Value of pretransplant albumin-bilirubin score in predicting outcomes after liver transplantation
2019-05-08TaoMaQingShanLiYueWangBoWangZhengWuYiLvRongQianWu
Tao Ma, Qing-Shan Li, Yue Wang, Bo Wang, Zheng Wu, Yi Lv, Rong-Qian Wu
Abstrac t BACKGROUND Due to the significant shortage of organs and the increasing number of candidates on the transplant waiting list, there is an urgent need to identify patients who are most likely to benefit from liver transplantation. The albuminbilirubin (ALBI) grading system was recently developed to identify patients at risk for adverse outcomes after hepatectomy. However, the value of the pretransplant ALBI score in predicting outcomes after liver transplantation has not been assessed.AIM To retrospectively investigate the value of the pretransplant ALBI score in predicting outcomes after liver transplantation.METHODS The clinical data of 272 consecutive adult patients who received donation after cardiac death and underwent liver transplantation at our centre from March 2012 to March 2017 were analysed in the cohort study. After the exclusion of patients who met any of the exclusion criteria, 258 patients remained. The performance of the ALBI score in predicting overall survival and postoperative complications after liver transplantation was evaluated. The optimal cut-off value of preoperative ALBI was calculated according to long-term survival status. The outcomes after liver transplantation, including postoperative complications and survival analysis, were measured.RESULTS The remaining 258 consecutive patients were included in the analysis. The median follow-up time was 17.30 (interquartile range: 8.90-28.98) mo. Death occurred in 35 patients during follow-up. The overall survival rate was 81.0%.The preoperative ALBI score had a significant positive correlation with the overall survival rate after liver transplantation. The calculated cut-off for ALBI scores to predict postoperative survival was -1.48. Patients with an ALBI score > -1.48 had a significantly lower survival rate than those with an ALBI score ≤ -1.48(73.7% vs 87.6%, P < 0.05), and there were no statistically significant differences in survival rates between patients with a model for end stage liver disease score ≥ 10 and < 10 and different Child-Pugh grades. In terms of the specific complications,a high ALBI score was associated with an increased incidence of biliary complications, intraabdominal bleeding, septicaemia, and acute kidney injury after liver transplantation (P < 0.05 for all).CONCLUSION The ALBI score predicts overall survival and postoperative complications after liver transplantation. The ALBI grading system may be useful in risk-stratifying patients on the liver transplant waiting list.
Key words: Albumin-bilirubin score; Liver transplantation; Survival; Postoperative complications; Liver transplant waiting list
INTRODUCTION
Ad vances in immunosup p ression and imp rovements in surgical techniques and p eriop erative care have marked ly imp roved the outcome of liver transp lant recipients, and liver transplantation (LT) has become the only effective treatment for patients with end-stage liver disease[1-3]. Because of the significant shortage of organs and the increasing number of cand id ates on the transplant w aiting list, there is an urgent need to identify patients who are most likely to benefit from LT[2,4,5].
The albumin-bilirubin (ALBI) score, as a simple assessment of liver function, is objectively calculated by only tw o variables (albumin and bilirubin)[6]. It was recently proposed by Johnson et al[6], And reatos et al[7], and Zou et al[8]as a new method for preop erative risk evaluation to d iscern patients w ith the risk of adverse outcomes after hepatectomy. While the ALBI grad ing system has been closely related to inhospital mortality in patients w ith chronic liver disease, its value to predict outcomes after LT has not been evaluated. Therefore, the purpose of this study was to explore the ability of the pretransplant ALBI score to predict outcomes after LT.
MATERIALS AND METHODS
Data source and patient population
This single-centre, retrospective cohort study w as conducted to investigate the relationship between pretransplant ALBI scores and outcomes after LT. From March 1, 2012 to March 31, 2017, 272 consecutive adult patients (age > 18 years) with endstage liver disease who received donation after cardiac death (DCD) and underwent LT at the First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China were included in this stud y. All clinical variables of these 272 patients, includ ing demographic features and preoperative, intraoperative, and postoperative data, were obtained from a computerized clinical database from the hospital. In addition to the date of this study, available medical records, including follow-up data, met the inclusion criteria. This study was approved by the First Affiliated Hospital of Xi'an Jiaotong University Ethics Committee. Written informed consent from the patients was waived due to the retrospective nature of this study. All cases received follow-up care routinely until June 2017.
Definitions
The ALBI score was calculated using the formula: (log10bilirubin × 0.66) + (albumin ×-0.085), where bilirubin is measured in μmol/L and albumin in g/L[6]. The primary outcome was overall survival. The secondary outcomes included total complications and the incidence of biliary comp lications, portal vein thrombosis, rejection,pneumonia, acute kidney injury (AKI), intraabdominal bleeding, and in-hospital mortality as well as length of postoperative hospital stay after LT.
Statistical analysis
To minimize bias, follow-up s and review s w ere comp leted by tw o clinicians.Categorical variables are reported as numbers and percentages and w ere compared by a chi-squared analysis or Fisher's exact test as appropriate. Normal and abnormal continuous variables are reported as the mean ± standard deviation (SD) and median[interquartile range (IQR)], and w ere compared by Student's t-test and the Mann-Whitney rank-sum test, respectively. The optimal cut-off value of preoperative ALBI was calculated by receiver operating characteristic (ROC) curve analysis and utilizing the Youden ind ex according to long-term survival status. The accuracy of ALBI for predicting outcomes was evaluated using the area under the ROC curve (AUC). The survival rates of recip ients w ith high ALBI grad es and low ALBI grad es w ere compared using a Kap lan-Meier estimation and a log-rank test. Univariate and multivariate analyses of p rognostic factors w ere p erformed using the Cox proportional hazards model. All statistical tests were tw o-sided, and P-values < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS Statistics 22.0 softw are (IBM Corporation, Armonk, NY, United States).
RESULTS
Patient demographics
A total of 272 patients underwent LT at our hospital from March 1, 2012 to March 31,2017. Of these patients, 14 were exclud ed from this study: 12 were lost to follow-up and 2 w ere missing criteria for ALBI and mod el for end stage liver d isease (MELD)score calculations. The remaining 258 consecutive p atients w ere includ ed in the analysis. The med ian follow-up time w as 17.30 (IQR: 8.90-28.98) mo. Table 1 show s the demographics and baseline characteristics of these patients. Of these patients, 206 were male (79.8%), and 52 w ere female (20.2%). The med ian age of the patients w as 47.0 (IQR: 39.0-56.0) years. The ind ications for LT w ere hep atocellular carcinoma(HCC) (33.7%), viral hepatitis-related cirrhosis (77.5%), alcoholic cirrhosis (3.1%),primary biliary cirrhosis and autoimmune hepatitis (8.2%), and others (11.2%), such as hepatolenticular degeneration, cryptogenic cirrhosis, drug-induced liver injury, upper biliary tract obstruction, and acute liver failure. The median preoperative ALBI score and MELD score w ere -1.78 (-2.40 to -1.33) and 15.5 (11.0-23.0), respectively. Death occurred in 35 patients during follow-up. The overall survival rate was 81.0%.
Predictive value of pretransplant ALBI for overall survival after LT
The performance of the ROC curve analysis w as d etermined by the value of the pretransplant ALBI score to pred ict the overall survival after LT. Figure 1 show s that the pretransplant ALBI score had a significant positive relationship w ith the overall survival rate. The AUC w as 0.647 w ith a 95% confidence interval (CI) of 0.540-0.753 and a P-value of 0.005. The cut-off for ALBI scores w as calculated as -1.48 by predicting postoperative survival, with a Youd en index of 0.304 (sensitivity = 60.0%,and specificity = 70.4%). Based on the cut-off value, 173 patients had a low ALBI score(ALBI ≤ -1.48, 67.1%) and 85 patients had a high ALBI score (ALBI > -1.48, 32.9%). As shown in Table 2, the pretransplant and demographic data were related to the ALBI grade. There was less likely to be HCC in patients with high ALBI scores than in patients with low ALBI scores. Patients in the high ALBI group also had higher preoperative MELD scores and higher Child-Pugh (C-P) grades. In terms of the preoperative laboratory values, patients in the high ALBI group had higher values for aspartate transaminase (AST), alpha-fetoprotein (ALT), total bilirubin (TBIL), direct bilirubin (DBIL), neutrophil granulocytes (NEUT), monocytes (MONO), prothrombin time (PT), activated partial thromboplastin time (APTT), and international normalized ratio (INR) (P < 0.05 for all) but lower levels of red blood cells (RBC), haemoglobin(HGB), platelets (PLT), albumin (ALB), and alpha-fetoprotein (AFP) (P < 0.05 for all).The 3-year survival after LT was analysed based on pretransplant ALBI scores using the Kaplan-Meier estimation. As shown in Figure 2, patients with high ALBI scores had a significantly lower survival rate than patients with low ALBI scores (73.7% vs 87.6%, P < 0.05). However, there were no statistically significant differences in 3-year survival rates betw een patients w ith MELD scores ≥ 10 and < 10 (Figure 3A).Similarly, no statistically significant differences were found in 3-year survival rates among patients with different C-P grades (Figure 3B). Univariable and multivariable analyses were performed to identify independent risk factors related to poor survival after LT. Univariate variables with P < 0.1 were included in the multivariate analysis.Table 3 shows that high pretransplant ALBI scores, high PLT, high serum levels of creatinine, and high APTT were independently associated with poor survival after LT in the multivariate analysis.
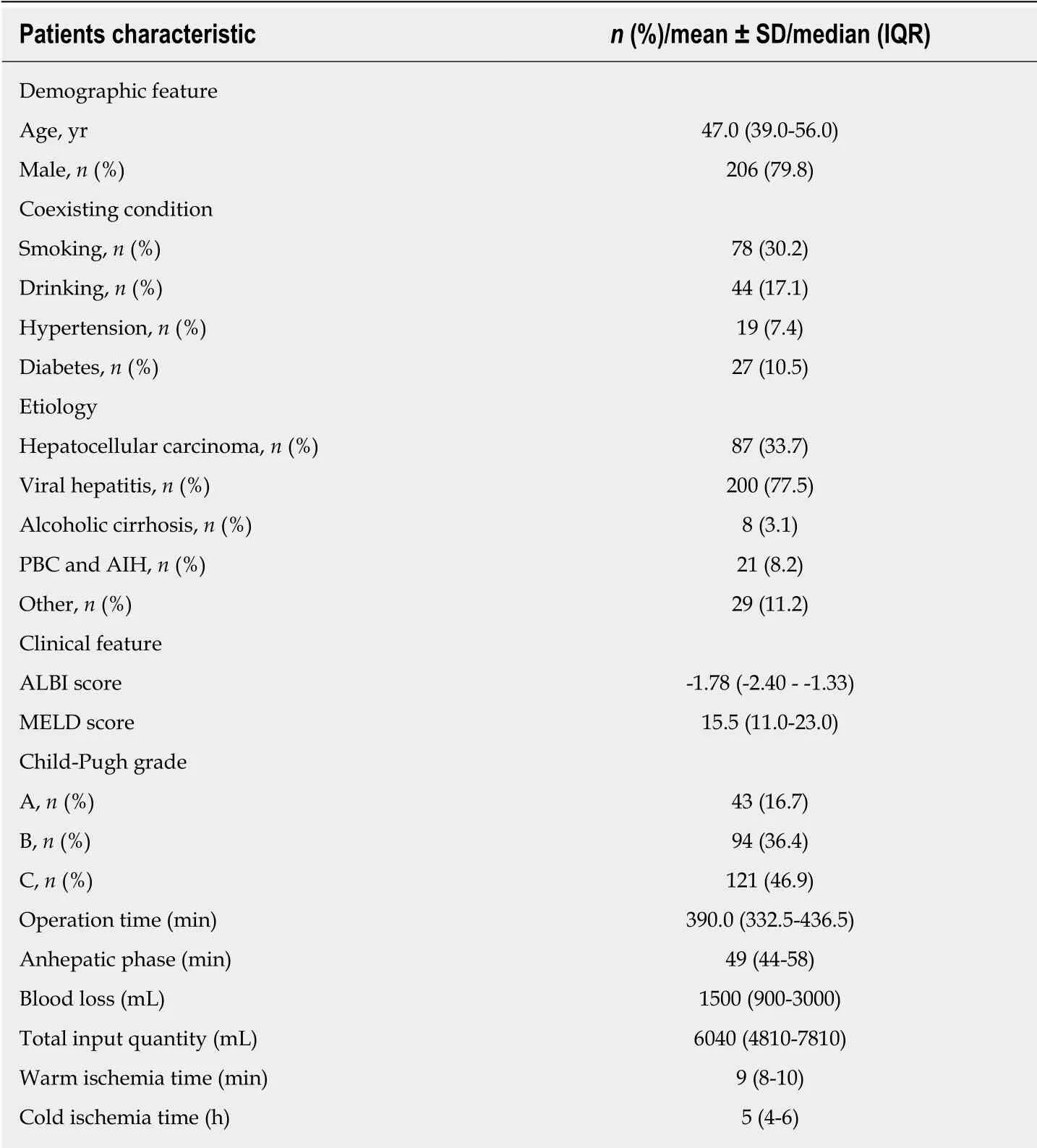
Table 1 Patient demographics (n = 258)
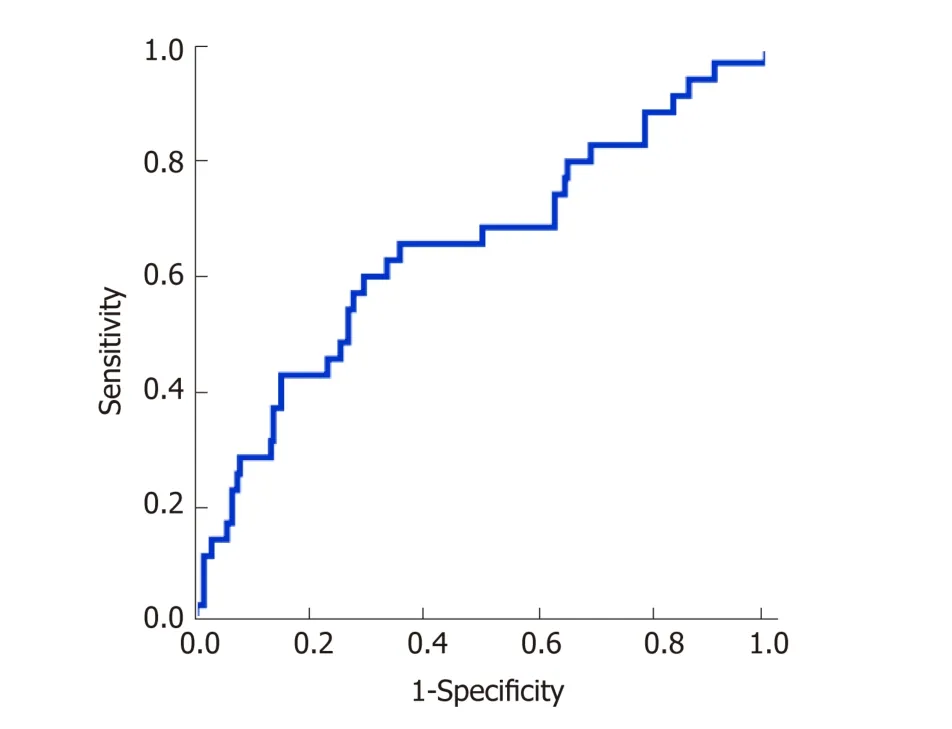
Figure 1 Determination of optimal albumin-bilirubin cut-off value by receiver operating characteristic analysis. The calculated cut-off for albumin-bilirubin scores to predict postoperative survival was -1.48, according to an area under a receiver operating characteristic curve of 0.647 (P = 0.005).
Pretransplant ALBI and postoperative complications
Table 4 shows postoperative complications stratified by pretransplant ALBI scores. A total of 189 patients developed various postoperative complications according to the Clavien-Dindo system[9]; 87.06% of patients in the high ALBI score group (74 out of 85)developed postoperative complications after LT, while only 66.47% of patients in the low ALBI score group (115 out of 173) did. The difference was statistically significant(P < 0.05), which was also reflected in the comprehensive complication index (CCI). In terms of specific complications, a high ALBI score was associated with an increased incidence of biliary complications, intraabdominal bleeding, septicaemia, and AKI (P< 0.05 for all). However, no significant differences w ere found between the tw o groups for other complications.
DISCUSSION
The prediction of prognosis is an important part of management in patients with endstage liver d isease. Our current d ata show that the ALBI score, a simp le mod el incorporating only serum bilirubin and serum albumin levels, performed better than the conventional MELD mod el in p red icting overall survival and p ostop erative complications after LT. Assessment of liver function is particularly important for patients on the liver-transplant w aiting list. Since both serum bilirubin and albumin are part of the commonly used liver function tests, the ALBI score is readily available.In this study, w e found that the optimal ALBI cut-off value was -1.48, analysed by the ROC curve to predict survival after LT, which is very close to the cut-off value (-1.39)betw een ALBI grad e 2 and grad e 3[6,10]. In fact, by using the cut-off value of the reported ALBI grad ing system developed for hepatectomy (i.e., -1.39)[6,7,11], w e found that patients in the ALBI grade 3 classification had significantly higher mortality and more adverse postoperative outcomes after LT than patients in the ABLI grade 1 or 2(data not show n) classifications, indicating that the reported ALBI grading system is also relevant in LT. Although many studies have shown that the ALBI grading system is a useful tool to identify patients at risk for adverse outcomes after hepatectomy, as far as we know, the present study is the first to assess the value of the pretransplant ALBI score in predicting outcomes after LT.
Assessment of preop erative liver function is vital to d etermine liver functional reserve in patients w ith end stage liver disease. The MELD system w as developed in 2002 to prioritize patients waiting for LT[12]. As a numerical scale, MELD w as used for adult LT candid ates[13-15]. The patient's urgency for LT w ithin the next three months was determined by personal MELD scores[16]. The MELD scoring system contains tw o variables for hepatic (dys)function (i.e., total bilirubin and INR) and one variable for renal (dys)function (i.e., creatinine). Although subsequent studies have show n poor outcomes for liver transplant recipients w ith high MELD scores, its overall capacity to predict posttransplant outcomes is limited[12,16,17].
In the current study, although w e found that patients w ith an MELD score < 10 seemed to have slightly higher survival rates than patients with an MELD score ≥ 10,there w ere no statistically significant d ifferences in either the univariable or multivariable analyses. These results clearly show that the performance of ALBI isbetter than MELD in predicting outcomes after LT.
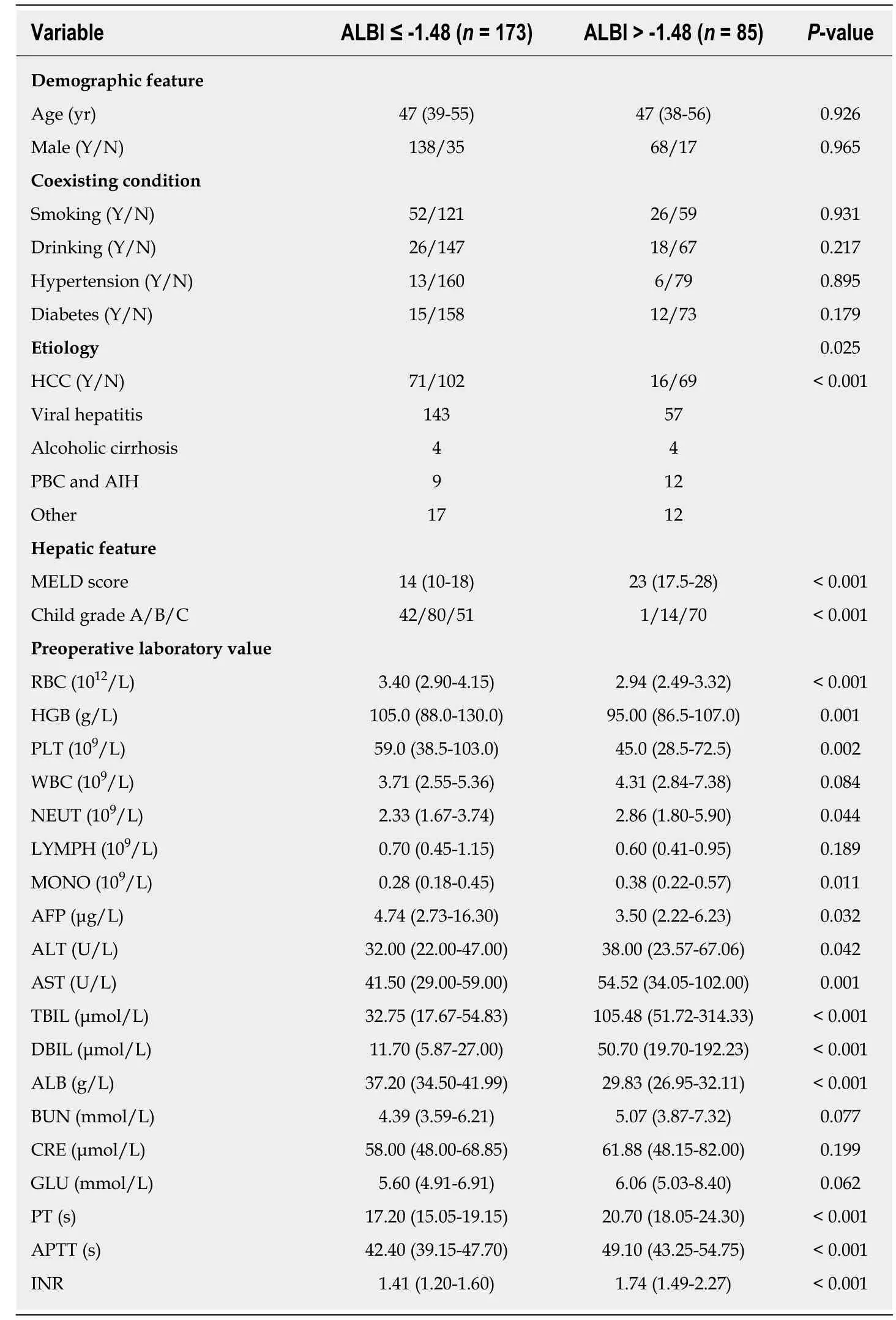
Table 2 Baseline comparison between patients with different albumin-bilirubin grades
Another mod el to assess liver function is the C-P system. The C-P grad e is determined by five variables, includ ing TBIL, ALB, PT, and d egree of ascites and hepatic encephalopathy. The C-P system w as developed arbitrarily several decad es ago based on clinical observation without proper statistical evidence. Although the CP system is w id ely used, there are many limitations for its implementation[18,19]. For instance, the grading of ascites and hepatic encephalopathy is highly subjective[15,18,20].It is not clear to identify the grad e of ascites and hepatic encephalopathy according to guidelines. Some of the parameters, such as serum albumin levels and the extent of ascites, are interrelated. More importantly, the C-P grade failed to show any value in discriminating both survival and complications after LT in our current study.
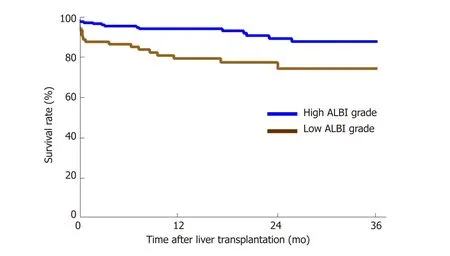
Figure 2 Kaplan-Meier estimation of 3-year survival according to albumin-bilirubin grade. Patients with a high albumin-bilirubin (ALBI) grade (> -1.48) had a significantly lower survival rate of 73.7% than patients with a low ALBI score (ALBI ≤ -1.48) of 87.6% (P < 0.05). ALBI: Albumin-bilirubin.
Of course, there w ere still some limitations in the stud y. First, this current study only included population data from one transplant centre; based on the LT data of the single centre, the posttransplant morbidity and mortality w ere low in the relatively small sample. For examp le, a relatively small prop ortion of p atients d ied d uring follow-up, w hich may have limited the robustness of the multivariable analysis for ad justment for confounding factors. Second, only patients w ho received d onation after DCD w ere includ ed in the stud y; the value of ABLI scores in p red icting outcomes of patients w ho received d onation after brain d eath needs to be further investigated. Third, as the median follow-up time in the current study was only 17.30 mo, w e w ere unable to comment on the effect of pretransplant ALBI scores on longer term outcomes of patients. Additionally, the study aimed to explore the effect of ALBI scores on overall survival, not on liver death related to liver disease (i.e., disease-free survival)[21]. The d ifficulty of sp ecifically attributing the reason for d eath after transplantation in the clinic makes no difference in terms of the p atients' outcomes.Lastly, as the nature of this stud y w as retrosp ective, the results are subject to a selection bias and some resid ual confound ing d ue to unmeasured or unknow n confounders.
In summary, the d ata reveal that the ALBI score may be better than the MELD score for risk stratification of LT patients. Ap p roximately one-third of our stud y population w as categorized as having a high ALBI score (> -1.48); therefore, the ALBI scoring system is clinically relevant. In addition, the ALBI grad ing system may be a more readily applicable means to model risk among patients undergoing LT because it relies on few er variables. The id entification of p atients w ho are most likely to benefit from LT remains a remarkable challenge[22].
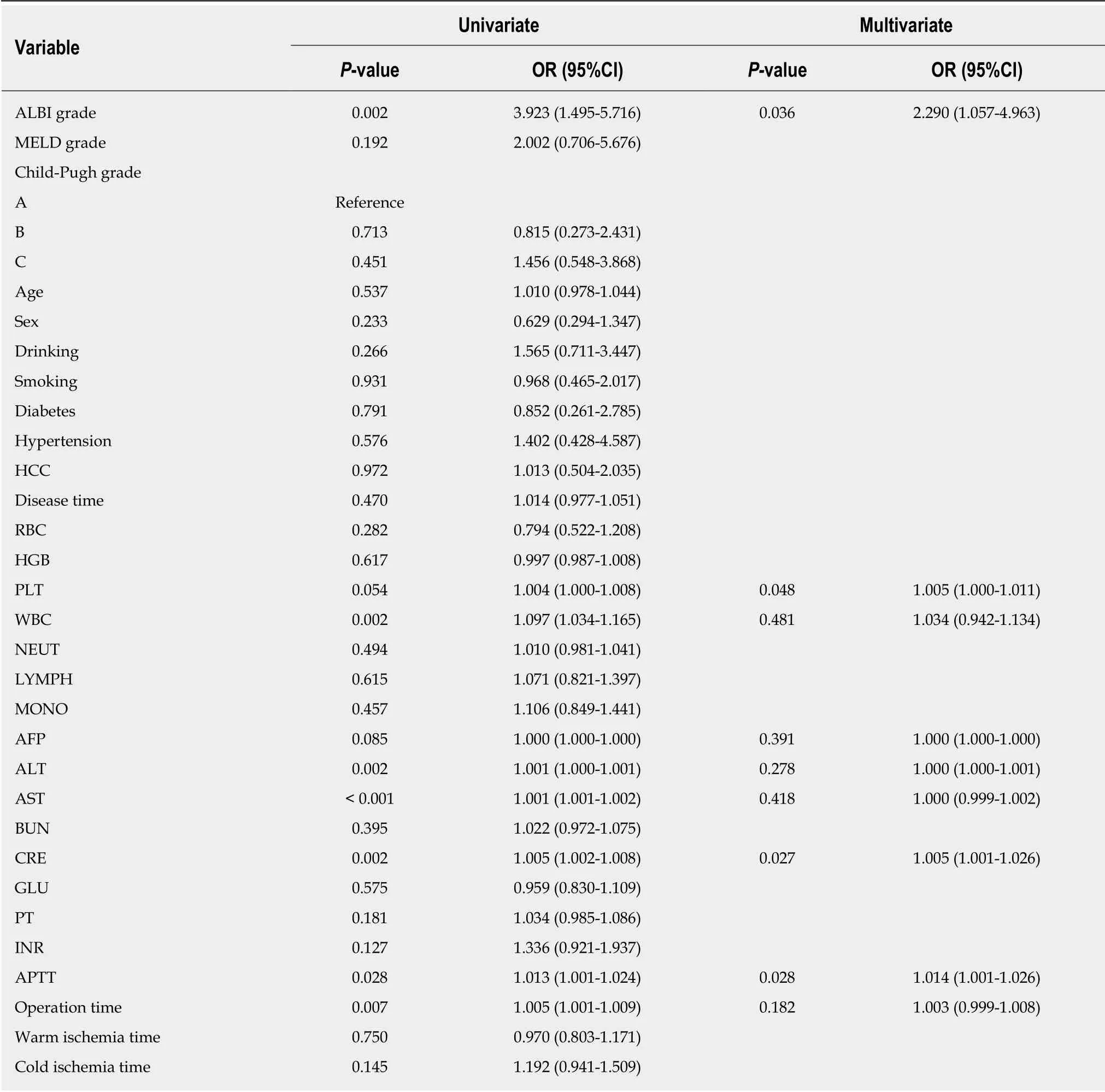
Table 3 Univariate and multivariate logistic regression analysis of overall survival
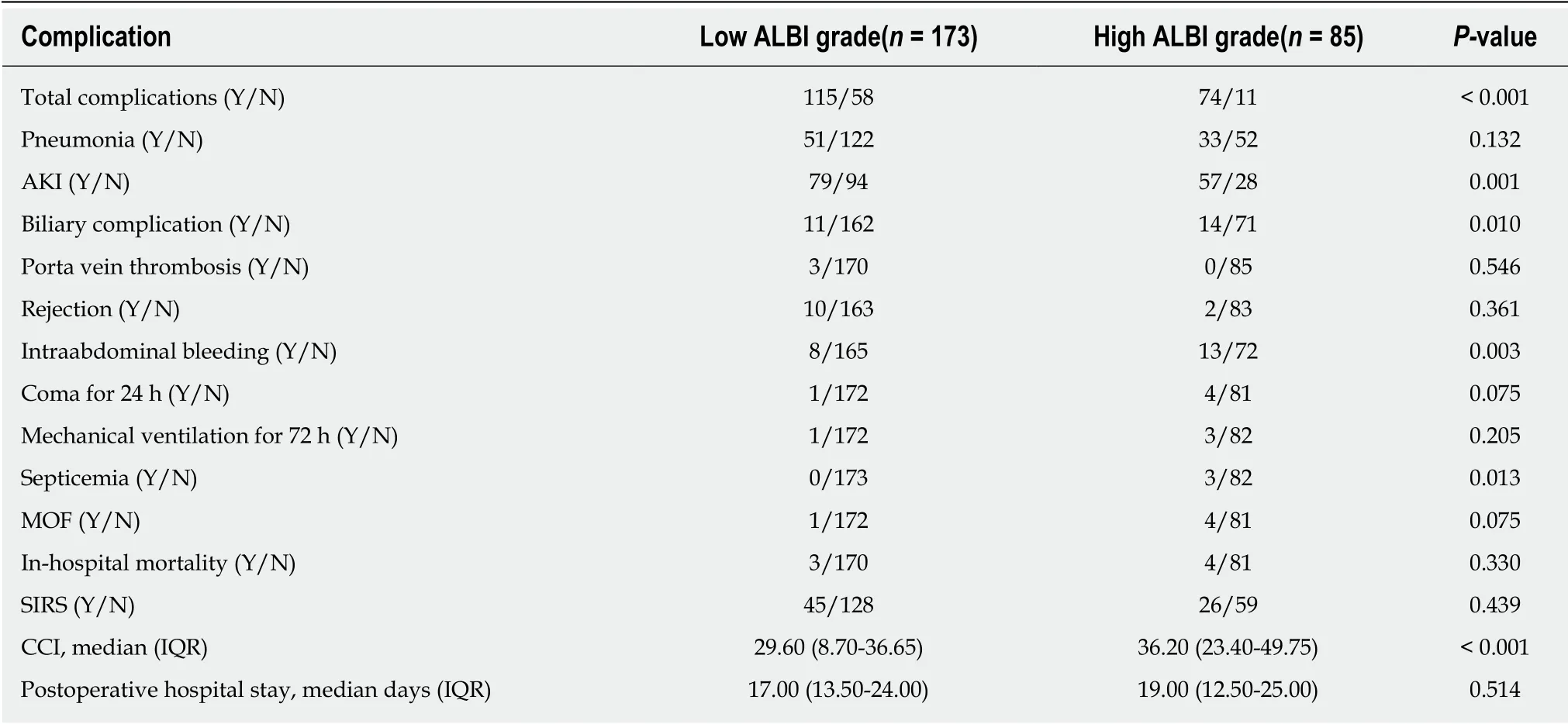
Table 4 Postoperative complications according to albumin-bilirubin grade
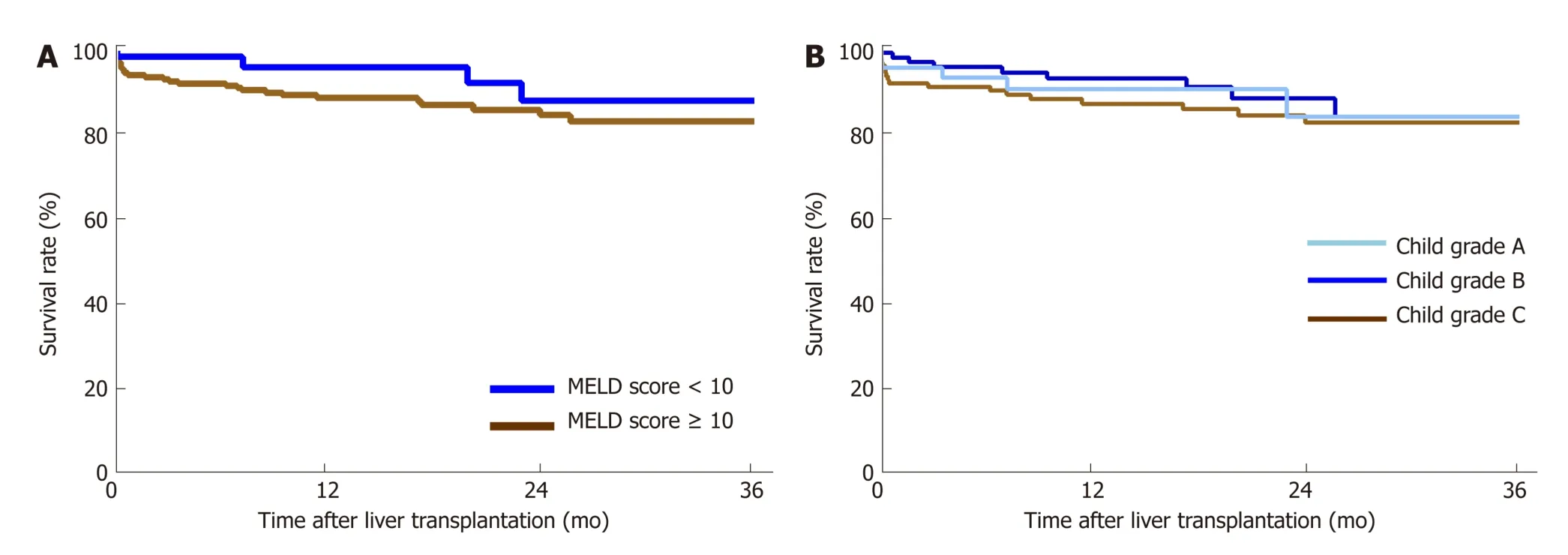
Figure 3 Kaplan-Meier estimation of 3-year survival according to model for end stage liver disease score. A: The 3-year survival rates between patients with a model for end stage liver disease score ≥ 10 and < 10 were 81.3% and 84.9%, respectively (P > 0.05). B: There were no statistically significant differences in 3-year survival rates among patients with different Child-Pugh grades (P > 0.05). MELD: Model for end stage liver disease.
ARTICLE HIGHLIGHTS
Research background
The albumin-bilirubin (ALBI) score, as a simple assessment of liver function, is objectively calculated by only two variables (albumin and bilirubin). It was proposed as a new method for preoperative risk evaluation to discern patients with the risk of adverse outcomes after hepatectomy. However, its ability to predict outcomes after liver transplantation has not been evaluated. Because of the significant shortage of organs and the increasing number of candidates on the transplant waiting list, there is an urgent need to identify patients who are most likely to benefit from LT.
Research motivation
The main topic of this study was to provide a potential scoring system for the allocation of donor liver resources by investigating the relationship between pretransplant ALBI score and outcomes after liver transplantation.
Research objectives
To retrospectively investigate the value of pretransplant ALBI scores in predicting outcomes after liver transplantation and as a tool for risk-stratifying patients on the liver transplant waiting list.
Research methods
The research data were obtained from a computerized clinical database from the First Affiliated Hospital of Xi'an Jiaotong University and included 258 consecutive patients w ho received donation after cardiac death (DCD) and underwent liver transplantation from March 2012 to March 2017. The optimal cut-off value of preoperative ALBI was calculated according to longterm survival status. The performance of the ALBI score in predicting outcomes, including postoperative complications and survival analysis, was measured and evaluated.
Research results
This study analysed data from 258 patients. Thirty-five patients died during follow-up [17.30(interquartile range: 8.90-28.98) mo], w ith an overall survival rate of 81.0%. The optimal cut-off value of preoperative ALBI scores to predict postoperative survival w as -1.48. Patients w ith an ALBI score > -1.48 had a significantly low er survival rate than those w ith an ALBI score ≤ -1.48(73.7% vs 87.6%, P < 0.05), and there w ere no statistically significant differences in survival rates betw een patients w ith a model for end stage liver disease (MELD) score ≥ 10 and < 10 and different Child-Pugh grades. Moreover, a high ALBI score w as associated w ith an increased incidence of biliary complications, intraabdominal bleeding, septicaemia, and acute kid ney injury after liver transplantation (P < 0.05 for all). Of course, this study only initially confirmed the predictive value of the ALBI score for liver transplantation outcomes. The predictive value of multi-centre data resources and other donations, except after DCD, need to be further researched and confirmed.
Research conclusions
After the ALBI grading system w as developed to identify patients at risk for adverse outcomes after hepatectomy, this study hypothesized that this score may also be valuable in evaluating outcomes after liver transp lantation. The ALBI score p red icted overall survival and postoperative complications after liver transplantation. These data suggest that ALBI may be superior to MELD in risk-stratifying liver transplantation patients. In addition, ALBI may be a more readily applicable tool for modelling risk among patients undergoing liver transplantation because it relies on few er variables.
Research perspectives
The ALBI grading system may be useful in risk-stratifying patients on the liver transplant w aiting list. Multi-centre and prospective studies are needed to confirm our findings.
ACKNOWLEDGEMENTS
The authors thank all members of the Liver Transplantation Unit for their contributions to this valuable resource.
杂志排行
World Journal of Gastroenterology的其它文章
- Repurposing drugs to target nonalcoholic steatohepatitis
- Central role of Yes-associated protein and WW-domain-containing transcriptional co-activator with PDZ-binding motif in pancreatic cancer development
- Considerations of elderly factors to manage the complication of liver cirrhosis in elderly patients
- Lysyl oxidase and hypoxia-inducible factor 1α: biomarkers of gastric cancer
- Predictive and prognostic implications of 4E-BP1, Beclin-1, and LC3 for cetuximab treatment combined with chemotherapy in advanced colorectal cancer with wild-type KRAS: Analysis from real-world data
- Extract of Cycas revoluta Thunb. enhances the inhibitory effect of 5-f luorouracil on gastric cancer cells through the AKT-mTOR pathway
