Considerations of elderly factors to manage the complication of liver cirrhosis in elderly patients
2019-05-08KenyaKamimuraAkiraSakamakiHiroteruKamimuraToruSetsuTakeshiYokooMasaakiTakamuraShujiTerai
Kenya Kamimura, Akira Sakamaki, Hiroteru Kamimura, Toru Setsu, Takeshi Yokoo, Masaaki Takamura,Shuji Terai
Abstrac t The aging of the organ function causes sensitivity to the disease progression and need careful consideration for the medical treatment. With the increase of aging population, the opportunity to provide medical treatment for people in very old age is rapidly increasing therefore, the understanding of the various physiological changes of cellular function, size and function of organs are essential for the decision of therapeutic options. Among the various chronic conditions seen in elderly people, we have focused on liver cirrhosis, since despite specific therapeutic options for many of liver diseases including direct acting antivirals for hepatitis C virus, nucleoside analogs for hepatitis B, and corticosteroids for autoimmune hepatitis, there is currently no standard therapy to treat liver cirrhosis, which is the final stage of these liver diseases. Therefore,management of the various symptoms of liver cirrhosis is essential, and agingrelated parameters must be considered in the decision making for therapeutic strategies and dosage of the available medicine. In this mini-review, we have summarized the therapeutic options to manage various symptoms of liver cirrhosis, carefully considering the physiological changes of various organs associated with aging.
Key words: Liver cirrhosis; Elderly patients; Quality of life; Aging
INTRODUCTION
The increasing aging p opulation is a w orld w id e issue[1], and societies are facing various problems including long-term care for populations w ith a high prevalence of chronic cond itions[2]. Previous studies have demonstrated that aging w ell requires activities of daily living[3]and appropriate care for elderly patients[4,5]. Therefore, these crucial factors need to be consid ered to und erstand the features of p hysiological changes w hen consid ering therap eutic op tions for chronic d iseases[5-7]d ue to the imp act of aging on cellular function, size and function of organs, and vascular cognitive impairment and dementia[8].
Among the various chronic conditions seen in eld erly people, w e have focused on liver cirrhosis, as liver d isease is a major issue as its symptoms vary and there are various consid erations involved in the treatment of these patients. The general management guid elines have been published for the any age[9], however, due to the physiological changes in the organs and body, special considerations are essential for the elderly patients.
Morphological and functional aging of the liver includes reduced liver w eight and blood flow in the liver[10,11]due to decreased cardiac output[12], decreased number of hep atocytes[13], loss of metabolic function, and loss of d etoxification in the liver.Ginsberg et al. reported that the total volume of cytochrome p450 decreases to 70% of its original level in peop le > 70 years old, resulting in d ecreased metabolism and d etoxification in the liver[14]. These age-related changes in p harmacokinetics are correlated w ith a d ecrease in renal function[15]and should be consid ered w hen ad ministering med icines to elderly p atients[16]. It w as rep orted that grow th factor expression decreases with aging; therefore, elderly patients have difficulties tolerating liver injury[17,18]. The etiologies of liver d iseases includ e viral hep atic d iseases,autoimmune hep atic d iseases, alcoholic liver d iseases, and non-alcoholic steatohep atitis. Desp ite sp ecific therap eutic op tions for many of these d iseases including direct acting antivirals for hepatitis C virus, nucleoside analogs for hepatitis B, corticosteroids for autoimmune hepatitis, ursodeoxycholic acid for primary biliary cholangitis, stopping of alcohol for alcoholic hepatitis, control of body weight, vitamin E, pioglitazone, peroxisome proliferator-activator recep tor agonists, farnesoid X recep tor, and glucagon-like p ep tid e for non-alcoholic steatohep atitis, there is currently no standard therapy to treat liver cirrhosis, w hich is the final stage of these liver d iseases and may be complicated w ith hepatocellular carcinoma. Therefore,management of the various symptoms of liver cirrhosis is essential, and aging-related parameters must be considered in the decision making for therapeutic strategies and d osage of the available med icine. In this mini-review, w e have summarized the therap eutic op tions to manage various symp toms of liver cirrhosis, carefully considering the physiological changes associated w ith aging.
Japan has the oldest population in the w orld and has one of the most advanced a g i n g s o c i e t i e s(https://w w w.mhlw.go.jp/english/d atabase/d b-hw/lifetb16/ind ex.html)., w ith 35.215 million (27.8%) people aged ≥ 65 years, and more than 10 million (7.9%) people over 80. One in 10 w omen in the country is over 81, and the number of people > 65 years is also grow ing (http s://w w w.stat.go.jp/english/d ata/kokusei/2015/summary.html). Under these circumstances, defining the eld erly as those aged ≥ 65 years does not seem appropriate, and the distinction of categories of old, old-old, and oldest old is under d iscussion w orldw ide[1]. In Jap an, there are 5.5 million elderly people aged ≥ 85 y ears, accounting for ju st u nd er 5% of the total p op u lation(https://w w w.mhlw.go.jp/english/database/db-hw/lifetb16/ind ex.html), and the op p ortunity to provid e med ical treatment for p eople in very old age is rap id ly increasing.
It is clear that management of hepatitis and cirrhosis is imp ortant to maintain hep atic function as w ell as activities of d aily living and quality of life (QoL) of patients. While direct acting antiviral drugs have mad e it possible to control chronic hep atitis C infection, it is imp ortant to und erstand the changing characteristics of d iseases in the eld erly, as w ell as continuously increasing lifestyle d iseases and associated non-alcoholic steatohepatitis that leads to liver cirrhosis and liver cancer, in ord er to fully understand the d isease concept and select the appropriate treatment methods. Furthermore, various complications of liver cirrhosis, such as liver cancer and gastrointestinal tract bleeding, affect QoL in the elderly. As there have been no literatures focusing on these problems, w e have summarized the main p oints that must be considered in the management of current liver cirrhosis treatment in eld erly patients.
LIVER CIRRHOSIS IN ELDERLY PATIENTS
It is clear that the removal of etiological factors, if possible, is the most important part to prevent the progression of liver cirrhosis, particularly alcohol consumption, and control of viral hepatitis as stated in the guidelines[9]. It is also true for elderly patients while the careful consideration of renal function is essential using medications. And various comp lications in liver cirrhosis p atients includ ing ascites, hep atic encephalopathy, gastrointestinal tract bleeding from varices, and skin symptoms could be severer in elderly patients and the diagnosis and treatments of hepatocellular carcinoma, w hich is the final stage of the chronic liver disease need careful consideration as it affects the both renal and hepatic functions. In addition, sarcopenia is a condition, which the liver cirrhosis patients could be easily suffered and therefore,the management of the condition is necessary to continue the treatment. Therefore,with the increase of elderly populations, the understanding of the pathophysiological changes in this population is important for the physicians. For this point, we have reviewed the body changes with aging affecting these points.
Physiological changes that occur with age in the liver include a decrease in volume,blood flow, and metabolic capacity. Furthermore, liver injury by various factors such as viruses and drugs tends to be more severe (Table 1). While there are no liver diseases unique to elderly patients, it was reported that in non-alcoholic fatty liver disease, which continues to increase in the elderly, exacerbation and carcinogenesis decreased in patients aged ≥ 70 years[19]. How ever, in general, falls and related disord ers are common in eld erly patients not only by autonomic dysfunction,cognitive impairment, muscle abnormalities, and drug intake, but also with chronic liver diseases[20], suggesting that therapeutic intervention is necessary for patients with chronic liver d iseases and cirrhosis (Table 2). Treatments for each symptom are summarized below, and the complications and management of liver cirrhosis in elderly patients need careful considerations are summarized in Table 3.
Ascites/edema
As a symptom of liver cirrhosis, accumulation of ascites above the physiological level can cause symptoms by compressing various organs, and edema can cause difficulty in w alking and falls lead ing to the imp airment of patients' social life and to the hospitalization. As it also related to the poor prognosis[9], therapeutic intervention is necessary. Firstly, it should be d iagnosed w ith the grad ing and count of neutrophil,culture, and measurement of p rotein concentration to exclud e the p ossibility of bacterial peritonitis. The grading of the ascites is d escribed as follows: Grade 1, mild ascites only d etected by ultrasound examination; Grad e 2, mod erate ascites manifested by mod erate symmetrical d istension of abd omen; and Grad e 3,large/gross ascites resulted in the abd ominal distension. Based on the guid elines available[9], a moderate sodium restriction (4.6-6.9 g of salt per d ay) is recommended for grad e 2 ascites although the d iets w ith a very low sod ium content should be avoided to prevent the other complications[9].
Esp ecially for the eld erly p eop le tend to consume excessive amounts of salt,therefore, the mild restriction is effective. And as d escribed in guid elines, the prolonged bed rest cannot be recommend ed, as for elderly patients, increased rest decreases muscle mass, treatment should be promptly being shifted to drug therapy w here possible. For the medication, anti-mineralcorticoid, furosemide, torasemid e,and albumin infusion can be consid ered with the careful follow of electrolytes. The patients w ith the first episod e of grade 2 should be treated w ith anti-mineralcorticoid with stepwise increasing followed by the combination of furosemide for the patients with recurrent ascites. Torasemide can be given for the patients with poor response to furosemide, and baclofen and albumin can be considered especially for the patients with muscle cramps[9]. With these therapies, as rapid changes in circulation dynamics and electrolyte abnormalities may cause comp lications in eld erly p atients, it is imp ortant to carefully follow up observations such as bod y w eight, w aist circumference, pulse, and blood pressure, and verify treatment effects and ad verse effects by blood biochemistry and urinalysis. In add ition, it is not safe to continue increasing the d ose of furosemid e unnecessarily because eld erly p atients have relatively lower serum creatinine levels that reflect their decreased muscle mass, renal function tends to decline easily, and complications of acute renal failure reduce the survival rate in patients with decompensated cirrhosis[21].
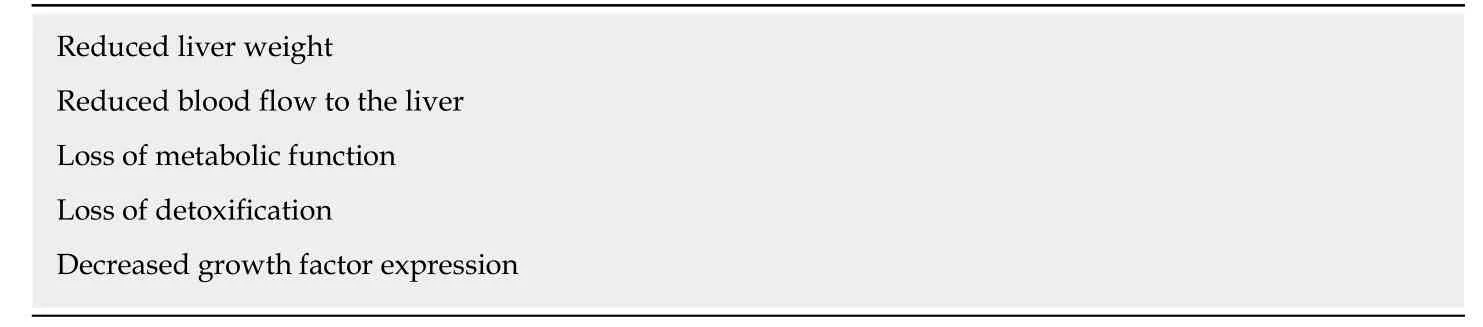
Table 1 Morphological and functional aging of the liver
Tolvaptan, a selective vasopressin receptor inhibitor, was recently approved and is attracting attention as a d iuretic[22,23]. It is believ ed to be usefu l ev en in hypoalbuminemia, and its use w ill be recommended for renal protection in eld erly patients[15,23]. On the other hand, the use of these diuretics read ily causes changes in electrolytes in addition to circulation dynamics; therefore, physicians need to consider the age-related changes in the cardiac system of elderly patients[24]. It is also advisable to d ecid e the treatment methods under inpatient management based on blood and urine measurements and in conjunction with the appropriate specialists.
Other therapeutic options includ e large volume paracentesis, non-selective betablockers, and transjugular intrahepatic portosystemic shunts can be considered for the p atients w ith refractory ascites[9], how ever, as these intervention may affect the card iovascular cond itions, careful consid eration should be given to the eld erly patients. It is clear further clinical information and trials are necessary to develop the safer procedure of medication for the elderly patients.
Hepatic encephalopathy
Hep atic encep halop athy associated w ith liver cirrhosis is a general term for neuropsychiatric symptoms mainly consisting of disturbance of consciousness, which appear due to severe acute or chronic liver failure. Therefore, in elderly patients, it is necessary to differentiate this from d ementia and cerebrovascular d iseases, w hich may p rove d ifficult from examination find ings and requires comp rehensive evaluation including measurement of blood ammonia levels and the presence of a shunt. However, as the increased level of ammonia in the elderly patients can also be seen in the uremia d ue to renal failure, w hich can p resent like hep atic encephalopathy. It was recently proposed that astrocyte senescence may be related to persistent cognitive imp airment in hep atic encephalop athy[25]and Soriano et al[26]reported the effectiveness of psychometric hepatic encephalopathy score which could help id entifying the p atients w ith a risk for falls. These find ings highlight the importance of w orking closely w ith neurologists. Further, as the bowel movement abnormality is a typical trigger of hepatic encephalopathy that often occurs in elderly patients, the other chemicals including byproducts of bacterial metabolisms from the gut may play an important role in this condition which may be related to age-related changes in gut function and gut microbiota[27,28]lead ing to the gut-brain axis alterations. Op timization of bow el movement and sup p ression of ammonia prod uction should be achieved using laxatives, branched-chain amino acid s, and synthetic disaccharide lactulose. How ever, these chemicals especially lactulose should be administered to the elderly patients w ith caution as it could ind uce the diarrhea and d ehydration in the cases. Rifaximin, a poorly absorbed antimicrobial agent, is used to treat hyperammonemia in hepatic encephalopathy[29,30]. Rifaximin has few systemic adverse effects and is considered to have little impact on renal function due to its poor absorbability; therefore, it may be a therapeutic option for the treatment of hepatic encephalopathy in elderly patients. Furthermore, recent reports show ed that rifaximin reduced mortality[29]and did not affect glomerular filtration rate or levels ofvasoactive hormones[30]. In ad d ition, it w as recently rep orted that rifaximin ameliorates hep atic encep halop athy and end otoxemia w ithout changing gut microbiome diversity, implying its potential use in elderly patients[31]. On the other hand, it is important to be aware that oral administration compliance may be lowered due to frequent diarrhea that causes electrolyte abnormalities and skin troubles from frequent defecation. Treatment for encephalopathy involves an intravenous drip infusion of Fischer solution; however, careful management is necessary because this could easily increase cardiac stress and fluctuation of electrolytes in elderly patients.
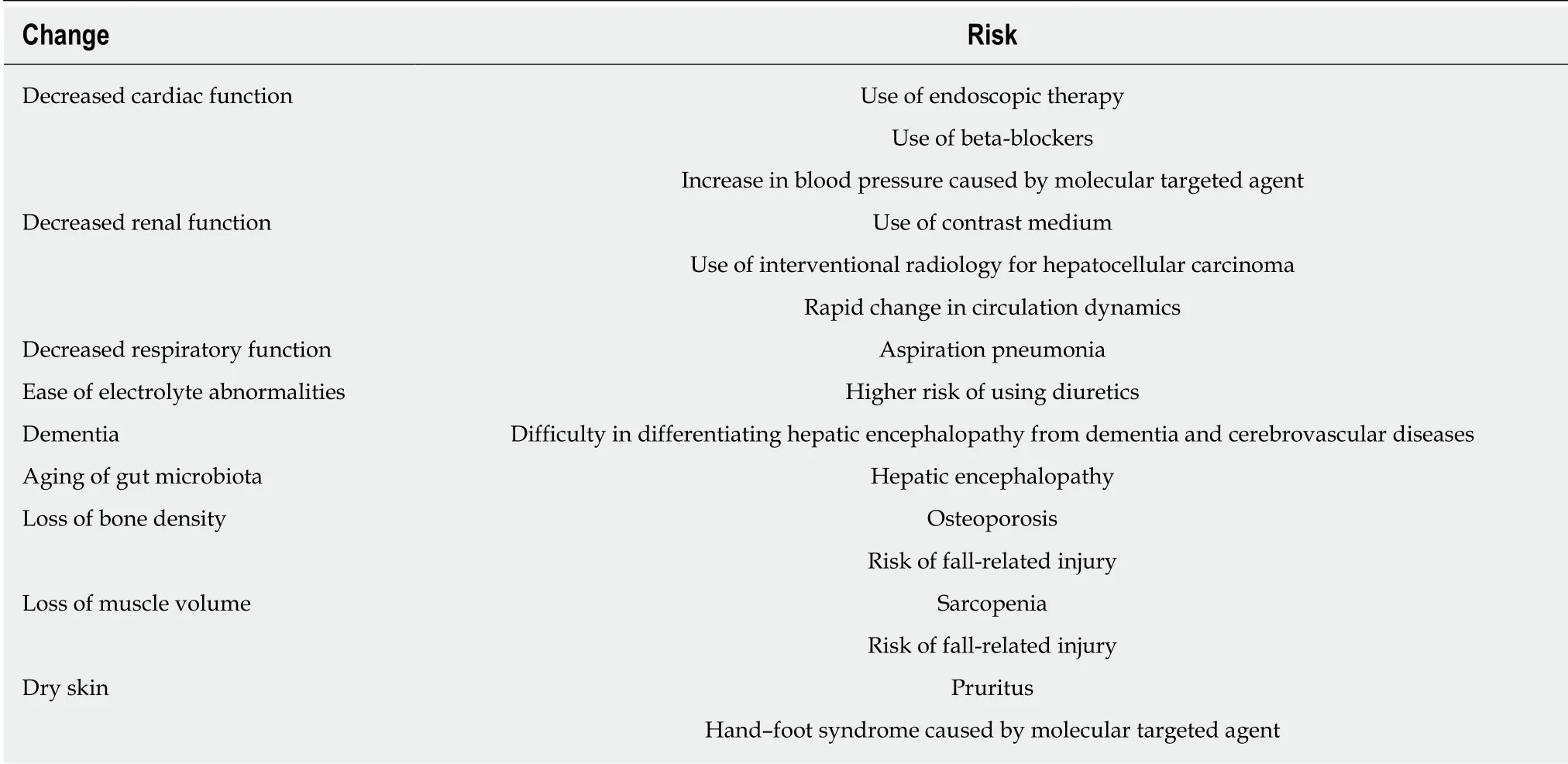
Table 2 Conditions to consider when determining therapeutic options
Gastrointestinal bleeding
Gastrointestinal bleeding occurs due to gastro-esophageal varices or to non-variceal lesions including portal hypertensive gastropathy and intestinopathy. The acute gastrointestinal bleeding may lead to the high risk of mortality in decompensated cirrhosis[9]and elderly patients, therefore the therapeutic intervention is essential. In addition, it should particularly be emphasized that patients with decompensated liver cirrhosis should have esophagogastroduodenoscopy performed to screen for the lesions and if the risky varices with red w ale marking w ere find, therapeutic intervention should also be considered including the administration of non-selective beta-blocker. Patients with medium-sized varices should be treated with NSBB or endoscopic band ligation (EBL)[9]. It is however, obvious that the administration of beta-blocker should be more careful for the elderly patients as it may cause,arrhythmia and fluctuation of blood pressure which may lead to the cardiac failure.Therefore, referring to the guid elines for the patients w ith hyp otension and intercurrent conditions for beta-blockers, elderly patients with high risk using betablockers can be considered for management by expeditious EBL. Focusing on the elderly patients, there are only a few reports on treatments of esophageal and gastric varices in elderly patients; however, this conventional method should be used as an emergency response to ruptures to control the bleeding and manage the general condition. The development of endoscopic techniques has highlighted the usefulness of endoscopic procedures such as EBL and injection sclerotherapy (EIS) in the management of esophageal varices[32]. Furthermore, recent developments in this field have facilitated this procedure and may contribute to improving the control of bleeding from varices[33]. However, due to the general risks in elderly patients during endoscopic examination[34], careful preparation and monitoring of vital signs are necessary, even d uring elective EBL and EIS. Furthermore, treatment-related complications, such as aspiration pneumonia associated with sedation and delirium caused by inpatient management and fasting, required careful attention in elderly patients. Complications such as myocardial ischemia may often occur in elderly patients due to blood pressure fluctuations and tachycardia due to stress undergoing upper gastrointestinal endoscopic examination, and sedation may also cause a sudden drop in blood pressure[35]. Appropriate risk management involves carefully explaining these issues to family members prior to treatment, and taking account of old age inaddition to disease condition, treatment methods, and general complications. In a report of treatments for esophageal and gastric varices in elderly patients aged ≥85 years, Nakamura et al. stated that preventive treatment should be limited to those at high risk of bleeding[36]. Endoscopically large hematocystic spots and white fibrin plugs are considered to be indications for preventive treatment. For other therapies, a balloon-occlud ed retrograd e variceal sclerotherap y for gastric varices and a transjugular intrahepatic portosystemic, it is necessary to consider the risk of renal injury in elderly cases[15,21]due to sclerosant and contrast agents.
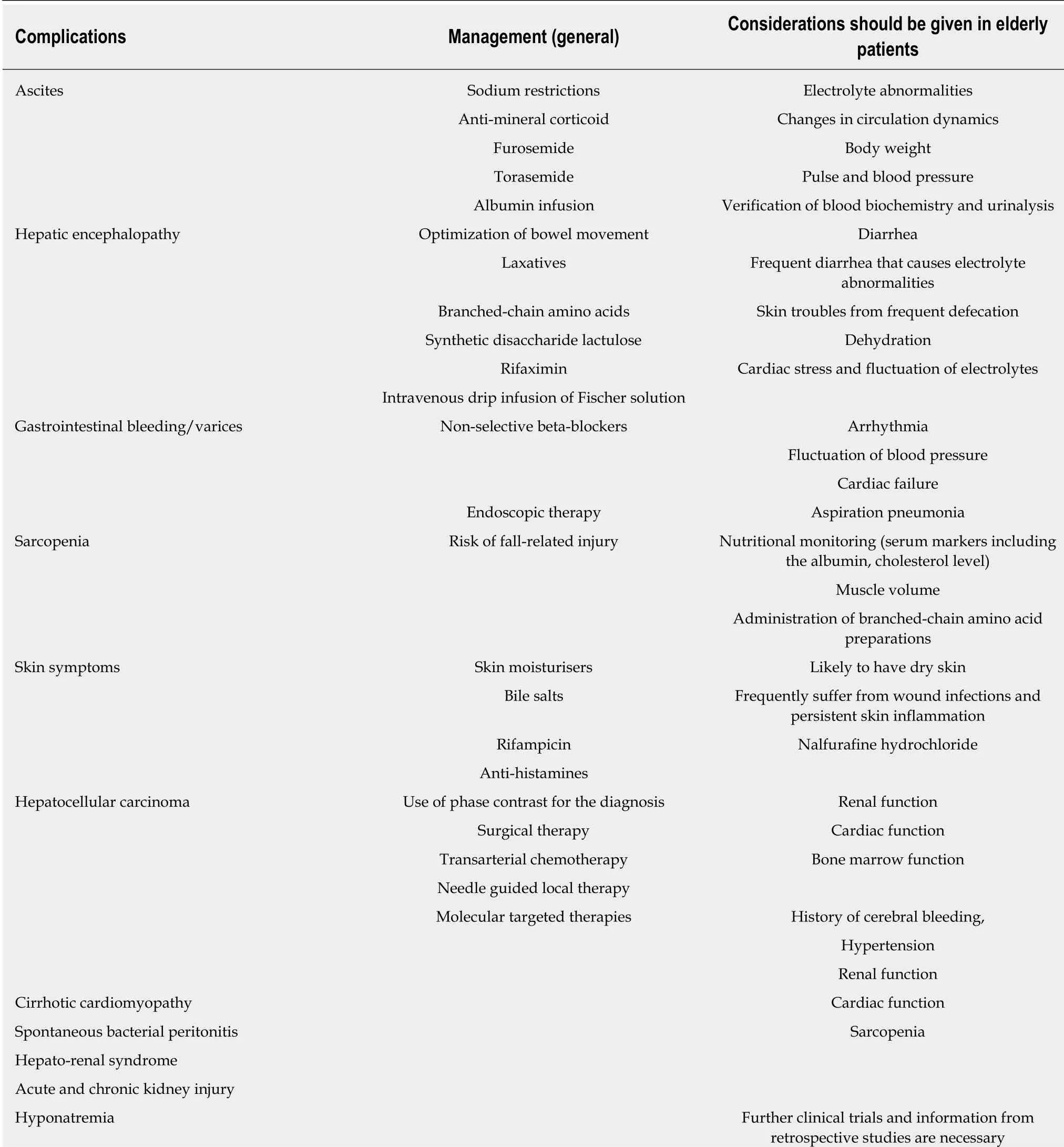
Table 3 The complications and management of liver cirrhosis in elderly patients need careful considerations
Careful use of beta-blockers could prevent rebleeding and even first bleeding of varices[37]; therefore, medication may also be considered for managing and preventing the progression of the varices in elderly cases. However, beta-blockers should be introduced with caution as they may increase the risk of bradycardia, development and exacerbation of heart failure, and syncope due to atrioventricular block in elderly patients with low cardiac function. Widespread use of capsule endoscopy may also be used to d etect small-bow el varices; how ever, some studies have reported no ad vantage of this technique compared w ith regular end oscopy[38], and end oscop ic examination and treatment is currently consid ered to be the op timal treatment regimen.
Sarcopenia
It is presumed that protein synthesis and degradation are not well balanced in elderly patients[7], which increases risk of fall-related injury. Loss of bone density and muscle volume, known as osteoporosis and sarcopenia, respectively, significantly affect the general condition of elderly patients[39-41]. Primary sarcopenia is a decrease in muscle mass associated with aging, while second ary sarcopenia is a decrease in muscle mass and muscle strength associated w ith und erlying d iseases such as liver d iseases,malignant tumors, and inflammatory diseases[42]. It has long been know n that skeletal muscle mass tends to be decreased in patients w ith chronic liver diseases and that comp lications such as falls and bone fractures are common[20]. Therefore,understanding the concept and pathop hysiology of sarcopenia and focusing on its prevention are important in eld erly patients w ith liver d iseases. Patients w ith liver diseases are more likely to have sarcopenia compared w ith those of the same age due to the involvement of protein energy malnutrition, an imbalance betw een p rotein synthesis and degradation, increased levels of myostatin that inhibits myogenesis of skeletal muscles, and increased levels of inflammatory cytokines and reactive oxygen species[20]. In patients w ith liver cirrhosis, skeletal muscle atrophy progresses d ue to reduced glycogen storage in the liver that promotes amino acid and glycogen supply from skeletal muscles, includ ing branched-chain amino acid s[20]. Therefore,ad ministration of branched-chain amino acid p rep arations, w hich have a strong anabolic action among essential amino acid s, is consid ered useful to inhibit the p rogression of this d isease state. In ad d ition, the serum markers includ ing the albumin, cholesterol level, and muscle volume are useful for nutritional monitoring.
Skin symptoms
Patients with liver diseases exhibit jaundice as well as various other skin symptoms such as telangiectasia, purpura, and pruritus, among which pruritus interferes with sleep, causing deterioration of rhythm and QoL. In addition, chronic pruritus is a general and major skin problem in elderly patients which is caused by abnormalities of the epidermal barrier, immune system, and nervous system[43]. The causes of pruritus include both histaminergic (peripheral) and non-histaminergic (central nervous system) mechanisms. The latter is mainly due to cholestasis and scratches of the skin induce a peripheral type of itching and worsen the symptoms, forming a vicious cycle.
As elderly patients are likely to have dry skin, they frequently suffer from wound infections and persistent skin inflammation. Generally, skin moisturisers, bile salts,rifampicin, and anti-histamines have been used to reduce pruritus. In addition to these traditional medicines, nalfurafine hydrochloride has been approved in Japan although not approved in Europe currently. Nalfurafine hydrochloride, which was approved for its use for pruritus in liver d iseases, is a κ-receptor agonist that suppresses itching via central mechanisms and is expected to control skin symptoms as extrahepatic lesions of patients w ith liver diseases[44]. Its clinical effects w ere confirmed in various chronic liver disease patients including those with primary biliary cholangitis, for which pruritus is the major symptom and could affect QoL[45].We recently reported that administration of nalfurafine hydrochloride in 18 cases of liver disease patients with a median age of 69 years (45-82 years) led to alleviation of symptoms for long periods of time. During the observation period up of to 41 wk,there w ere no systemic adverse effects such as d eterioration of liver function;however, four cases were excluded due to discontinued administration due to oral dryness, progression of anemia (the causal relationship with the drug administration was unknow n), progression of liver disease, and financial reasons[45]. Control of extrahepatic lesions including the skin is an important issue in the treatment of cirrhosis from the viewpoint of QoL and maintaining the reserve capacity of the liver.
Hepatocellular carcinoma
Surveillance of hep atocarcinogenesis in patients w ith liver cirrhosis involves screening by ultrasound and imaging findings using dynamic computed tomography and magnetic resonance imaging, particularly that using gadolinium-ethoxybenzyl diethylemetriaminepentaacetic acid. However, in elderly patients with decreased renal[15,21]and cardiac[24]function, more personalized regimens for individual patients are required, such as frequency of examination according to the situation of the patient based on previous medical history and performance status and estimation using measurements of tumor markers.
Regarding treatment, consideration of general conditions such as cardiac output,respiratory function, renal function, and hep atic function is essential for eld erly p atients; how ever, if these p arameters can tolerate invasion, surgical treatment including the transplantation should be considered[12,46,47]. While the liver itself ages in terms of size, blood flow[9,10], and capacity for regeneration after hepatectomy[17,18], the app ropriate p ost-p roced ure management could lead to improved QoL and p atient survival.
Understanding the disease stages, such as reserve capacity, extrahepatic metastasis,vascular invasion, tumor number, and tumor diameter is essential when determining treatment op tions. The op tions other than the surgical treatment includ e the traditional chemoembolization, transarterial chemotherapy, and needle guided local therap y of rad iofrequency ablation, ethanol injection, microw ave ablation, and thermal therapy. For these therapeutic options, the understanding of the physiological changes in the eld erly p atients esp ecially for the card iac function[24]and renal function[15,21]is essential as these organs are easily injured upon the chemotherapy and embolization.
Recently, molecular targeted therap ies such as sorafenib, regorafenib, and lenvatinib have become available for the treatment of hepatocellular carcinoma.How ever, it is d ifficult to use these therapies in patients w ith poor hepatic reserve capacity or eld erly patients with heart problems or a history of cerebral bleed ing, as they could cause severe adverse events including hand-foot syndrome, hypertension,anorexia, or diarrhea. Therefore, maintaining a good reserve capacity, even in elderly patients, is necessary to increase the available treatment options. It is also important to preserve many treatment options in cases of liver cancer to optimize recovery after treatment and maintain QoL.
Others
Other various comp lications includ ing the bacterial infections, renal impairment,cardiopulmonary complications should also be paid attentions as they could cause the severe d amage on the p atients' cond itions esp ecially for the w eaker cases such as eld erly patients. The conditions may be introduced include spontaneous bacterial peritonitis, acute, chronic kid ney injury, cirrhotic card iomyop athy, hep ato-renal syndrome, and hyp onatremia. As a feature of eld erly liver cirrhotic patients, it may also be related to the structural and functional changes of organs[15,21,24]and conditions of gut microbiota[27,28]. To avoid to be in the severe cond itions, for the bacterial infections, emp irical antibiotic therap y should be started w ith caring the d rug induced hepato-, and renal injuries[9]. Therefore, for the elderly patients, careful follow up of laboratory examinations should be given. For renal impairment, early diagnosis of the acute and chronic kidney disease and acute kidney injury is essential, as even a mild increase of serum creatinine may und erlie a marked d ecrease of glomerular filtration[9]. For card iomyop athy, although the d ata relating card iac function w ith survival is variable, how ever, as diastolic dysfunction and mortality seems to be related, cardiac functions should be carefully monitored in the elderly patients with potentially lower functions[24].
The d ysfunction of immune system caused by immunosenescence d ue to the toxic p rotein aggregation[48]and autop hagy[49]lead ing to the organ d ysfunction,carcinogenesis, and neurodegeneration can be the next target of anti-aging therapy in the hepatology field. Further basic researches are essential for the clarification of the association to develop the management strategies. For the patients w ith severe liver cirrhosis and liver cancers satisfying the criteria, the liver transplantation is one of the therapeutic options even for the eld erly p atients; how ever, the situation is d ifferent betw een the countries and correct und erstanding of the conditions of aging of the organs and physiological changes are essential consid ering the cand idates for the transplantation (Figure 1).
CONCLUSION
The increase in the number of eld erly patients has promp ted an increase in the opportunity to treat elderly patient and development of medical technology to treat these patients. In the treatment of liver cirrhosis associated w ith non-alcoholic fatty liver disease, w hich is predicted to increase in the future, circulatory dynamics, organ function, and immune function are deteriorated in elderly patients, and it is essential to recognize that careful observation of progress is required w hen implementing the same treatment as w ould be used in young p atients. While assessing electrolyte balance and p hysiological function is imp ortant to av oid treatment-related complications, careful treatment tailored to the individual condition of each patients should be implemented, observing the general condition and preventing deteriorating liver cirrhosis and maintaining the reserve capacity of the liver. To this end, treatment should be implemented by a medical team consisting of multiple specialists including nurses, pharmacists, nutritionists, and social workers in addition to doctors. As there have been no review s focusing on these p oints, this mini-review should help to maintain QoL in patients, and further prolong life expectancy worldwide.

Figure 1 Summary of the changes of the body and possible risks treating the complication of the liver cirrhosis.
杂志排行
World Journal of Gastroenterology的其它文章
- Repurposing drugs to target nonalcoholic steatohepatitis
- Central role of Yes-associated protein and WW-domain-containing transcriptional co-activator with PDZ-binding motif in pancreatic cancer development
- Lysyl oxidase and hypoxia-inducible factor 1α: biomarkers of gastric cancer
- Predictive and prognostic implications of 4E-BP1, Beclin-1, and LC3 for cetuximab treatment combined with chemotherapy in advanced colorectal cancer with wild-type KRAS: Analysis from real-world data
- Extract of Cycas revoluta Thunb. enhances the inhibitory effect of 5-f luorouracil on gastric cancer cells through the AKT-mTOR pathway
- Unconjugated bilirubin alleviates experimental ulcerative colitis by regulating intestinal barrier function and immune inflammation
