溃疡性结肠炎患者肠道菌群含量变化及其与炎性因子及TOLL样受体分子的相关性
2020-08-27李会荣崔昭梁博
李会荣 崔昭 梁博
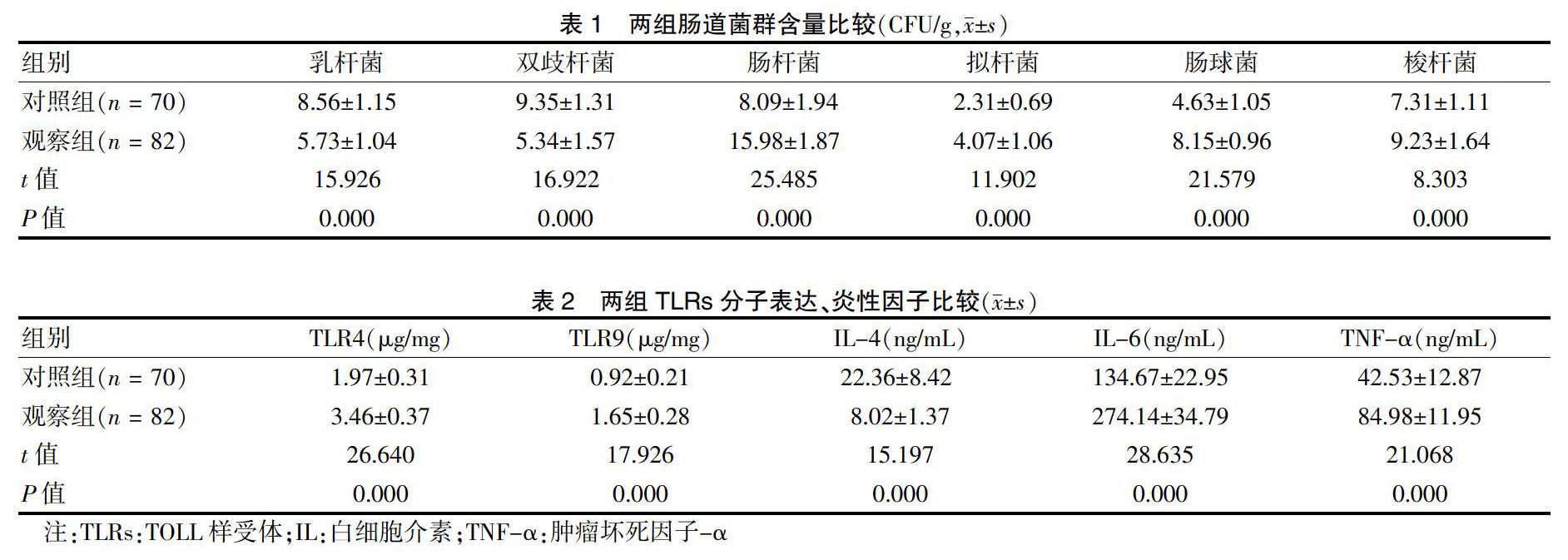

[摘要] 目的 探討溃疡性结肠炎(UC)患者肠道菌群含量变化及其与炎性因子及TOLL样受体(TLRs)分子的相关性。 方法 选取2016年2月~2018年8月河北省保定市第二医院收治的UC患者82例作为观察组,另选取同期行健康体检的志愿者70例作为对照组,检测白细胞介素(IL)-4(IL-4)、IL-6、肿瘤坏死因子-α(TNF-α)、肠道菌群含量情况以及TLRs分子(TLR4、TLR9)表达情况并进行比较,采用Pearson相关性分析TLRs分子表达与肠道菌群、炎性因子的相关性。 结果 观察组肠杆菌、拟杆菌、肠球菌以及梭杆菌含量高于对照组,而乳杆菌、双歧杆菌含量则低于对照组,差异均有统计学意义(均P < 0.05)。观察组TLR4、TLR9、IL-6、TNF-α高于对照组,IL-4低于对照组,差异均有统计学意义(均P < 0.05)。Pearson相关性分析结果显示,UC患者TLR4、TLR9与肠杆菌、拟杆菌、肠球菌、梭杆菌、IL-6、TNF-α呈正相关(r > 0,P < 0.05),与乳杆菌、双歧杆菌、IL-4呈负相关(r < 0,P < 0.05)。结论 UC患者体内肠道菌群失调,其可通过促进TLRs分子表达进而提高促炎因子水平,降低抑炎因子水平,介导肠黏膜炎性反应。
[关键词] 溃疡性结肠炎;肠道菌群;炎性因子;TOLL样受体;相关性
[中图分类号] R574.62 [文献标识码] A [文章编号] 1673-7210(2020)07(a)-0156-04
[Abstract] Objective To investigate the changes of intestinal flora in patients with ulcerative colitis (UC) and its correlation with inflammatory factors and TOLL-like receptors (TLRs) molecules. Methods A total of 82 patients with UC admitted to the NO.2 Hospital of Baoding Hebei Province from February 2016 to August 2018 were selected as the observation group, and 70 volunteers who underwent physical examination during the same period were selected as the control group. The levels of interleukin (IL)-4, IL-6, tumor necrosis factor-α (TNF-α), intestinal flora content and the expression of TLRs molecules (TLR4 and TLR9) were detected and compared. Pearson correlation was used to analyze the correlation between TLRs expression and intestinal flora and inflammatory factors. Results The contents of Enterobacter, Bacteroides, Enterococcus and Fusobacterium in the observation group were higher than those in the control group, while the contents of Lactobacillus and Bifidobacterium in the observation group were lower than those in the control group, with statistically significant differences (all P < 0.05). TLR4, TLR9, IL-6 and TNF-α in the observation group were higher than those in the control group, and IL-4 was lower than that in the control group, with statistically significant differences (all P < 0.05). Pearson correlation analysis showed that TLR4 and TLR9 in UC patients were positively correlated with Enterobacter, Bacteroides, Enterococcus, Fusobacterium, IL-6 and TNF-α (r > 0,P < 0.05), but negatively correlated with Lactobacillus, Bifidobacterium and IL-4 (r < 0,P < 0.05). Conclusion In patients with UC, intestinal flora is dysregulated, which can promote the expression of TLRs molecules to increase the level of pro-inflammatory factors, reduce the level of anti-inflammatory factors, and mediate the inflammatory response of intestinal mucosa.
TOLL基因最早于果蝇体内发现,其编码的跨膜受体蛋白称TLR,TLR是一个新型的细胞受体蛋白家族,而TLRs则是体内重要的模式识别受体,具有识别多种病原菌的能力,通过下游髓样分化因子88以促进核因子-κB进入细胞核,最终启动多种炎性因子表达[14-15]。其中TLR4能识别脂多糖,同时能介导肠上皮细胞对细菌胞壁成分的反应,有研究表明,高TLR4水平可通过影响肠上皮细胞对细菌胞壁成分的信号传递,促进炎性因子的增殖,导致肠道炎性反应[16];TLR9能够识别细菌的非甲基化的胞嘧啶-磷酸-鸟嘌呤基序,可介导胞嘧啶-磷酸-鸟嘌呤基序激活T细胞、DC细胞、B细胞等多种免疫细胞,诱导免疫应答,参与UC的发生发展[17]。本研究中观察组TLR4、TLR9高于对照组,可见肠黏膜中的TLR4、TLR9参与UC的病情进展,与陈胜等[18]学者研究结果一致。进一步Pearson相关性分析结果提示,TLR4、TLR9与肠杆菌、拟杆菌、肠球菌、梭杆菌呈正相关,与乳杆菌、双歧杆菌呈负相关,提示UC患者中肠道菌群紊乱可促进TLR4、TLR9高表达,与李顺清等[15]研究结论相符。TNF-α是炎症启动因子,参与着炎症的发生发展过程[19]。IL-4为抑炎因子,可下调炎症细胞因子基因的转录及其分泌,发挥抗炎和免疫调节作用,是肠道免疫的重要因子[20]。IL-6是一种促炎细胞因子,可加剧肠黏膜炎性反应[21]。本研究中观察组IL-6、TNF-α均高于对照组,IL-4低于对照组,可见IL-6、TNF-α、IL-4均参与着UC的病情进展过程,同时相关性分析也显示TLR4、TLR9与IL-6、TNF-α呈正相关,与IL-4呈负相关,说明肠黏膜中的TLR4、TLR9可能通过识别肠道内异常繁殖的肠杆菌、肠球菌等条件致病菌及拟杆菌、梭杆菌等病原菌调控IL-6、TNF-α、IL-4水平进而介导炎性反应[22-25]。
综上所述,UC患者体内肠道菌群失调,其可通过促进TLRs分子表达进而提高促炎因子水平,降低抑炎因子水平,介导肠黏膜炎性反应。
[参考文献]
[1] Ungaro R,Mehandru S,Allen PB,et al. Ulcerative colitis [J]. Lancet,2017,389(10080):1756-1770.
[2] 李世权,吕晓丹,谢彦飞,等.溃疡性结肠炎小鼠外周血和结肠组织中Tfh、Tfr细胞水平变化及意义[J].山东医药,2018,58(9):9-12.
[3] 施煜燕,周建波.老年溃疡性结肠炎患者炎症细胞因子、T淋巴细胞亚群和凝血功能变化[J].中国老年学杂志,2018,38(2):382-384.
[4] Adams SM,Bornemann PH. Ulcerative colitis [J]. Am Fam Physician,2013,87(10):699-705.
[5] 杨斐,郑晓娟,刘近春,等.溃疡性结肠炎肠道菌群失调的治疗进展[J].胃肠病学,2018,23(1):56-58.
[6] Ordás I,Eckmann L,Talamini M,et al. Ulcerative colitis [J]. Lancet,2012,380(9853):1606-1619.
[7] 中华医学会消化病学分会炎症性肠病学组.炎症性肠病诊断与治疗的共识意见(2012年·广州)[J].中华内科杂志,2012,51(10):818-831.
[8] Cross R,Ko CW,Singh S. Mild-to-Moderate Ulcerative Colitis Guideline [J]. Gastroenterology,2019,156(3):768.
[9] 王晓宏,张邑.槐花散联合仙方活命饮治疗溃疡性结肠炎临床研究[J].国际中医中药杂志,2017,39(8):701-704.
[10] Fukuda T,Naganuma M,Kanai T. Current new challenges in the management of ulcerative colitis [J]. Intest Res,2019,17(1):36-44.
[11] 张永利,申妮.溃疡性结肠炎患者肠道菌群的变化特征[J].河北医药,2018,40(7):1054-1057.
[12] 刘志威,王学群,李甜甜,等.溃疡性结肠炎患者肠道菌群变化的临床意义[J].胃肠病学和肝病学杂志,2016, 25(5):554-556.
[13] 李静,陈卫刚.肠道菌群治疗溃疡性结肠炎的研究进展[J].实用医学杂志,2017,33(24):4189-4192.
[14] 谭芳.益生菌对溃疡性结肠炎大鼠肠黏膜TLRs表达的影响[D].乌鲁木齐:新疆医科大学,2015.
[15] 李顺清.溃疡性结肠炎患者肠道菌群含量以及细胞因子、TLRs分子表达情况的检测[J].海南医学院学报,2017, 23(5):662-664,668.
[16] 徐晓云,李冬斌,李彬.TLR4、NF-κB p65、IL-8在溃疡性结肠炎中的表达[J].疑难病杂志,2012,11(3):181-183,封3.
[17] 何雁,王启之.Toll样受体9与溃疡性结肠炎[J].安徽医药,2009,13(6):593-595.
[18] 陈胜,邹开芳,杨天,等.Toll样受体(TLR)2、TLR4和TLR9在大鼠结肠炎模型结肠组织中的表达及其意义[J].胃肠病学,2007,12(6):339-343.
[19] Panés J,Alfaro I. New treatment strategies for ulcerative colitis [J]. Expert Rev Clin Immunol,2017,13(10):963-973.
[20] 岳文杰,刘懿,徐薇,等.溃疡性结肠炎(UC)肠黏膜中IL-2、IL-4、IL-17和IL-10的表达特点及其与疾病活动度的关系[J].复旦学报:医学版,2012,39(5):454-459,488.
[21] 黄鹤,伦伟健,梁晓燕,等.沙利度胺对溃疡性结肠炎大鼠MMP-9、COX-2、IL-6水平的影響[J].中国老年学杂志,2016,36(7):1594-1596.
[22] 张爱军,朱叶珊,费亚军等.中药封包电磁波导入辅治溃疡性结肠炎的疗效及对血清炎性因子和免疫球蛋白的影响[J].疑难病杂志,2018,17(4):370-373.
[23] 邓台燕,全大祥,吴彬,等.复方黄柏液联合美沙拉嗪对溃疡性结肠炎及肠道菌群和血清炎症因子的影响[J].中国现代医学杂志,2016,26(9):124-127.
[24] 王云滨,陈霞.益生菌联合美沙拉嗪对溃疡性结肠炎患者血清炎症因子及免疫功能的影响[J].中国现代医生,2020,58(9):40-43.
[25] 李琳,钟青.溃疡性结肠炎患者肠道菌群变化与细胞因子、TLRs分子表达的相关性研究[J].传染病信息,2017, 30(6):361-364.
(收稿日期:2019-07-30)
