New variation of median arcuate ligament compression causing hepatic arterial hypoperfusion during liver transplantation
2020-09-21NoelCassarStephenGregoryKrishnaMenon
Noel Cassar , Stephen Gregory , Krishna Menon
Institute of Liver Studies, King's Healthcare Partners, Denmark Hill Site, London SE5 9RS, UK
Satisfactory blood flow after hepatic arterial anastomosis in liver transplantation is a critical point of the operation.Problems with this anastomosis can result in hepatic artery thrombosis with resultant graft failure and patient morbidity and mortality.Causes of hepatic artery thrombosis include problematic technique, hepatic artery dissection, external compression (e.g.from hematoma),hypercoagulable state, splenic arterial steal and rarer causes such as median arcuate ligament compression (MALC).A careful review of preoperative radiology and imaging will reveal these rare instances and enable a proper intraoperative plan.
A 51-year-old female patient with hepatocellular carcinoma complicating HCV-related cirrhosis underwent liver transplantation using a deceased after brain-death liver from a 63-year-old donor,with a cold ischemia time of 11 h.Caval replacement was carried out and a duct-to-duct biliary anastomosis was performed.The donor liver had an accessory right artery which was reconstructed on the backbench on the gastroduodenal artery.The arterial anastomosis was done between donor common hepatic artery and recipient common hepatic artery.The recipient gastroduodenal artery was divided before the anastomosis.
After the anastomosis no pulsation was visible or felt in the hepatic artery, which lead us to dissect further the recipient coeliac artery and to consider ligation of the splenic artery.However, at the origin of the splenic artery from the coeliac artery there was a ligamentous band which was seen constricting the coeliac artery.We proceeded to release this band and flow in the hepatic artery was immediately improved as judged from pulsatility of the vessel.As per our unit's protocol she had day 1 and day 5 ultrasound of her liver which showed patent vasculature with hepatic artery resistive index of 0.52 and 0.54, respectively, and a CT scan done at day 5 postoperatively again confirmed patent arterial system.She was discharged well 12 days postoperatively.
Ligamentous bands constricting vessels occur in several parts of the body giving rise to several rare syndromes, such as thoracic outlet obstruction [1], popliteal entrapment syndrome [2]and coeliac artery compression [3].There are reports of unsatisfactory blood flow after arterial anastomosis during liver transplantation which were found to be caused by a median arcuate ligament compressing the coeliac artery [3-6].Blood flow was restored once the cause was appropriately dealt with.However in most reports,the compression from the aberrant anatomy was not detected at the time of transplant [3-5].This resulted in patients being reexplored and re-transplanted because of hepatic artery thrombosis and necessitating arterial reconstruction with grafts or conduits in some cases.
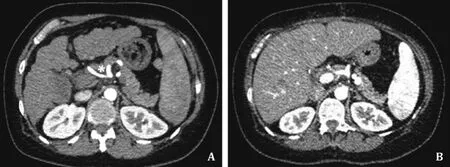
Fig.1.A: Constriction in coeliac artery seen on preoperative imaging for our patient(*); B: CT scan on postoperative day 5 which shows patent coeliac artery without any constriction.
Our case is different to that caused by reported cases of MALC.On reviewing the imaging, in our patient the constriction was seen across the coeliac artery at the origin of the splenic artery (Figs.1 and 2).The CT scan at day 5 postoperatively showed the coeliac artery without any constriction (Fig.1 B).As described by Sugae et al.[7], all three types of MALC (A-C) have the constriction very close to the aorta, and proximal to the splenic (Fig.3).Therefore this is the first time that a ligamentous compression across the coeliac artery at the origin of the splenic artery causing problematic arterial anastomosis has been reported.We may therefore look at our case as a variation of MALC, as suggested in Fig 3.
In the setting of liver transplantation, the incidence of MALC is between 2% and 12% [8-10].With the widespread use of contrast enhanced imaging the radiographic incidence of MALC will probably rise.Screening for MALC during assessment of preoperative imaging is essential.When detected preoperatively, there are several strategies one can adopt.In a survey of 52 European transplant centers, Czigany et al.[10]reported that 12 centers (29%of respondents) routinely divided median arcuate ligament (MAL)found preoperatively, whilst 18 centers (43% of respondents) based their decision on preoperative color Doppler ultrasound or intraoperative assessment of pulse and flowmetry.In this same article [10]the authors reported their experience of 34 patients with MALC during a 7-year period, where 27 patients underwent division of the MAL with standard arterial reconstruction, whilst 4 underwent alternative arterial reconstruction (e.g.aorto-hepatic con-duit).All the MALC recipients who underwent surgical division or alternative reconstruction didn't experience any postoperative complications, which is in contrast with 3 patients with MALC who didn't undergo surgical correction and who developed vascular complications, requiring re-transplantation in one patient.Similarly Jurim et al.[8]reported no vascular complications in 17 patients who had surgical correction of the MAL.In this series two patients underwent reconstruction with an aortic conduit, as flow was still not satisfactory after division of MAL.On the other hand Lubrano et al.[9]reported that division of the MAL is not always necessary and is associated with potential serious complications.In ten patients with MALC they divided the MAL in only one patient, and did standard arterial reconstruction in 6 out of 10 patients with no vascular complications.

Fig.2.Schematic representation of the intraoperative findings (A) and possible working algorithm for MALC detected preoperatively (B).MALC: median arcuate ligament syndrome.

Fig.3.In reported cases of median arcuate ligament syndrome, all cases have the constriction very close to the aorta.In our case, the constriction was more distal, at origin of splenic artery.Modified with permission from Surgery [7].A: diameter of the stenotic part; B: diameter of the normal part; C: length of the stenotic part; D:distance from the aorta; CHA: common hepatic artery; SA: splenic artery.
A possible working algorithm is shown in Fig.2.If MALC is detected preoperatively, an intraoperative assessment is done checking for arterial thrill and using flowmetry and if necessary division of the MAL is undertaken.If this is not enough, an aortic conduit can then be reconstructed.
In conclusion, an awareness of this rare cause of hepatic and coeliac artery compression is crucial to ideally detect them preoperatively, as a proper intraoperative plan can then be undertaken.
Acknowledgments
None.
CRediT authorship contribution statement
Noel Cassar:Data curation, Writing - original draft, Writing - review & editing.Stephen Gregory:Data curation.Krishna Menon:Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by Local Ethical Committee.Consent for publication was obtained from the patient.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Two-in-one: A pooled analysis of primary hepatic neuroendocrine carcinoma combine d/collide d with hepatocellular carcinoma
- A ten-year experience of inferior vena cava reconstruction for malignancy: The importance of a multidisciplinary approach with hepatobiliary surgery
- Echinococcus granulosus: A novel parenchymal sparing surgical treatment
- Serum chitinase-3-like protein 1 is a biomarker of liver fibrosis in patients with chronic hepatitis B in China
- Role of selected criteria and preventive chemotherapy in tumor recurrence after liver transplantation
