Two-in-one: A pooled analysis of primary hepatic neuroendocrine carcinoma combine d/collide d with hepatocellular carcinoma
2020-09-21JiaXiMaoFeiTengKeYanSunCongLiuGuoShanDingWenYuanGuo
Jia-Xi Mao , Fei Teng , Ke-Yan Sun , Cong Liu , Guo-Shan Ding, Wen-Yuan Guo
Department of Liver Surgery and Organ Transplantation, Changzheng Hospital, Navy Medical University, Shanghai 20 0 0 03, China
TotheEditor:
Primary hepatic neuroendocrine carcinoma (PHNEC) combined/collided with hepatocellular carcinoma (HCC) is a rare and intriguing disease with characteristics of two histologically different cancers.Usually, a combined type refers to the cases in which hepatic neuroendocrine carcinoma (HNEC) and HCC components intermingle with each other and cannot be clearly separated in the transitional areas, while a collision type refers to those in which the two distinct cancers occurred simultaneously and independently.Sometimes it is difficult to readily distinguish these two types.We searched PubMed, Medline, China Science Periodical Database, and VIP Database with the publication from January 1980 to January 2019, using the keywords (“hepatic neuroendocrine carcinoma”or “HNEC”) and (“hepatocellular carcinoma”or“HCC”).After manually excluding records on secondary HNEC and other types of liver cancer, a total of 28 cases in 24 reports [1-24]were identified and summarized in Table 1.The current summary thus aimed to provide more information about the clinical manifestations, managements and prognosis of this rare disease.
The 28 cases included 26 men and 2 women, with a median age of 68 years (range, 43-77 years).The clinical symptoms of nine cases were not described in the original reports.Among the remaining 19 cases, 10 (10/19, 52.6%) had no symptoms and were identified in health examination or follow-up for hepatitis, while the other nine (9/19, 47.4%) presented with intermittent upper or right upper abdominal pain, accompanied sporadically by jaundice(n= 1), back pain (n= 1), shiver (n= 1), or weight loss (n= 1).A history of hepatitis B was found in 9 patients and hepatitis C in 13 patients, while 3 cases had no history of hepatitis and the status of hepatitis in the remaining three cases was not reported.Analysis of preoperative tumor markers in the 28 patients estimated the positive rate of alpha-fetoprotein (AFP) at 77%, carbohydrate antigen 125 (CA125) at 20%, CA19-9 at 10%, carcinoembryonic antigen(CEA) at 17%, neuron-specific enolase (NSE) at 100% and protein induced by vitamin K absence or antagonist-II (PIVKA-II) at 50%.Pathological diagnoses were determined using specimens in 24 patients with surgical resection and the others with percutaneous liver biopsy.Cirrhosis was found in 10 cases and liver fibrosis in three cases, and seven cases were reported non-cirrhotic while the background of liver was not mentioned in the other eight cases.The aggregated data for tumor-related characteristics in 28 patients were shown in Table 2.
The 28 patients were followed up for 0.5-28 months after treatments, and 13 patients died because of tumor recurrence and metastasis (eight cases), progressive disease (three cases), and perioperative complications such as liver and renal failure (two cases).The 1 and 2 year survival rates were 42% and 25%, respectively, with the median survival time of 17.88 months.Univariate analysis showed that hepatitis viral infection and tumor recurrence time were related with survival [harzard ratio(HR) = 0.122,P= 0.005; HR = 0.680,P= 0.007, respectively],while multivariate analysis indicated that tumor recurrence time was the only independent risk factor for survival (P= 0.022,Table 3).Postoperative tumor recurrence sites were intrahepatic(six cases), bone (five cases), lymph nodes (four cases, including two in abdominal lymph nodes and two in para-aortic lymph nodes), peritoneum (one case), ovary (one case), and adrenal gland (one case).The time to recurrence was 0.75-20 months(median 6 months).Multivariate analysis indicated that preoperative AFP and tumor number were independent risk factors for tumor recurrence (HR = 0.150,P= 0.022; HR = 13.987,P= 0.011, respectively, Table 4).PHNEC, when occurred by itself, was highly malignant with 3- and 5-year overall survival of 55% and 48% respectively [25].Especially, the 5 year recurrence rate of PHNEC, which was 77%-100%, was even higher than HCC [ 25 , 26 ].Therefore, elevated AFP and hepatitis infection, which indicated a higher proportion of HCC in the combined/collided carcinoma, predicted a relatively better prognosis in the PHNEC combined/collided HCC.
Compared with primary pancreatic neuroendocrine tumor, the prognosis of PHNEC was poorer, with an overall survival of 25.4 ±6.7 months [27].The current results suggested that the prognosis of PHNEC combined/collided with HCC was even worse,with a median survival of only 17.88 months.Though preoperative diagnosis is difficult, PHNEC combined/collided with HCC is usually accompanied by hepatitis C or B and cirrhosis, without apparent symptoms or presented with intermittent upper or right upper abdominal pain.Elevated NSE and/or AFP are the most predictive preoperative tumor markers.Pathology and immunohistochemistryare the gold standards for diagnosis.Surgical resection is the most commonly used treatment and prolongs patient survival compared with conservative treatments.Regular follow-ups are required after surgery, and re-examinations are recommended at least every 1-2 months within the first postoperative year, including NSE and AFP, enhanced computed tomography/magnetic resonance imaging of the upper abdomen, and single photon emission computed tomography of bones.
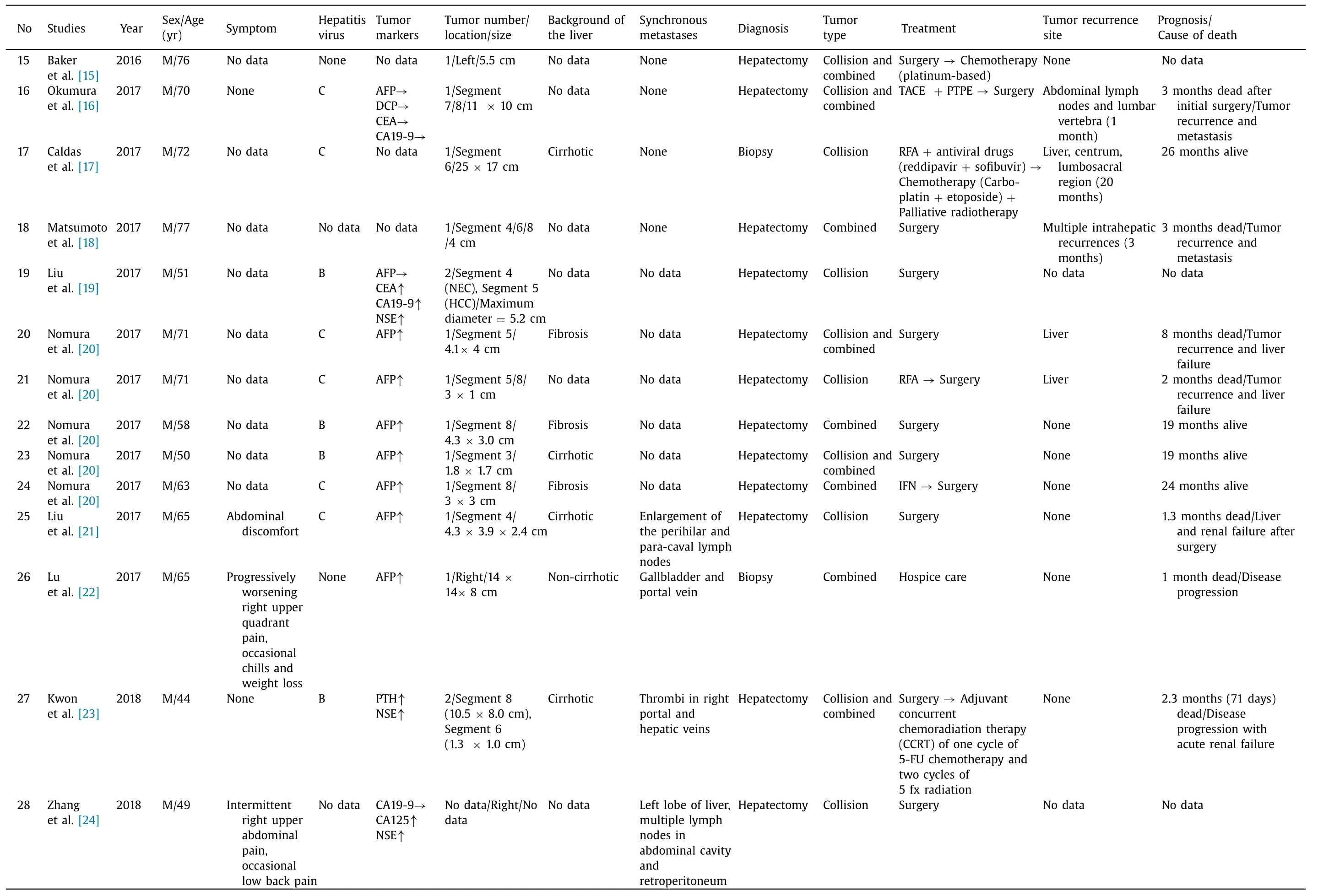
Table 1(continued)
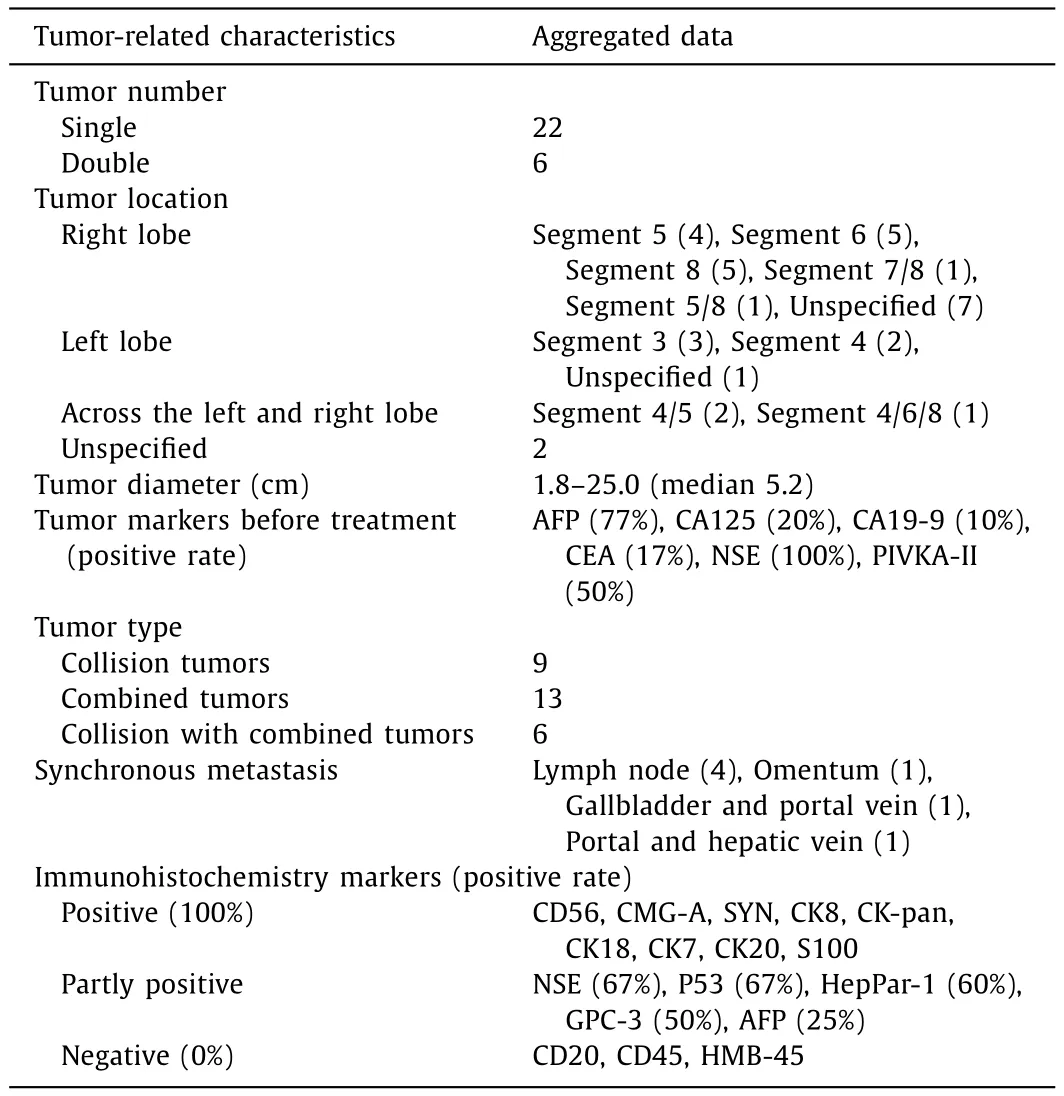
Table 2Tumor-related characteristics in 28 patients with PHNEC combined/collided with HCC.
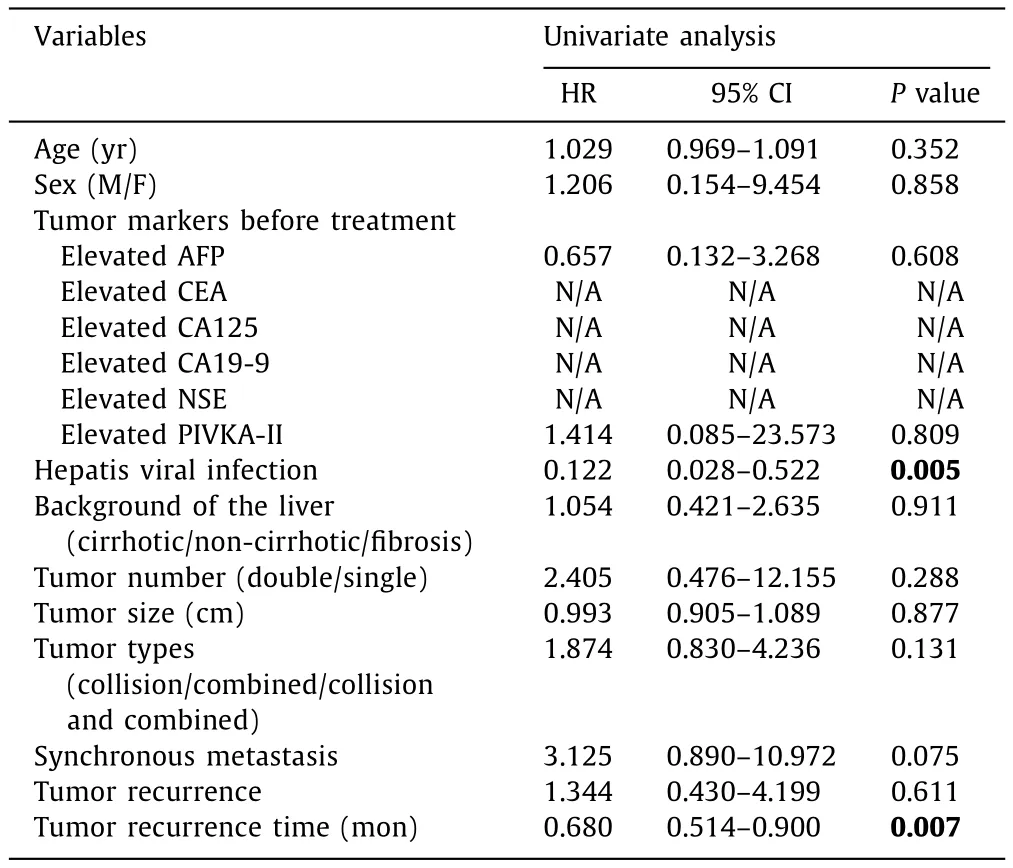
Table 3Uni- and multivariate analysis of indicators affecting the overall survival of patients with PHNEC combined/collided with HCC.
In conclusion, PHNEC combined/collided with HCC is a rare but highly malignant disease, with a median overall survival of 17.88 months and median time to recurrence of 6 months.Surgical comprehensive therapies are recommended, keeping in mind the biological behaviors of both HNEC and HCC.

Table 4Uni- and multivariate analysis of indicators affecting the tumor recurrence of PHNEC combined/collided with HCC.
Acknowledgments
We thank Nikki March for language editing.
CRediT authorship contribution statement
Jia-Xi Mao:Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources,Writing - original draft.Fei Teng:Conceptualization, Data curation, Formal analysis, Funding acquisition, Project administration,Resources, Supervision, Writing - review & editing.Ke-Yan Sun:Formal analysis, Funding acquisition, Project administration, Resources, Software, Writing - review & editing.Cong Liu:Conceptualization, Data curation, Formal analysis, Resources, Software, Writing - original draft.Guo-Shan Ding:Project administration, Resources, Supervision, Validation, Visualization, Writing - review &editing.Wen-Yuan Guo:Conceptualization, Funding acquisition,Investigation, Project administration, Resources, Supervision, Validation, Writing - review & editing.
Funding
This project was supported by grants from the National Natural Science Foundation of China (81702923, 81971503), the Foundation of Shanghai Science and Technology Commission (18ZR1439300),the Precision Medicine Project of Navy Medical University, China(2017JZ50) and the Pyramid Talent Project of Changzheng Hospital.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group