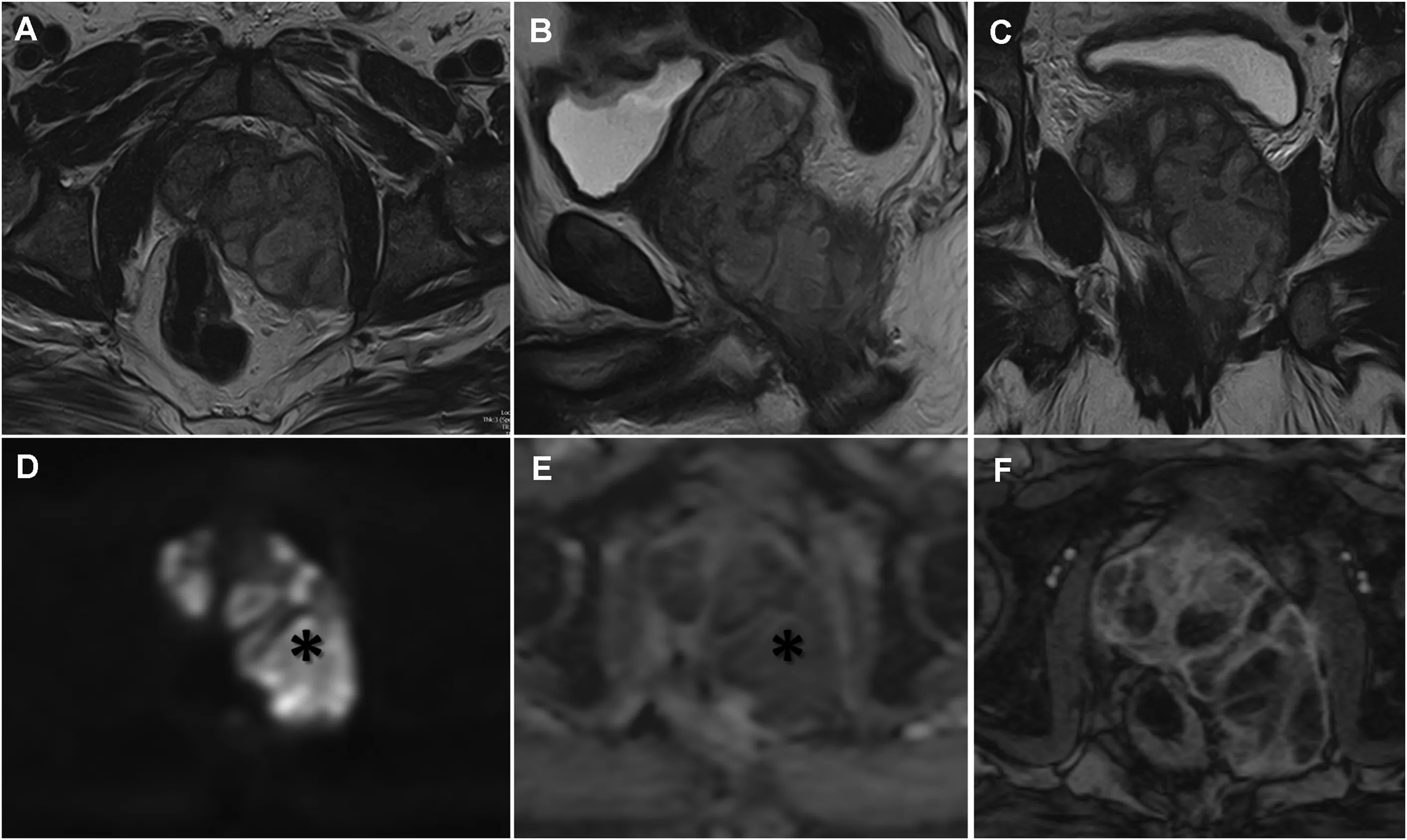
Figure 1 Axial (A), sagittal (B) and coronal (C) T2-weighted images (MRI 1.5 T machine with 8-channel phased array body coil,Signa Excite,GE Healthcare,Little Chalfont,UK)show a large lobulated multi-septate mass of intermediate signal intensity which is replacing the prostate and extending into the peri-prostatic space.The extra-prostatic component abuts the lavator ani muscle and extends into the mesorectal fat displacing both the prostate gland and anorectal junction to the right. The mass has a T2-hypointense rim or pseudocapsule. On the axial diffusion-weighted MRI (D) and ADC map (E) the mass shows marked restricted diffusion (asterisk). (F) Axial DEC MR image shows early and heterogeneous enhancement of the septations and wall of the mass.Multiple non-enhancing areas are seen, interpreted as cystic necrosis. MRI, magnetic resonance imaging; ADC, apparent diffusion coefficient; DCE, dynamic contrast enhanced.
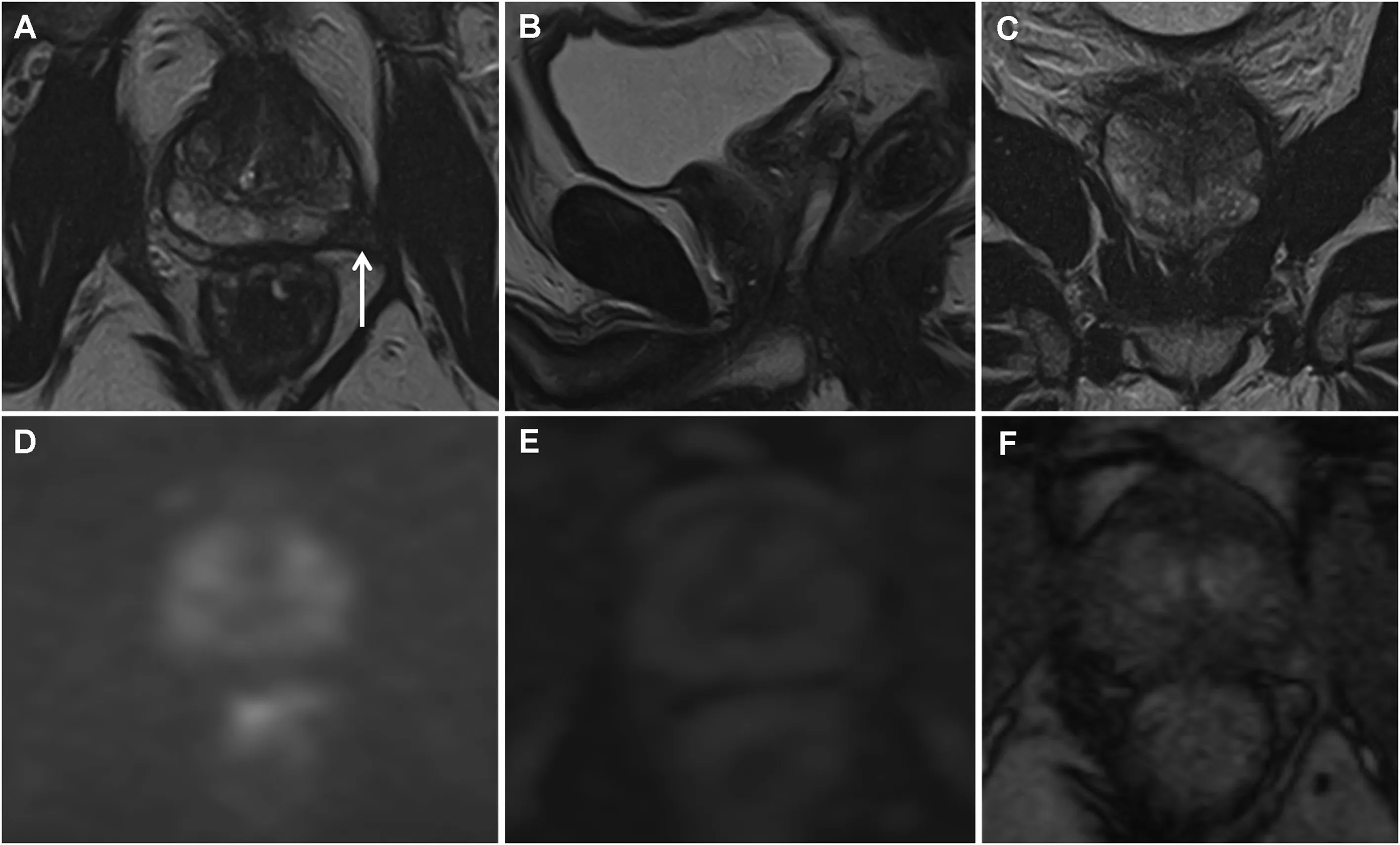
Figure 2 Repeat MRI performed 10-months later shows dramatic resolution of the previously noted intra- and extra-prostatic mass and reconstitution of the normal T2-weighted (A, B, C) zonal appearance to the prostate gland. There are no residual areas of restriction on the diffusion images and ADC map(D,E)and a normal enhancement pattern on the DCE images(F).The only sequelae from the prior infection is the low T2-weighted fibrosis/scarring in the peri-prostatic fat on the left (white arrow). MRI,magnetic resonance imaging; ADC, Apparent diffusion coefficient; DCE, dynamic contrast enhanced.
Author contributions
Study design:Sampi Mehta.
Data acquisition:Spyridon Kampantais,Sidath H.Liyanage,Konrad Wolfe.
Drafting of manuscript:Spyridon Kampantais, Sidath H.Liyanage.
Critical revision of the manuscript:Sampi Mehta,Sidath H.Liyanage.
Conflicts of interest
The authors declares no conflict of interest.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2019.10.010.
杂志排行
Asian Journal of Urology的其它文章
- Primary lymphomas of the genitourinary tract: A population-based study
- Giant pyogenic granuloma on the glans penis
- Huge urinoma caused by spontaneous ureteral rupture secondary to ureteral obstruction due to prostate cancer
- Cystoscopic extraction of an inadvertently placed ureteral stent in inferior vena cava
- Ambiguous clear cell carcinoma in medullary sponge kidney: A case report
- Investigation of confocal microscopy for differentiation of renal cell carcinoma versus benign tissue. Can an optical biopsy be performed?