熊去氧胆酸对妊娠期肝内胆汁淤积症患者妊娠结局的影响
2020-02-29应柳青施锦梅潘丹
应柳青 施锦梅 潘丹


[摘要] 目的 探討熊去氧胆酸对妊娠期肝内胆汁淤积症(ICP)患者妊娠结局的影响。 方法 选取2012年1月~2018年4月我院妇产科住院治疗ICP患者90例,随机分为观察组和对照组,每组各45例。对照组均予以能量合剂等常规治疗。观察组在对照组基础上加用熊去氧胆酸0.25 g/次,2次/d,口服,两组连用14 d。观察两组治疗前和治疗7 d后肝功能水平变化,并比较其临床疗效及妊娠结局。 结果 治疗14 d后,两组血清TBA、ALT和AST水平均较治疗前显著下降(P<0.01或P<0.05),且观察组下降值大于对照组(P<0.05);同时观察组临床总有效率较对照组更佳(χ2=4.54,P<0.05)。观察组发生不良妊娠结局4例(8.88%),对照组11例(24.44%),观察组不良妊娠结局发生率低于对照组(χ2=3.92,P<0.05)。 结论 熊去氧胆酸治疗ICP患者的效果确切,能明显改善肝功能指标;降低不良妊娠结局,保护母婴安全。
[关键词] 肝内胆汁淤积症;妊娠期;熊去氧胆酸;妊娠结局
[中图分类号] R714.255 [文献标识码] B [文章编号] 1673-9701(2020)01-0059-04
Effect of ursodeoxycholic acid on pregnancy outcome in patients with intrahepatic cholestasis of pregnancy
YING Liuqing SHI Jinmei PAN Dan
Department of Gynaecology, Taizhou Municipal Hospital in Zhejiang Province, Taizhou 318000, China
[Abstract] Objective To investigate the effect of ursodeoxycholic acid on pregnancy outcome in patients with intrahepatic cholestasis of pregnancy (ICP). Methods 90 patients with ICP in the department of obstetrics and gynaecology in our hospital from January 2012 to April 2018 were randomly divided into observation group and control group, with 45 cases in each group. The control group was given conventional treatment such as energy mixture. The observation group was treated with ursodeoxycholic acid 0.25 g/time, twice/d, orally, based on the treatment of the control group. The two groups were treated for 14 days. The changes of liver function before and after 7 days of treatment were observed, and the clinical efficacy and pregnancy outcome were compared. Results After 14 days of treatment, the serum levels of TBA, ALT and AST in the two groups were significantly lower than those before treatment(P<0.01 or P<0.05), and the decrease in the observation group was greater than that in the control group (P<0.05). At the same time, the total effective rate of the observation group was better than that of the control group (χ2=4.54, P<0.05). There were 4 cases (8.88%) of adverse pregnancy outcomes in the observation group and 11 cases (24.44%) in the control group. The incidence of adverse pregnancy outcomes in the observation group was lower than that in the control group (χ2=3.92, P<0.05). Conclusion Ursodeoxycholic acid in the treatment of ICP patients has positive effect, which can significantly improve liver function indicators, reduce adverse pregnancy outcomes and protect maternal and child safety.
[Key words] Intrahepatic cholestasis; Pregnancy; Ursodeoxycholic acid; Pregnancy outcome
妊娠期肝内胆汁淤积症(Intrahepatic cholestasis of pregnancy,ICP)是妊娠中晚期特发性黄疸,主要表现为皮肤瘙痒、肝功能异常、食欲下降及黄疽,易发生早产、宫内窘迫、死胎等并发症,增加围母婴的死亡率,因此,及时采取有效的治疗措施显得尤为重要[1-2]。ICP的发病机制迄今尚不完全明确,临床上尚无特效的治疗药物,常用的药物为保肝、利胆药物[3-4]。熊去氧胆酸是一种临床常用的代表性利胆剂,是目前治疗ICP的首选药物,但其对妊娠结局的影响国内外报道不多[5-6]。本研究观察熊去氧胆酸对ICP患者肝功能及妊娠结局的影响,现报道如下。
1 资料与方法
1.1 一般资料
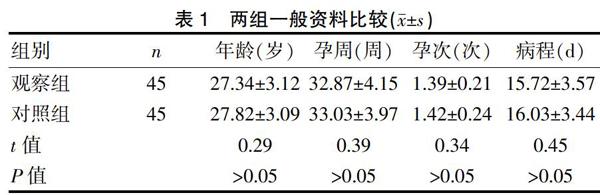
选取2012年1月~2018年4月我院妇产科住院治疗的ICP患者90例。纳入标准[7]:符合《妊娠期肝内胆汁淤积症诊疗指南》中的ICP诊断标准[8]。排除标准[9]:①存在妊娠期糖尿病、高血压等疾病者;②以往存在肝胆系统疾病者。采用随机数字表法将90例ICP患者分为观察组和对照组,各45例。两组患者的年龄、孕周、孕次和病程等情况比较,差异无统计学意义(P>0.05),具有可比性。见表1。
1.2 治疗方法
对照组均予以能量合剂[三磷腺苷针(福建古田药业有限公司,规格:20 mg/支,国药准字H35020101)40 mg,辅酶A针(天津生物化学制药有限公司,规格:100 U/支,国药准字H12020489)100 U,维生素C针(郑州卓峰制药有限公司,规格:0.5 g/支,国药准字H20044375)2.0 g]等常规治疗。观察组在对照组能量合剂治疗基础上加用熊去氧胆酸(Losan Pharma GmbH,规格:250 mg/片,国药准字H20100502)0.25 g/次,2次/d,口服,两组连用14 d。观察两组治疗前和治疗14 d后肝功能指标水平的变化,并比较其临床疗效及妊娠结局。
1.3 观察指标
1.3.1 血清肝功能测定 采集空腹静脉血约3~5 mL,离心取上清,低温保存备用,采用全自动生化分析仪测定肝功能指标,包括胆汁酸(Total bile acid,TBA)、谷丙转氨酶(Alanine transaminase,ALT)和谷草转氨酶(Aspartic transaminase,AST)。
1.3.2 妊娠結局 包括胎儿宫内窘迫、早产、产后出血和新生儿窒息等。
1.4 疗效评定标准[10]
显效:治疗后肝功能指标TBA、ALT和AST恢复正常,临床症状较前显著改善;有效:治疗后肝功能指标TBA、ALT和AST指标下降>50%,临床症状较前大改善;无效:未达上述标准。以显效和有效合计总有效。
1.5 统计学方法
采用SPSS18.0统计软件分析,计量资料以均数±标准差(x±s)表示,采用t检验,计数资料以率[n(%)]表示,采用χ2检验,以P<0.05为差异有统计学意义。
2 结果
2.1 两组治疗前后TBA、ALT和AST水平比较
治疗前两组TBA、ALT和AST水平比较差异无统计学意义(P>0.05)。治疗14 d后,两组血清TBA、ALT和AST水平均较前显著下降(P<0.01或P<0.05),且观察组明显低于对照组(P<0.05)。见表2。
2.2 两组治疗后效果比较
治疗14 d后,观察组临床总有效率较对照组更佳(χ2=4.54,P<0.05)。见表3。
2.3 两组妊娠结局比较
观察组不良妊娠结局发生率明显低于对照组(χ2=3.92,P<0.05)。见表4。
3 讨论
ICP是妊娠中晚期一种特有的严重影响母婴安全的并发症,其临床发病率约8%~12%,主要表现为皮肤瘙痒及黄疸,如不及时治疗易出现母体产后出血,胎儿宫内窘迫、早产和新生儿窒息等现象,需积极有效治疗[10-12]。ICP的病因及发病机制国内外尚无完全明确,可能与遗传易感性、雌孕激素水平异常、免疫功能失调、种族因素、环境污染及胆酸在体内大量积聚密切相关,尤其是与患者鹅去氧胆酸、去氧胆酸和石胆酸的大量积聚密切相关[13-15]。研究已证实ICP孕妇由于体内雌性激素水平升高,降低Na+-K+-ATP酶活性,抑制肝内胆红素代谢所需酶,导致胆酸代谢异常,胆汁流出受阻形成胆汁淤积,引起胆汁回流增加,胆汁黏稠度增加,使血中胆酸浓度增加并积蓄到皮下,刺激患者感觉神经末梢,产生皮肤瘙痒等临床症状。另外由于胆汁酸、胆红素水平急剧上升,大量沉积于胎膜绒毛膜板上,使胎盘绒毛间隙逐渐变窄,基质形成水肿增厚,降低胎盘的血流灌注,红细胞携氧量明显下降,氧气交换量减少,可引起胎儿宫内缺氧出现多种较严重的并发症,发生羊水污染、胎儿发育迟缓、宫内窘迫甚至形成死胎,不利于母婴结局与预后,是影响围生儿病死率的重要因素[16-17]。
熊去氧胆酸是一种双羟基胆汁酸,是治疗急慢性肝炎的常用的利胆药,主要由体内的鹅脱氧胆酸代谢生成,具有较强的亲和力及亲水性,通过竞争性抑制作用产生良好的保肝利胆作用[18-19]。熊去氧胆酸能抑制并拮抗水性胆汁酸的细胞毒性作用,有效降低胆汁酸的毒性,保护细胞和细胞膜,能干扰胆酸及鹅脱氧胆酸在小肠的吸收,抑制内源性胆汁酸的吸收,减少血胆酸水平,稳定肝细胞膜保护肝细胞;同时熊去氧胆酸还能减少线粒体和细胞膜通透性,抑制肝细胞凋亡,调节免疫功能而减少肝组织活化,从而保护肝细胞,有利于受损肝组织的修复,促进肝细胞再生,改善肝功能[20-21]。彭小燕等[22]研究发现熊去氧胆酸治疗ICP疗效良好,能促进患者肝胆功能的恢复,缓解患者肝功能,降低体内胆酸的水平,为胎儿营造良好环境,改善不良分娩结局。章杨韦等[5]研究亦发现熊去氧胆酸片可降低母体胆酸浓度,有效提高ICP患者围生期结局,降低胎儿死亡率。本研究示治疗14 d后,观察组血清TBA、ALT和AST水平[(21.09±4.03)μmol/L、(47.34±9.12)U/L、(51.72±9.85)U/L]和对照组血清TBA、ALT和AST水平[(35.13±7.47)μmol/L、(69.86±11.64)U/L、(78.17±12.60)U/L]均较前[(53.20±13.06)μmol/L、(92.36±14.28)U/L、(118.48±20.67)U/L、(52.78±12.34)μmol/L、(91.84±13.73)U/L、(116.39±19.84)U/L]显著下降(P<0.01或P<0.05),且观察组下降值大于对照组,且其临床总有效率(95.56%)较对照组(82.22%)更佳。提示熊去氧胆酸治疗ICP患者的临床效果确切,能降低AST、ALT、TBA等生化指标,显著改善肝功能指标;同时研究还发现观察组患者不良妊娠结局发生率明显低于对照组,提示熊去氧胆酸治疗ICP患者能降低不良妊娠结局。我们推测熊去氧胆酸治疗ICP可能通过抑制内源性胆汁酸的吸收、抑制肝细胞凋亡等途径保护肝细胞,修复受损肝组织,改善肝功能指标。随着肝功能的好转,胎盘的血流灌注逐渐增加,有利于降低不良妊娠结局。
总之,熊去氧胆酸治疗ICP患者的临床效果确切,能明显改善肝功能指标,降低不良妊娠结局,保护母婴安全。但本研究纳入的病例数偏少,实验的研究可能存在一定的误差,必要时增加病例数进行深入的研究探讨。
[参考文献]
[1] Sanhal CY,Kara O,Yucel A.Can fetal left ventricular modified myocardial performance index predict adverse perinatal outcomes in intrahepatic cholestasis of pregnancy?[J]. J Matern Fetal Neonatal Med,2016,17(1):1-22.
[2] Kularatnam GAM,Warawitage HD,Vidanapathirana DM,et al. Correction to:Dubin-Johnson syndrome and intrahepatic cholestasis of pregnancy in a Sri Lankan family:A case report[J]. BMC Res Notes,2017,10(1):492.
[3] Ekiz A,Kaya B,Avci ME,et al. Alanine aminotransferase as a redictor of adverse perinatal outcomes in women with intrahepatic cholestasis of pregnancy[J]. Pak J Med Sci,2016,32(2):418-422.
[4] Covach AJ,Rose WN. Intrahepatic cholestasis of pregnancy refractory to multiple medical therapies and plasmapheresis[J]. AJP Rep,2017,7(4):e223-e225.
[5] 章杨韦,丁其培,王琛琛. 熊去氧胆酸治疗妊娠期肝内胆汁淤积症的疗效及对妊娠结局的影响[J]. 中国妇幼保健,2017,32(21):5242-5244.
[6] 宋倩倩. 熊去氧胆酸改善妊娠期肝内胆汁淤积症患者妊娠结局的Meta分析[J]. 中国现代应用药学,2016, 33(11):1468-1473.
[7] 庄小平. 丁二磺酸腺苷蛋氨酸肠溶片对妊娠期肝内胆汁淤积症重症患者瘙痒程度、妊娠结局及肝功能的影响[J]. 肝脏,2017,22(3):229-231.
[8] 中華医学会妇产科学分会产科学组. 妊娠期肝内胆汁淤积症诊疗指南(第1版)[J]. 中华妇产科杂志,2011, 46(5):391-395.
[9] 朱瑜,黄小萍,谢涵. 丁二磺酸腺苷蛋氨酸联合熊去氧胆酸治疗妊娠期肝内胆汁淤积症40 例[J]. 医药导报,2015,34(8):1040-1043.
[10] Abu-Hayyeh S,Ovadia C,Lieu T,et al. Prognostic and mechanistic potential of progesterone sulfates in intrahepatic cholestasis of pregnancy and pruritus gravidarum[J].Hepatology,2016,63(4):1287-1298.
[11] Zhang Y,Pan Y,Lin C,et al. Bile acids evoke placental inflammation by activating Gpbar1/NF-κB pathway in intrahepatic cholestasis of pregnancy[J]. J Mol Cell Biol,2016,8(6):530-541.
[12] Wensink MJ. The risk of infant and fetal death by each additional week of expectant management in intrahepatic cholestasis of pregnancy by gestational age:Various objections [J]. Am J Obstet Gynecol,2016,215(6):807-808.
[13] Keitel V,DroGe C,Stepanow S,et al. Intrahepatic cholestasis of pregnancy(ICP):Case report and review of the literature[J]. Zeitschrift für Gastroenterologie,2016,54(12):1327-1333.
[14] Kurtulmu S,Gür EB,Kztekin D,et al. The impact of intrahepatic cholestasis of pregnancy on fetal cardiac and peripheral circulation[J]. J Turk Ger Gynecol Assoc,2015,16(2):74-79.
[15] Liu X,Landon MB,Chen Y,et al. Perinatal outcomes with intrahepatic cholestasis of pregnancy in twin pregnancies[J]. J Matern Fetal Neonatal Med,2016,29(13):2176-2181.
[16] 杜巧玲,段涛. 胆汁酸与妊娠期肝内胆汁淤积症发病机制关系的研究进展[J]. 中华妇产科杂志,2013,48(2):141-143.
[17] Bull LN,Hu D,Shah S,et al. Intrahepatic cholestasis of pregnancy (ICP) in U.S. latinas and chileans:Clinical features,ancestry analysis,and admixture mapping[J]. PLoS One,2015,10(6):e0131211.
[18] 孙雪梅,田鹏. 熊去氧胆酸治疗妊娠期肝内胆汁淤积症及对脐静脉血总胆汁酸等的影响[J]. 中国生化药物杂志,2015,35(8):81-83.
[19] 游玉琼. 熊去氧胆酸联合低分子肝素治疗妊娠期肝内胆汁淤积症的疗效评价[J]. 实用妇科内分泌电子杂志,2017,4(9):59.
[20] 曹杰,蔡艾杞,田立碧,等. 熊去氧胆酸、腺苷蛋氨酸联合多烯磷脂酰胆碱对妊娠期肝内胆汁淤积症患者相关指标的影响[J]. 中国药房,2017,28(18):2509-2511.
[21] 赵丹阳. 熊去氧胆酸与多烯磷脂酰胆碱治疗对妊娠期肝内胆汁淤积症患者妊娠结局及胎儿并发症的影响[J]. 中国妇幼保健,2017,32(18):4380-4382.
[22] 彭小燕. 熊去氧胆酸对妊娠期肝内胆汁淤积症患者分娩结局的影响[J]. 实用妇科内分泌杂志,2017,4(2):98-99.
(收稿日期:2018-12-04)
