Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
2020-09-21ToYuYnQiuYueJinChenHongBoRenRuiJiBoQunCheng
To Yu , Yn-Qiu Yue , Jin Chen , Hong-Bo Ren , Rui Ji , Bo-Qun Cheng , *
a Department of Gastroenterology, Qilu Hospital, School of Medicine, Shandong University, Jinan 250012, China
b Department of Gastroenterology, Binzhou People's Hospital, Binzhou 256610, China
TotheEditor:
Simplifying the endoscopic procedures and reducing the procedure time are necessary, while guaranteeing that the stone retrieval efficacy is an important prerequisite for minimizing the risk of complications after endoscopic retrograde cholangiopancreatography (ERCP).Compared with endoscopic sphincterotomy (EST),which can effectively extract common bile duct stones, endoscopic papillary balloon dilatation (EPBD) causes less bleeding and perforation and preserves the function of sphincter of Oddi [ 1 , 2 ].However, in comparison with EST, EPBD is related to a higher risk of pancreatitis [ 2 , 3 ].Retrieving large bile duct stones (≥10 mm) using the conventional techniques EST and EPBD is difficult.The use of EST combined with endoscopic papillary large balloon dilation(EPLBD) for bile duct stone removal was first introduced by Ersoz et al.[4], and this innovation has become useful in patients with large or difficult stones.In addition, removing the bile duct stones should be considered urgent.Especially, EPLBD procedure is appropriate for patients with unfavorable anatomy for EST, such as those who underwent Roux-en-Y or Billroth II gastrectomy [5].
Performing EST before EPLBD might decrease post-ERCP-related pancreatitis by guiding balloon dilation toward the bile duct instead of the pancreatic duct [2-4].Although some studies reported that EPLBD without EST was safe and effective in patients with large bile duct stones [4-6], the long-term outcomes of EPLBD alone are still controversial and poorly understood.To investigate the safety and efficacy of EPLBD alone in the treatment of large bile duct stones and to elucidate its long-term outcomes, we conducted a retrospective research to compare these two different therapeutic methods.
We reviewed 111 patients who underwent endoscopic biliary stone extraction in our department from January 2012 to December 2016.The inclusion criteria were as follows: (1) age ≥18 years old and (2) maximum stone size ≥10 mm.The exclusion criteria included (1) prior EST or EPBD, (2) bleeding diathesis, and (3)acute pancreatitis.All patients individually provided a written informed consent for the procedure, and this study was approved by the Ethics Committee of Qilu Hospital of Shandong University(2016063).The diameters of the balloons ranged from 12 to 16 mm, and the size of the balloon dilation was selected according to the diameters of the stones and bile duct proximal to the tapered segment under fluoroscopy.Bile duct stones were extracted with standard Dormia baskets or removal balloons.When the standard technique failed to retrieve the stones, a mechanical lithotripter was used to fragment the stones.Complete stone removal was confirmed by the nonexistence of any filling defect by balloon occlusion cholangiography.If the stones were not completely removed in the first session, another attempt at stone extraction was performed 3 days later.Post-ERCP pancreatitis, cholangitis, perforation, and bleeding were evaluated.Abdominal pain persisting for more than 24 h and a serum amylase level>3 times the reference value after the procedure were signs of bile duct obstruction.The occurrence of increased body temperature (>38 °C), abdominal pain, leukocytosis, and jaundice were signs of cholangitis.The presence of perforation was evaluated by persistent abdominal pain, increased body temperature, and peritoneal irritation sign and was confirmed by survey radiography or computed tomography (CT).Bleeding was defined as decreased hemoglobin level of at least 20 g/L from the baseline or requirement of blood transfusion after the procedure.All early complications were defined and classified according to the 1991 consensus guidelines [7].Stone recurrence, cholangitis, and cholecystitis were evaluated in the long-term follow-up (>30 days after EPLBD).Stone recurrence was diagnosed by abdominal ultrasound, CT, or magnetic resonance imaging.Right upward abdominal pain, increased body temperature, enlarged gallbladder, and thickened gallbladder wall indicated cholecystitis.
EPLBD with or without EST was performed in 20 and 91 patients, respectively.No significant differences were found between the two groups in terms of age, sex, number of stones, distal bile duct stricture, and maximum size of stones.EPLBD with or without EST was successfully performed in all patients, with an overall complete stone removal rate of 95.5% (106/111).No differences were observed in complete stone retrieval rate, first-session complete stone removal rate, and mechanical lithotripsy rate between the two groups (95.6%, 94.5%, and 13.2% in the EPLBD alonegroup; 95.0%, 95.0%, and 5.0% in the EST + EPLBD group, respectively) (Table 1).Early complications were observed in 1/20 patients (5.0%) in the EST + EPLBD group and 9/91 (9.9%) in the EPLBD alone group.Five patients (5.5%) developed pancreatitis in the EPLBD alone group, while none in the EST + EPLBD group.Cholangitis had developed in one patient (5.0%) in the EST + EPLBD group and three patients (3.3%) in the EPLBD alone group.Moreover, only one incidence of perforation (1.1%) was observed in the EPLBD alone group and none in the EST + EPLBD group.Meanwhile, no hemorrhage occurred in both groups.Overall, no statistically significant differences in the incidence of pancreatitis, cholangitis, perforation, and hemorrhage were observed between the EST + EPLBD and EPLBD alone groups (allP>0.05).Nineteen (17.1%) patients were lost to follow-up (2 in the EST + EPLBD group and 17 in the EPLBD alone group).Ultimately, 18 patients in the EST + EPLBD group and 74 patients in the EPLBD alone group were enrolled for the analysis of long-term outcomes.And the rates of stone recurrence, cholangitis, and cholecystitis did not differ significantly between the two groups (allP>0.05).To determine the potential risk factors of stone recurrence, we assessed the age, sex, number of stones (≥3/<3), maximum size of stones (≥15 mm/<15 mm),bile duct diameter (≥16 mm/<16 mm), mechanical lithotripsy,periampullary diverticulum, EST + EPLBD/EPLBD alone, and gallbladder status.However, no significant differences were found between the stone recurrence and no stone recurrence groups for any of these factors (allP>0.05) (Table 2).
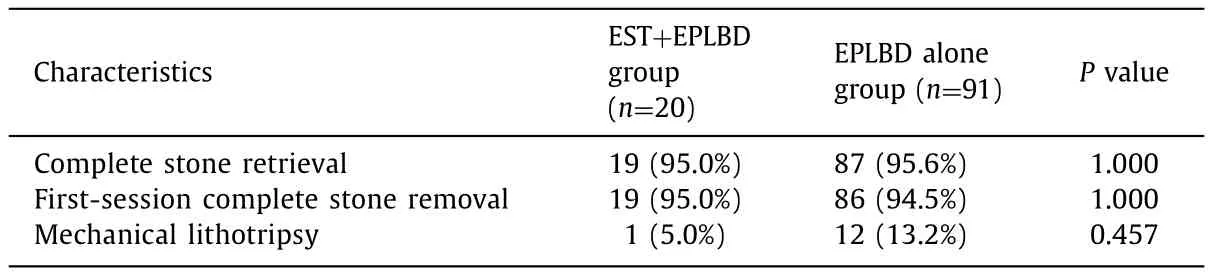
Table 1Results of stone retrieval after endoscopic papillary large balloon dilation.
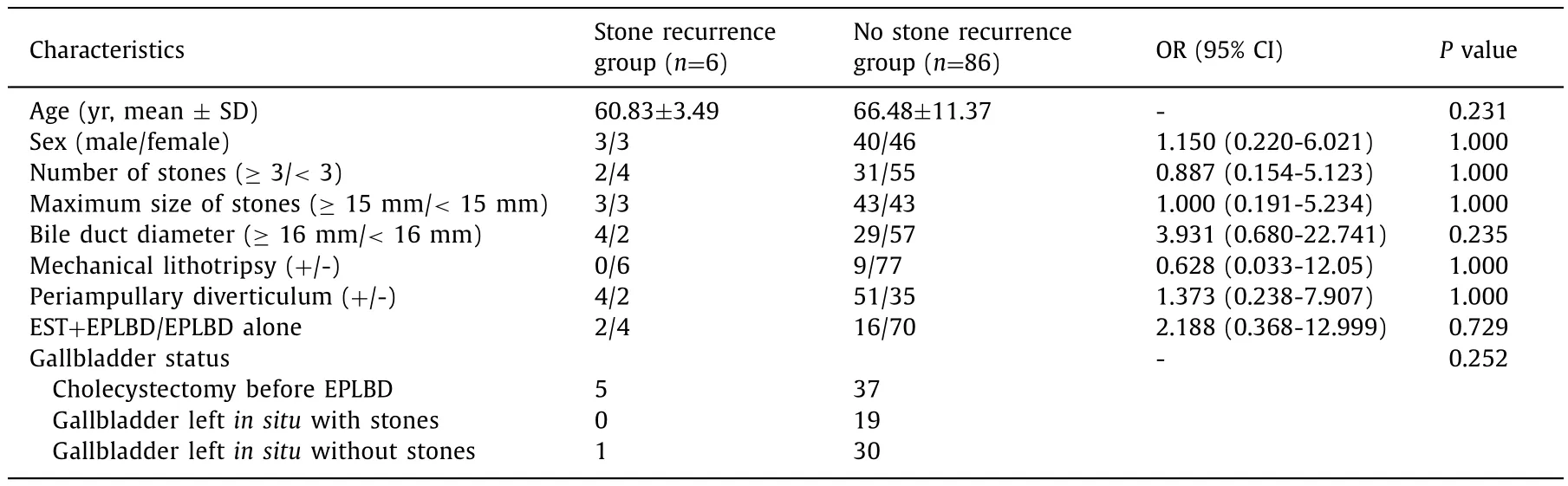
Table 2Risk factors for stone recurrence.
In the present study, the results on the efficacy of removing stones (≥10 mm) by EPLBD alone are satisfactory, with a complete stone extraction success rate of 95.6% (87/91).This success rate is comparable to that of 95.0% (19/20) in the EST + EPLBD group,conforming to the results in previous study [5].Therefore, EPLBD alone can provide adequate orifice dilation for a successful stone retrieval.
The incidence of pancreatitis in the EPLBD alone and EST + EPLBD groups was 5.5% (5/91) and 0% (0/20), respectively,with no significant difference (P= 0.583).Therefore, EPLBD itself does not increase pancreatitis incidence.A multicenter study emphasized that large-diameter balloons (≥14 mm) were independently correlate with low risks of pancreatitis, suggesting that direct physical compression by large-diameter balloons is not the main factor for the occurrence of pancreatitis after EPLBD [6].Perforation occurred in one patient in the EPLBD alone group, while none in the EST + EPLBD group.Fortunately, the patient was treated conservatively.A large-scale multicenter study reported that distal bile duct stricture is an independent factor of perforation [5].Therefore, despite the uncertain perforation site, we speculate that distal bile duct stricture was the cause of this complication.
Stone recurrence is the most common long-term complication after bile duct stone removal, and its pathogenesis may be closely related to bile stasis, duodenobiliary reflux, and biliary bacterial infection [8].Permanent loss of sphincter function after EST increases the likelihood of bacterial infection in the bile duct.Therefore, irreversible damage may occur to the sphincter function after EST.Compared with EST, conventional EPBD generates slight trauma to the papilla; thus, sphincter function is partially preserved [ 1 , 2 ].A histologic study conducted in animal models indicated that a balloon dilation diameter reaching 8 or 10 mm did not change the papillary structure, but if the dilation reached 12 mm or larger, the papillary structure was disrupted, resulting in sphincter function loss [9].Additionally, a persistent and comparable loss of sphincter function may occur in both EPLBD alone and EST + EPLBD groups after 1 year [10].Therefore, EPLBD may not be able to reserve the sphincter function, and its long-term outcome is comparable with that of EST.
In summary, EPLBD alone may be alternative therapy for patients with large bile duct stones compared with EPLBD + EST.However, our study was limited by its small sample size and retrospective nature.Therefore, further large-scale multicenter comparative studies are necessary to confirm the safety, efficacy, and long-term outcomes of EPLBD alone.
Acknowledgments
None.
CRediT authorship contribution statement
Tao Yu:Conceptualization, Supervision, Writing - review & editing.Yan-Qiu Yue:Data curation, Formal analysis, Writing - original draft.Jian Chen:Data curation, Investigation, Writing - originaldraft.Hong-Bo Ren:Data curation, Investigation, Writing - original draft.Rui Ji:Data curation, Investigation, Writing - original draft.Bao-Quan Cheng:Conceptualization, Methodology, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Qilu Hospital of Shandong University (2016063).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Two-in-one: A pooled analysis of primary hepatic neuroendocrine carcinoma combine d/collide d with hepatocellular carcinoma
- A ten-year experience of inferior vena cava reconstruction for malignancy: The importance of a multidisciplinary approach with hepatobiliary surgery
- New variation of median arcuate ligament compression causing hepatic arterial hypoperfusion during liver transplantation
- Echinococcus granulosus: A novel parenchymal sparing surgical treatment
- Serum chitinase-3-like protein 1 is a biomarker of liver fibrosis in patients with chronic hepatitis B in China
- Role of selected criteria and preventive chemotherapy in tumor recurrence after liver transplantation
