A ten-year experience of inferior vena cava reconstruction for malignancy: The importance of a multidisciplinary approach with hepatobiliary surgery
2020-09-21MriBimsGeorgeRynPickensJesseSulzerDionisiosVrochidesJohnMrtinieDvidLeviDvidInnitti
Mri R.Bims-George , Ryn C.Pickens , Jesse K.Sulzer , Dionisios Vrochides ,John B.Mrtinie , Dvid M.Levi , Dvid A.Innitti , *
a Division of Hepatopancreatobiliary Surgery, Department of Surgery, Carolinas Medical Center, 1025 Morehead Medical Drive, Suite 600, Charlotte, NC 28204, USA
b Division of Transplant Surgery, Department of Surgery, Carolinas Medical Center, Charlotte, NC, USA
TotheEditor,
Tumor invasion of the inferior vena cava (IVC) through direct erosion is a rare and poor prognostic feature of aggressive hepatic or perihepatic malignancies [1 , 2].Literature shows poor response to chemotherapy, such that resection often is the only option for improved survival [3].Multidisciplinary collaborations can expand technical options; incorporation of transplant techniques has led to successful R0 resection involving difficult vascular reconstruction and extended resection [4 , 5].This study describes and analyzes the ten-year collaborative experience of hepatobiliary (HPB) surgeons in management of malignancies involving the perihepatic IVC.
A retrospective review was performed of hepatobiliary malignancies with involvement of the perihepatic IVC from 2008 to 2018.Primary outcomes were early mortality and survival.Secondary perioperative outcomes included postoperative length of stay (LOS), major complications, readmission, and 90-day mortality.All patients considered for perihepatic IVC resection underwent pre-operative multidisciplinary evaluation and optimization.They were presented at multidisciplinary tumor board involving medical oncology, radio-oncology and surgical oncology.IVC resection is only offered for malignancies in which R0 resection was required for significant improvement in survival.
Vascular exclusion is guided by intraabdominal and transesophageal ultrasonography.If IVC clamping is not tolerated for infra-diaphragmatic tumors, venovenous bypass is employed with assistance from transplant surgery.For tumors extending to the right atrium, cardiopulmonary bypass is utilized with assistance from cardiothoracic surgery.
Tumor location and circumferential involvement dictates IVC resection approach.Invasion of up to 25% circumference allows for tangential resection with primary repair of venotomy.If thrombus is non-adherent, it can be extracted without resection followed by primary repair, even if tumor extends above hepatic veins.If tumor adheres or invades between 25% and 75% of circumference, partial resection can be employed but is location dependent.Further,the cavotomy for larger resections may require a bovine pericardial patch.Tumor that involves more than 75% of the circumference is managed with segmental resection.If no evidence of chronic infrarenal IVC occlusion, reconstruction is required to ensure adequate venous drainage and cardiac inflow.Primary circumferential repair is preferred if resection gap is small such that the caval ends can be approximated without tension.Most cases require synthetic polytetrafluoroethylene (PTFE) inter-positional graft.
For chronic occlusion of the infrarenal IVC with tumor and/or bland thrombus, reconstruction may not be required due to development of abdominopelvic collaterals through the azygoushemiazygous and portomesenteric systems.If no history of obstructive symptomology, the IVC can be sutured or staple ligated if hemodynamically stable during caval interruption, which will increase risk of recurrent venous thrombus, pulmonary embolism, or distal thrombus.
Retrohepatic IVC invasion requiringex-vivohepatic resection is offered to carefully selected patients with excellent pre-operative performance status.Hepatic explantation,enblocresection on the backtable, synthetic graft reconstruction of the IVC, and piggyback auto-transplantation are performed in an overlapping manner through collaboration with HPB and transplant surgeons.When necessary to achieve an adequate future liver remnant after hepatic resection, two-staged liver molding with techniques such as associating liver partition & portal vein ligation for staged hepatectomy(ALPPS) can be employed [6].
We identified 16 patients with perihepatic IVC tumor invasion or extension requiring liver resection and/or mobilization with caval repair or reconstruction.Disease included intrahepatic cholangiocarcinoma (n= 4), colorectal liver metastases (n= 2),hepatocellular carcinoma (n= 2), retroperitoneal sarcoma (n= 5),pancreatic adenocarcinoma (n= 1), gastrointestinal stromal hepatic metastases (n= 1), and neuroendocrine tumor hepatic metastases (n= 1).Age at time of surgery ranged from 33 to 76 years,with an average of 58 years.The majority were female (56%) andhad a body mass index ranging from 21.9 to 39.8 kg/m2.Operations included right hepatectomy (n= 5), left hepatectomy (n= 2),right trisectionectomy (n= 1),ex-vivohepatectomy (n= 3), pancreaticoduodenectomy (n= 1), anden-blocretroperitoneal mass excision (n= 4).Several representative intra-operative photos are shown in Figs.1-3.
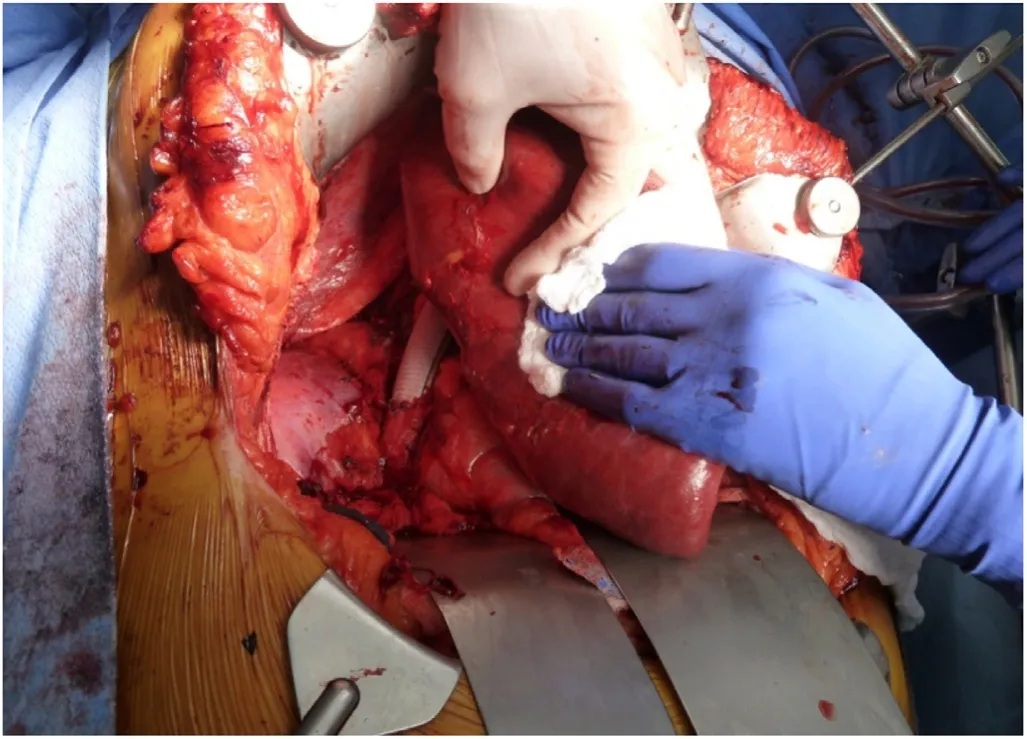
Fig.1.Intra-operative image of IVC replacement with a synthetic graft.IVC: inferior vena cava.
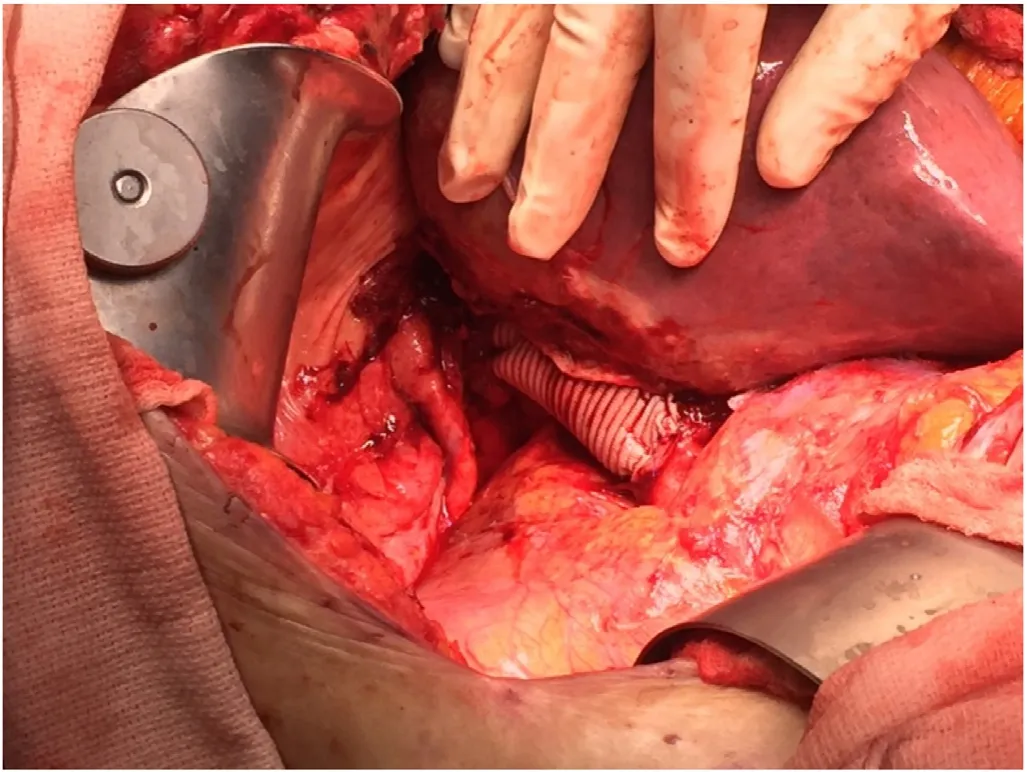
Fig.2.Vena caval reconstruction perfusing the re-implanted right lobe after an exvivo approach.
Three patients underwent anex-vivopartial hepatectomy with backtable IVC resection and interposition graft reconstruction followed by liver auto-transplantation, including one case as stage II of an ALPPS procedure (Table 1) [6].One patient underwent ligation of the infrarenal IVC without reconstruction.IVC repair with primary closure was the most common technique employed(n= 7; 54%).Reconstruction was equally divided between bovine pericardial patch (n= 3; 23%) and PTFE interposition graft (n= 2;15%).
For cases with a standard non-exvivoapproach, R0 resection was achieved in five of 13 resections with only two of the 8 positive margins on the IVC resection edge (Table 2).Post-operative LOS was 8 days (IQR 0-20 days).The 90-day readmission rate was 15% and 90-day major complication rate was 38%.There were no complications related to graft infections or IVC compression.The 90-day IVC patency rate was 100% for all three techniques.Early mortality at 30 and 90 days was 8% and 15%, respectively.There was one intraoperative death of a patient with cholangiocarcinoma who suffered acute cardiac dysfunction after coming offvenovenous bypass, resulting in outflow congestion and hemorrhage with uncorrectable coagulopathy.Median oncologic survival was found to be 44 months and survival at five years was 42.4%.
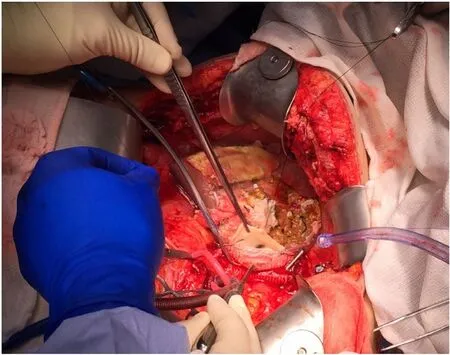
Fig.3.Hypertrophied liver remnant reimplanted; note the ice slush around the auto-graft; forcep marking the IVC patch with hepatic outflow being anastomosed to the retrohepatic IVC graft; cannulation of the portal vein for venovenous bypass pictured as well.IVC: inferior vena cava.
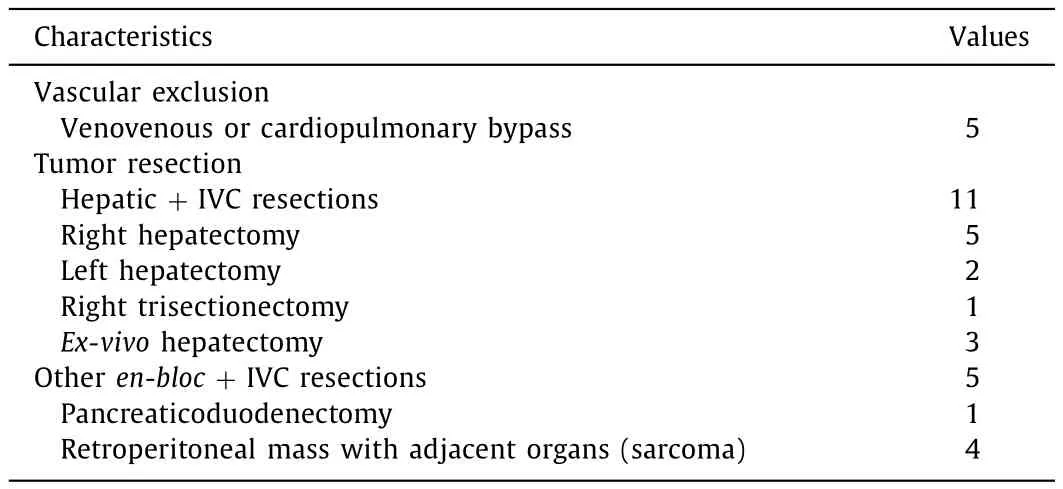
Table 1Surgical characteristics.
Of the three patients who underwentex-vivohepatectomy with IVC resection and interposition graft reconstruction, R0 resection was achieved in 100%, including oneex-vivoresection performed as phase II of ALPPS (Table 2).Post-operative LOS was 21 days (IQR 14-25 days).The 90-day readmission rate was 100% and 90-day major complication rate was 67%.There were no 90-day mortalities and no current evidence of recurrent or metastatic disease at 12-month follow-up.
Invasion of the perihepatic IVC confers poor prognosis by extravascular invasion from hepatic or perihepatic tumors.This 10-year experience describes the short- and long-term outcomes from collaboration of HPB surgeons for malignancies that require resection and/or mobilization, vascular exclusion, perihepatic caval resection, and reconstruction.Multidisciplinary collaboration offers an extension of techniques, providing opportunity for cure in otherwise conventionally unresectable populations.Despite an overall survival advantage, careful patient selection and thorough counseling is imperative given the high demonstrated perioperative risk.
We found 30-day mortality of 8% and 90-day mortality of 15%of our non-exvivocases which is comparable to the current literature demonstrating mortality rates ranging from 4% to 25% [2 , 7-9 ].One of the largest series of combined hepatic and IVC resections demonstrated 90-day mortality rate of 8% [8].Our median oncologic survival was found to be 44 months with a five-year survival of 42.4%.These results are comparable to published survival rates of 79%-89% at one year for IVC-invading hepatic malignancies, with only 31%-35% alive at five years [8 , 10].
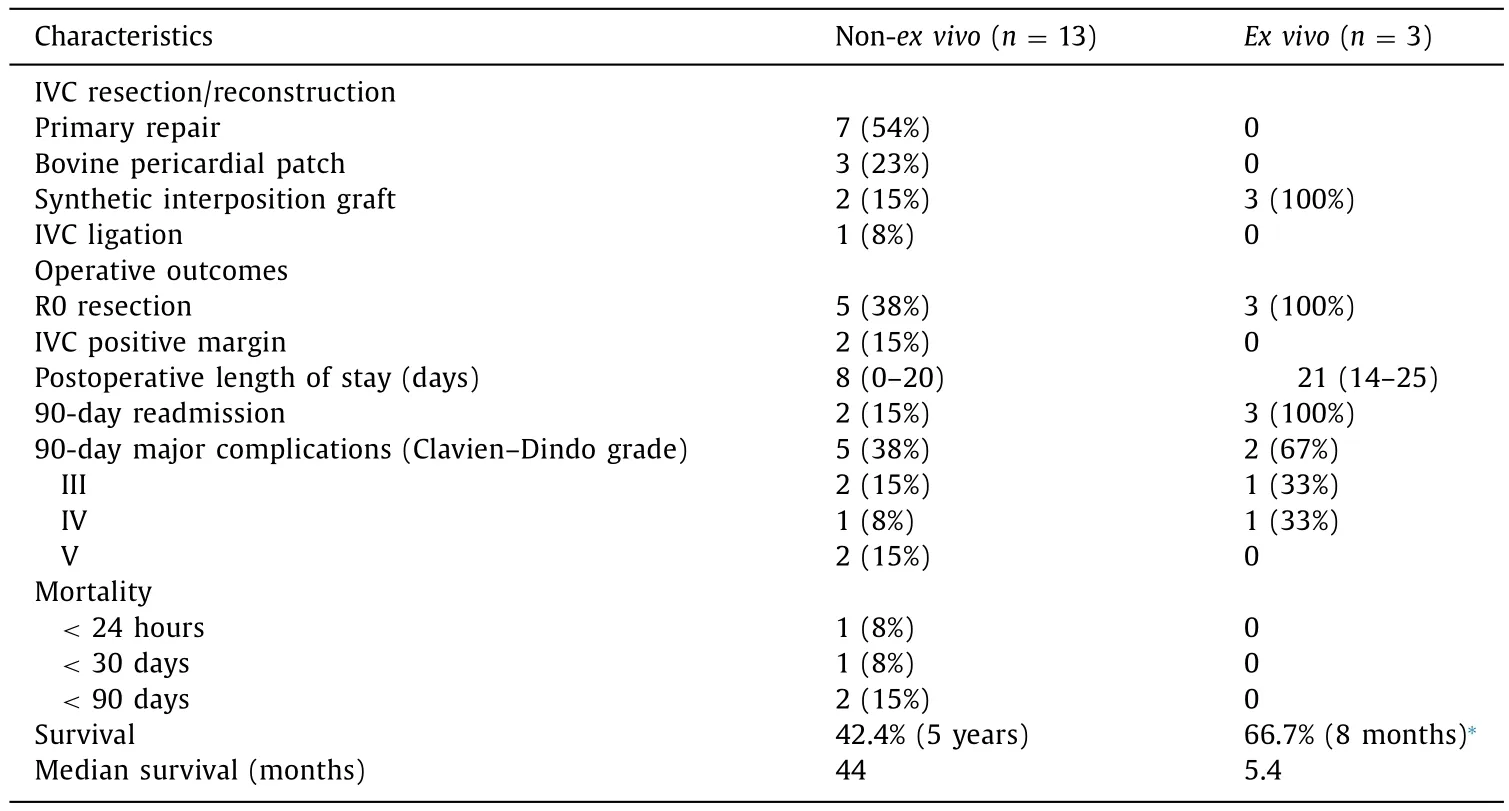
Table 2Surgical and oncologic outcomes.
In conclusion, resection of tumors involving the perihepatic IVC with or without various techniques for caval reconstruction infers high morbidity and mortality yet provides the only opportunity for R0 resection in some locally-advanced abdominal malignancies.Regardless of etiology, it is integral to collaborate with appropriate surgical teams such as HPB, transplant or cardiothoracic to expand options and offer the highest probability for improved survival.These cases should be performed at highly specialized centers with pre- and post-operative multidisciplinary approaches and extensive preparation regarding cure and risk.A centralized registry for such complex resections and reconstructions may help to guide further multidisciplinary evaluation and future patient selection.
Acknowledgments
None.
CRediT authorship contribution statement
Maria R.Baimas-George:Conceptualization, Investigation,Methodology, Writing - original draft, Writing - review & editing.Ryan C.Pickens:Data curation, Investigation, Methodology,Writing - original draft.Jesse K.Sulzer:Conceptualization, Formal analysis, Writing - review & editing.Dionisios Vrochides:Conceptualization, Data curation, Formal analysis, Writing - review& editing.John B.Martinie:Conceptualization, Data curation,Formal analysis, Writing - review & editing.David M.Levi:Conceptualization, Data curation, Formal analysis, Writing - review &editing.David A.Iannitti:Conceptualization, Data curation, Formal analysis, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964HelsinkiDeclarationand its later amendments or comparable ethical standards.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Two-in-one: A pooled analysis of primary hepatic neuroendocrine carcinoma combine d/collide d with hepatocellular carcinoma
- New variation of median arcuate ligament compression causing hepatic arterial hypoperfusion during liver transplantation
- Echinococcus granulosus: A novel parenchymal sparing surgical treatment
- Serum chitinase-3-like protein 1 is a biomarker of liver fibrosis in patients with chronic hepatitis B in China
- Role of selected criteria and preventive chemotherapy in tumor recurrence after liver transplantation
