血清神经生长因子及细胞免疫水平在乳腺癌中的表达及其与临床病理特征的相关性
2020-05-25王文慧温媛媛陈豪
王文慧 温媛媛 陈豪
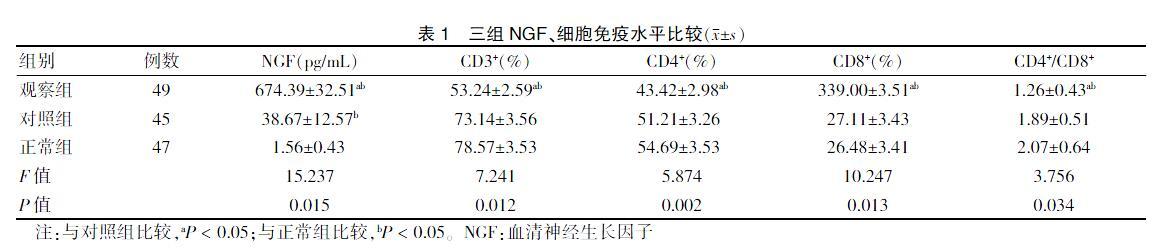
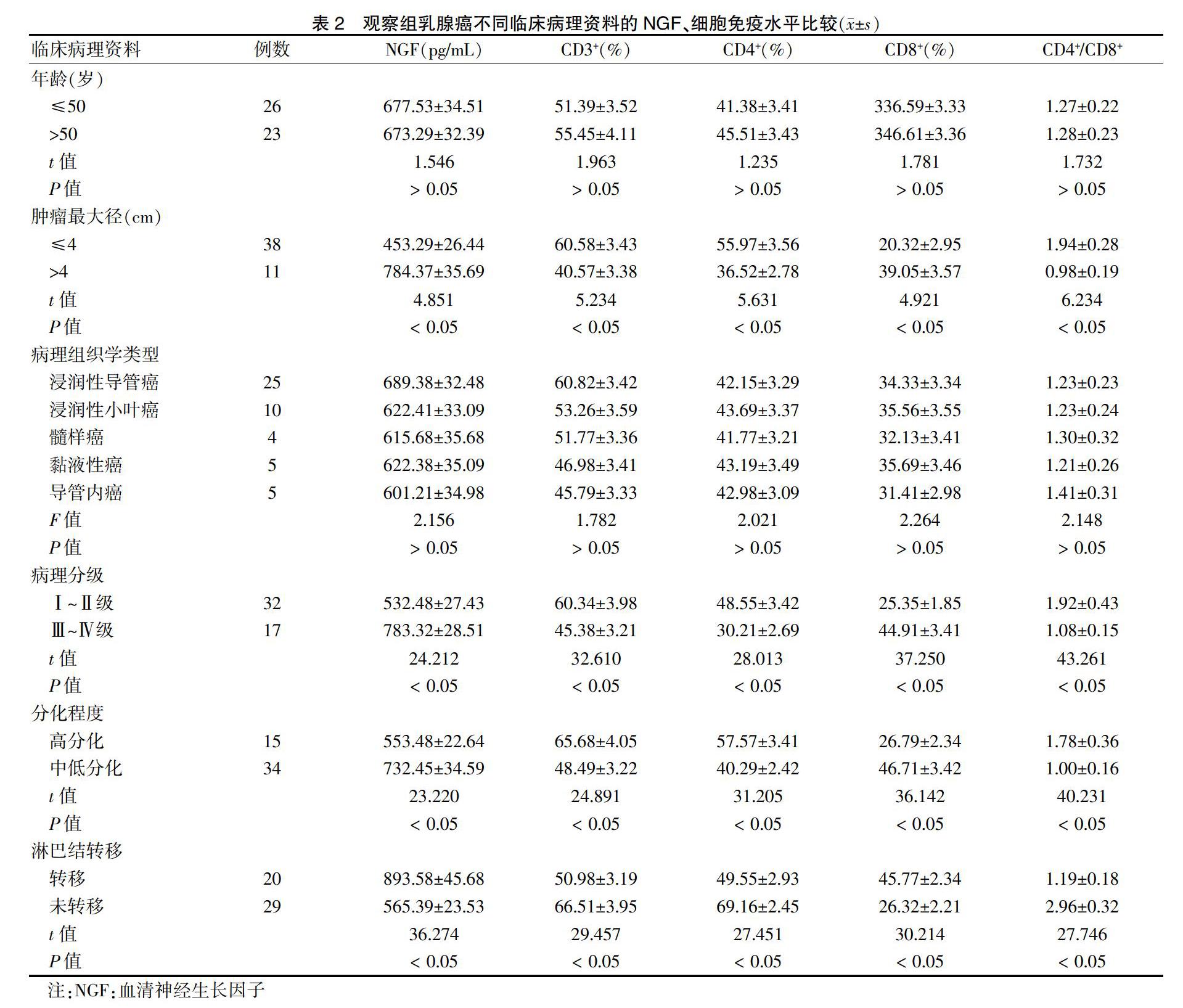
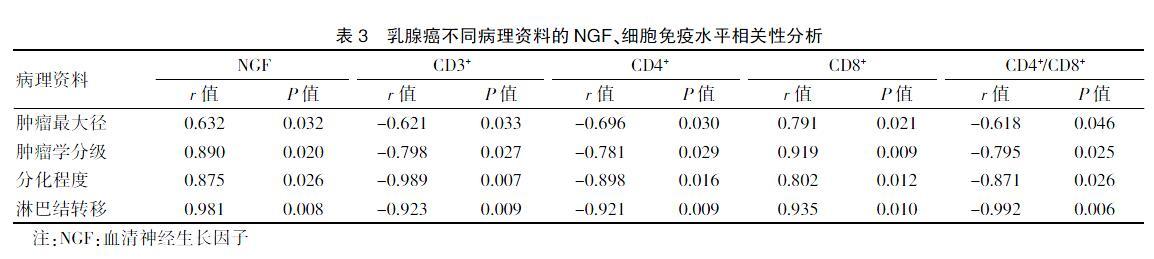
[摘要] 目的 探討血清神经生长因子(NGF)及细胞免疫水平在乳腺癌患者中的表达及其与临床病理特征的相关性。 方法 选择2015年3月~2018年2月在杭州市妇产科医院及浙江省舟山医院确诊的乳腺癌患者49例,设为观察组;选择同期入院的乳腺良性疾病患者45例,设为对照组;选择同期入院健康体检女性47名,设为正常组。采用酶联免疫吸附试验测定各组NGF表达水平;采用流式细胞仪测定各组CD3+、CD4+、CD8+及CD4+/CD8+水平;记录并统计患者临床病理资料,分析各组和观察组乳腺癌不同临床病理资料的NGF、细胞免疫水平;采用Pearson分析NGF、细胞免疫水平与乳腺癌患者临床病理资料的相关性。 结果 三组NGF、细胞免疫水平比较,差异均有统计学意义(P < 0.05)。观察组NGF水平高于对照组与正常组,且对照组NGF水平高于正常组,差异均有统计学意义(P < 0.05)。观察组CD3+、CD4+及CD4+/CD8+水平低于对照组与正常组,CD8+水平高于对照组与正常组,差异均有统计学意义(P < 0.05);对照组与正常组CD3+、CD4+、CD8+及CD4+/CD8+水平比较,差异无统计学意义(P > 0.05)。乳腺癌组织中NGF、CD3+、CD4+、CD8+及CD4+/CD8+水平在年龄、病理组织学类型方面比较,差异无统计学意义(P > 0.05);乳腺癌组织中NGF、CD3+、CD4+、CD8+及CD4+/CD8+水平在肿瘤最大径、病理分级、分化程度及淋巴结转移方面比较,差异均有统计学意义(P < 0.05);Pearson相关性分析显示:NGF、CD8+水平与肿瘤最大径、病理分级、分化程度及淋巴结转移呈正相关(P < 0.05);CD3+、CD4+及CD4+/CD8+水平与肿瘤最大径病理分级、分化程度及淋巴结转移呈负相关(P < 0.05)。 结论 NGF在乳腺癌患者中呈高表达,导致机体细胞免疫水平下降,且二者表达水平与病理特征具有相关性,加强NGF及细胞免疫水平测定能评估患者疾病严重程度,指导临床治疗。
[关键词] 血清神经生长因子;细胞免疫水平;乳腺癌;病理特征;相关性;酶联免疫吸附试验;流式细胞仪
[中图分类号] R737.9 [文献标识码] A [文章编号] 1673-7210(2020)04(b)-0088-05
Expression of serum nerve growth factor and cellular immunity in breast cancer and its correlation with clinicopathological feature
WANG Wenhui1 WEN Yuanyuan2 CHEN Hao1
1.Department of Pathology, Hangzhou Maternity Hospital, Zhejiang Province, Hangzhou 310008, China; 2.Pathological Diagnosis Center, Zhejiang Zhoushan Hospital, Zhejiang Province, Zhoushan 316021, China
[Abstract] Objective To investigate the expression of serum nerve growth factor (NGF) and cellular immunity in breast cancer patients and its correlation with clinicopathological feature. Methods A total of 49 breast cancer patients diagnosed in Hangzhou Maternity Hospital and Zhejiang Zhoushan Hospital from March 2015 to February 2018 were selected as the observation group. A total of 45 patients with benign breast disease who were hospitalized at the same time were selected as the control group. A total of 47 female patients with physical examination at the same time were selected as the normal group. The expression levels of NGF in each group were determined by enzyme-linked immunosorbent assay. The levels of CD3+, CD4+, CD8+ and CD4+/CD8+ in each group were determined by flow cytometry. The clinicopathological data of the patients were recorded and counted. The levels of NGF and cellular immunity in each group and the levels of NGF and cellular immunity in different clinicopathological data of breast cancer in the observation group were analyzed. The correlation between NGF, cellular immunity level and clinicopathological data of breast cancer patients was analyzed by Pearson analysis. Results The levels of NGF and cellular immunity in the three groups were statistically significant (P < 0.05). The level of NGF in the observation group was higher than that in the control group and the normal group, and the level of NGF in the control group was higher than that in the normal group, with statistically significant differences (P < 0.05). The levels of CD3+, CD4+ and CD4+/CD8+ in the observation group were lower than those in the control group and the normal group, and the level of CD8+ was higher than that in the control group and the normal group, with statistically significant differences (P < 0.05). There was no significant difference in the levels of CD3+, CD4+, CD8+ and CD4+/CD8+ between the control group and the normal group (P > 0.05). The levels of NGF, CD3+, CD4+, CD8+ and CD4+/CD8+ in breast cancer tissues were not statistically significant differences in terms of age and histopathological type (P > 0.05). The levels of NGF, CD3+, CD4+, CD8+ and CD4+/CD8+ in breast cancer tissues were compared in terms of tumor maximum diameter, pathological grading, differentiation degree and lymph node metastasis, with statistically significant differences (P < 0.05). The Pearson correlation analysis results showed that the NGF and CD8+ levels were positively correlated with the maximum tumor diameter, pathological grading, differentiation degree and lymph node metastasis (P < 0.05). The levels of CD3+, CD4+ and CD4+/CD8+ were negatively correlated with the maximum tumor diameter, pathological grading, differentiation degree and lymph node metastasis (P < 0.05). Conclusion The high expression of NGF in breast cancer patients leads to the decline of cellular immunity level in the body, and the expression level of both is correlated with the pathology feature. Strengthening the determination of NGF and cellular immunity level can assess the severity of the disease in patients and guide clinical treatment.
乳腺癌的发生发展是一个多因素过程,常伴有细胞免疫水平的变化[16-17]。研究表明[18-19],肿瘤患者外周血肿细胞免疫水平常呈低表达。CD4+T细胞能调控局部炎症与细胞毒相关的免疫应答,能促进机体产生抗体;此外,CD4+T细胞还能活化自然杀伤细胞与巨噬细胞,提高巨噬细胞的杀伤能力;CD8+T细胞毒性相对较轻,在杀死肿瘤细胞中发挥了重要的作用。研究表明[20-21],细胞免疫对于肿瘤免疫反应的抑制能在淋巴组织中表现,能种植效应细胞活化阶段,改变肿瘤的微环境,从而干扰机体正常的抗肿瘤免疫应答,抑制肿瘤细胞的清除。乳腺癌患者中细胞免疫水平受影响因素较多,包括肿瘤的分期、肿瘤大小、分化程度等。本研究中,分析结果显示:NGF、CD8+水平与肿瘤最大径、病理分级、分化程度及淋巴结转移呈正相关(P < 0.05);CD3+、CD4+及CD4+/CD8+水平与肿瘤最大径、病理分级、分化程度及淋巴结转移呈负相关(P < 0.05)。可见乳腺癌患者中细胞免疫水平与病理表现存在相关性。为了提高乳腺癌患者诊断、治疗效果,可加强患者NGF和细胞免疫水平测定,评估患者疾病严重程度;对于确诊的乳腺癌患者尽早给予手术、放化疗等治疗,且治疗过程中加强患者NGF和细胞免疫水平测定能评估患者预后,可以视检测结果调整治疗方案,使得患者的治疗更具科学性[22]。
综上所述,NGF在乳腺癌患者中呈高表达,导致机体细胞免疫水平下降,且二者表达水平与病理表现具有相关性,加强NGF及细胞免疫水平测定能评估患者疾病严重程度,指导临床治疗。
[参考文献]
[1] 張季,李杨,杨思原,等.乳腺癌患者血清神经生长因子和低亲和力受体p75表达水平的变化及其意义[J].中国普通外科杂志,2017,26(11):1498-1501.
[2] 李福喜,邵文凤,唐芮,等.埃兹蛋白477位酪氨酸的磷酸化在神经生长因子前体促进乳腺癌细胞侵袭中起关键作用[J].南方医科大学学报,2016,36(7):898-903.
[3] Zhu J,Zhang XR,Yang H. Effects of combined epidural and general anesthesia on intraoperative hemodynamic responses,postoperative cellular immunity,and prognosis in patients with gallbladder cancer:A randomized controlled trial [J]. Medicine(Baltimore),2017,96(10):e6137.
[4] 吴立春,谷仕艳,代黄梅,等.长链非编码RNA-ROR在乳腺癌患者血清、癌组织中的表达变化及其临床意义[J].山东医药,2017,57(32):78-80.
[5] Xiao Z,Wang C,Sun Y,et al. Can Aidi injection restore cellular immunity and improve clinical efficacy in non-small-cell lung cancer patients treated with platinum-based chemotherapy. A meta-analysis of 17 randomized controlled trials following the PRISMA guidelines [J]. Medicine(Baltimore),2016,95(44):e5210.
[6] Chen X,Yin B,Lian RC,et al. Modulatory effects of vitamin D on peripheral cellular immunity in patients with recurrent miscarriage [J]. Am J Reprod Immunol,2016,76(6):432-438.
[7] 王松,薛文华,赵晓玉,等.多西他赛、表柔比星联合环磷酰胺对不同分子分型乳腺癌患者临床疗效及肿瘤标志物表达的影响[J].中国药房,2017,28(23):3212-3216.
[8] 刘玉芳,李琳,许岩垒,等.三黄煎剂联合新辅助化疗对乳腺癌的近期疗效及对Survivin及Ki-67表达的影响[J].中药材,2016,39(9):2143-2146.
[9] Gruber IV,Hartkopf AD,Hahn M,et al. Relationship Between Hematogenous Tumor Cell Dissemination and Cellular Immunity in DCIS Patients [J]. Anticancer Res,2016, 36(5):2345-2351.
[10] Lundgren S,Lyden E,Burdorf A,et al. Left ventricular assist device does not improve cellular immunity in end-stage heart failure[J]. J A Coll Cardiol,2018,71(11):A950.
[11] Grifoni A,Angelo M,Sidney J,et al. Patterns of Cellular Immunity Associated with Experimental Infection with rDEN2Δ30 (Tonga/74)Support Its Suitability as a Human Dengue Virus Challenge Strain [J]. J Virol,2017,91(8). pii:e02133-16.
[12] 李杰宝,喻晓程,田野,等.果蝇zeste基因增强子同源物2在乳腺癌组织中的表达及其与乳腺癌分子分型的相关性[J].中华实验外科杂志,2016,33(9):2196-2199.
[13] 王博,王宇,胡少军,等.卡培他滨联合多西他赛对乳腺癌肝转移患者血管内皮生长因子、肝细胞生长因子及预后的影响[J].中国免疫学杂志,2017,33(11):1706-1708,1712.
[14] 钱朋飞,张树平,邓素华,等.尿多酸肽联合化疗对乳腺癌患者免疫功能的影响[J].中华肿瘤防治杂志,2016, 23(19):1307-1311.
[15] 张楠,孙刚,马斌林.散发性乳腺癌患者乳腺癌易感基因1mRNA与蛋白的表达变化差异及意义[J].中华实验外科杂志,2016,33(4):884-887.
[16] Khaled AR,Limaye A,Bassiouni R,et al. Abstract P4-04-12:Enhancing the immunogenicity of breast cancer cells to stimulate innate immunity and augment the effects of cellular immunotherapy [J]. Cancer Res,2016,76(4 Supplement):P4-04-12-P4-04-12.
[17] 金妍.細胞免疫功能检测在乳腺癌临床分期及预后评估中的价值分析[J].中国现代医生,2019,57(12):124-126.
[18] 程枫,朱磊,陈欢,等.富含半胱氨酸分泌性酸性蛋白在乳腺癌组织中的表达及其临床意义[J].中国临床药理学杂志,2017,33(1):18-20.
[19] Cook KL,Soto-Pantoja DR,Clarke PA,et al. Endoplasmic reticulum stress protein GRP78 modulates lipid metabolism to control drug sensitivity and anti-tumor immunity in breast cancer [J]. Cancer Res,2016,76(19):5657-5670.
[20] 郭崇勇,丁宝忠,李柏成,等.三阴性乳腺癌组织中ALDH1、TGF-β_1蛋白的表达变化及其对预后的影响[J].山东医药,2017,57(46):61-63.
[21] 曾榃伦,吕铮,崔久嵬,等.肿瘤浸润淋巴细胞在三阴性乳腺癌疗效预测及预后评估中作用的研究进展[J].中国医药,2018,13(7):1103-1106.
[22] 周玉冰,殷德涛,李朵璐,等.细胞周期蛋白依赖性激酶11在乳腺癌组织中的表达及临床意义[J].中华实验外科杂志,2016,33(3):639-642.
(收稿日期:2019-08-21 本文编辑:顾家毓)
