早期腹腔镜手术联合内镜鼻胆(胰)引流治疗重症急性胰腺炎患者的效果
2018-04-26刘宁
刘宁
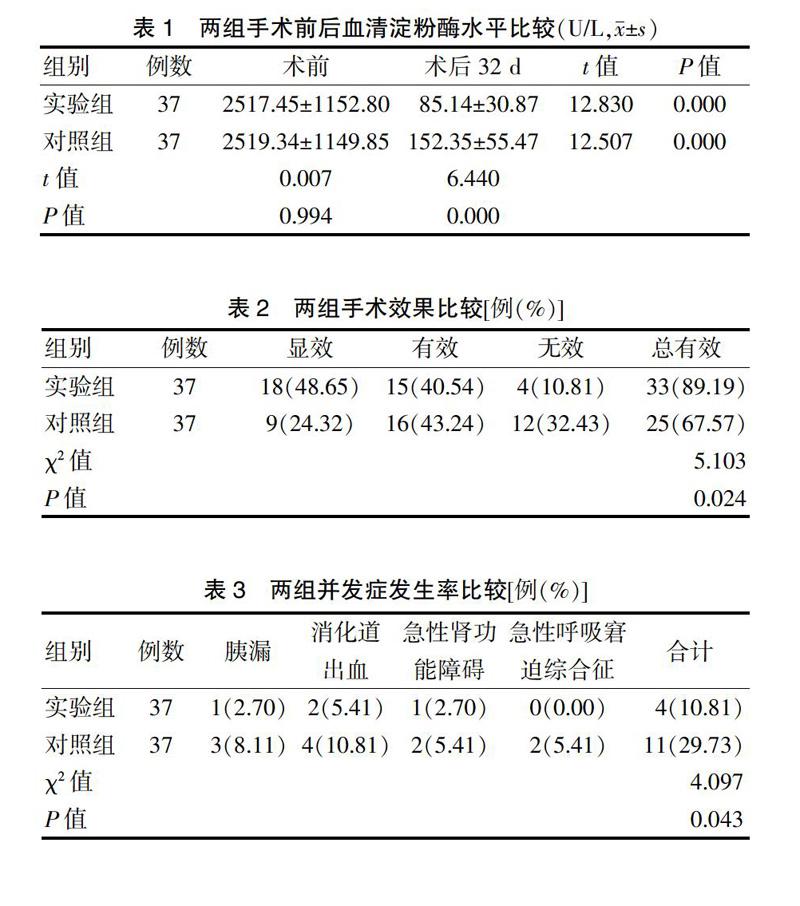
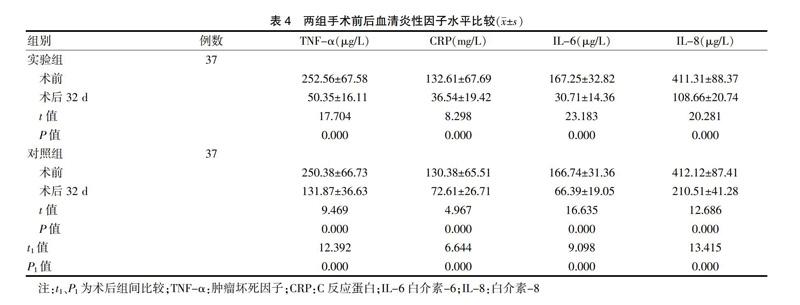
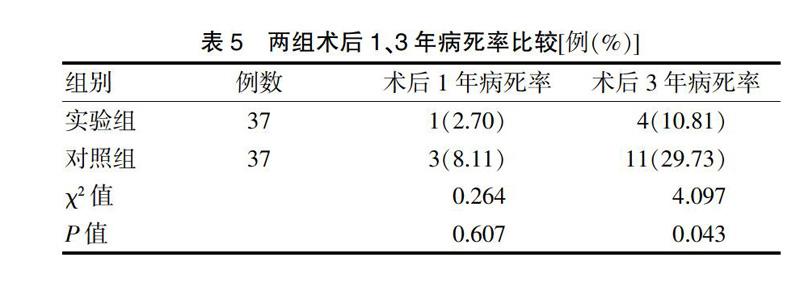
[摘要] 目的 探討早期腹腔镜手术联合内镜鼻胆(胰)引流治疗重症急性胰腺炎(SAP)患者效果及术后中、远期随访结果。方法 回顾性分析2011年2月~2014年5月武汉科技大学附属孝感医院SAP患者74例,根据不同术式分为实验组和对照组,各37例。对照组施行腹腔镜手术治疗,实验组施行腹腔镜手术+内镜鼻胆(胰)引流治疗。对比两组手术效果、术后并发症发生率、术前及术后32 d血清淀粉酶及炎性因子[肿瘤坏死因子(TNF)-α、白介素(IL)-6、C反应蛋白(CRP)、IL-8]变化情况,随访3年,统计两组病死率。 结果 ①血清淀粉酶:术前两组血清淀粉酶水平比较差异无统计学意义(P > 0.05),术后32 d两组血清淀粉酶水平较术前明显下降,且实验组明显低于对照组,差异有高度统计学意义(P < 0.01);②手术效果:实验组手术总有效率(89.19%)明显高于对照组(67.57%),差异有统计学意义(P < 0.05);③术后并发症:实验组术后并发症发生率(10.81%)明显低于对照组(29.73%),差异有统计学意义(P < 0.05);④血清炎性因子:术后32 d两组血清炎性因子TNF-α、IL-6、CRP、IL-8水平均显著低于术前(P < 0.01),且实验组血清炎性因子TNF-α、IL-6、CRP、IL-8水平显著低于对照组,差异有高度统计学意义(P < 0.01);⑤术后病死率:两组术后1年病死率比较差异无统计学意义(P > 0.05),实验组术后3年病死率(10.81%)低于对照组(29.73%),差异有统计学意义(P < 0.05)。 结论 联合采用早期腹腔镜手术、内镜鼻胆(胰)管引流术治疗SAP,可显著降低患者血清淀粉酶、炎性因子TNF-α、IL-6、CRP、IL-8水平,有效减少术后并发症发生率及病死率,进一步提高手术效果。
[关键词] 重症急性胰腺炎;腹腔镜手术;内镜鼻胆(胰)引流
[中图分类号] R657.51 [文献标识码] A [文章编号] 1673-7210(2018)02(a)-0077-05
Effect of early laparoscopic surgery combined with endoscopic nassl biliary (pancreatic) drainage in the treatment of severe acute pancreatitis patients
LIU Ning
The First Department of General Surgery, Xiaogan Hospital Affiliated to Wuhan University of Science and Technology, Hubei Province, Xiaogan 432000, China
[Abstract] Objective To investigate the effect of early laparoscopic surgery combined with endoscopic naso biliary (pancreatic) drainage in the treatment of severe acute pancreatitis and the postoperative follow-up results of mid term and long term. Methods Seventy-four patients with severe acute pancreatitis (SAP) from February 2011 to May 2014 in Xiaogan Hospital Affiliated to Wuhan University of Science and Technology were retrospectively analyzed and divided into experimental group and control group according to different surgical procedures, with 37 cases in each group. The control group received laparoscopic surgery, and the experimental group received laparoscopic surgery combined with endoscopic nasal biliary (pancreatic) drainage. The surgical results, postoperative complication rate, the changes of preoperative and postoperative 32 d of serum amylase and inflammatory factor [tumor necrosis factor (TNF) -α, interleukin (IL)-6, C reactive protein (CRP), IL-8] of the two groups were compared. Followed-up for three years, the mortality rates of both groups were counted. Results ①Serum amylase: there was no significant difference in serum amylase level between the two groups (P > 0.05), the levels of serum amylase in the two groups were significantly lower than that before surgery, the experimental group was significantly lower than the control group, and the difference was highly statistically significant (P < 0.01). ②Operation effect: the total effective rate in the experimental group (89.19%) was significantly higher than that in the control group (67.57%), the difference was statistically significant (P < 0.05). ③Postoperative complications: the incidence of postoperative complication rate in the experimental group (10.81%) was significantly lower than that in the control group (29.73%), the difference was statistically significant (P < 0.05). ④Serum inflammatory factors: the levels of serum inflammatory factors TNF-α, IL-6, CRP and IL-8 were significantly lower than those before operation (P < 0.01). The levels of TNF-α, IL-6, CRP and IL-8 in the experimental group were significantly lower than those in the control group, the differences were highly statistically significant (P < 0.01). ⑤Postoperative fatality rate: there was no statistically significant difference between the two groups in 1 year after surgery (P > 0.05). The mortality rate of the experimental group (10.81%) was lower than that of the control group (29.73%), the difference was statistically significant (P < 0.05). Conclusion Early laparoscopic surgery combined with endoscopic nasal biliary (pancreatic) drainage for the treatment of SAP can significantly reduce serum amylase, the levels of inflammatory factors TNF-α, IL-6, CRP and IL-8, and can effectively reduce the incidence of postoperative complication rate and fatality rate and further improve the operation effect.
[Key words] Severe acute pancreatitis; Laparoscopic surgery; Endoscopic nasal biliary (pancreatic) drainage
重症急性胰腺炎(SAP)为临床常见急腹症,是由全身炎症综合征引发的特殊类型急性胰腺炎,临床主要表现为腹痛、黄疸、高热、呼吸异常、神志改变,严重者甚至休克,病情险恶,并发症多,病死率极高,占急性胰腺炎患病人数的10%~20%,严重威胁患者生命安全[1-2]。因此,积极采取疗效确切、安全性高的治疗方案对降低SAP患者病死率、改善生活质量具有重要意义。目前,临床在SAP早期治疗策略上存在一定争议,多数学者认为急性反应期采用复杂手术或非手术治疗,均对患者整体状况不利[3-4]。以往临床治疗SAP多采用传统开腹手术治疗,虽可取得一定效果,但术后易出现切口感染、肠瘘、胰瘘及切口疝等多种并发症,且手术时间较长,患者耐受力不佳,手术效果并不理想[5-6]。近年来,随着微创技术的飞速发展,SAP治疗有了更多选择,如内镜、腹腔镜下引流术等,但有学者提出,单一治疗方案易导致术后并发症发生率及复发率升高,影响手术效果[7]。本研究为进一步提高手术效果,选取74例SAP患者,分组探讨早期腹腔镜手术联合内镜鼻胆(胰)引流治疗SAP患者效果。现报道如下:
1 资料与方法
1.1 一般资料
回顾性分析2011年2月~2014年5月武汉科技大学附属孝感医院(以下简称“我院”)SAP患者74例,根据不同术式分为实验组与对照组,各37例。其中实验组女20例,男17例;年龄29~77岁,平均(50.92±5.10)岁;发病至入院时间3~7 h,平均(4.62±0.31)h。对照组女21例,男16例;年龄28~78岁,平均(51.15±5.16)岁;发病至入院时间2~7 h,平均(4.85±0.37)h。两组基线资料比较差异无统计学意义(P > 0.05),具有可比性。本研究经医院医学伦理委员会通过。
1.2 纳入标准
①均符合中华肝胆外科杂志发布《重症急性胰腺炎诊治草案》[8]中SAP相关诊断标准;②手术指征明确;③纳入研究前未接受相关手术治疗;④患者或其家属知情同意并签署知情同意书。
1.3 排除标准
①具有手术禁忌证;②伴有全身性感染性疾病;③合并恶性肿瘤;④妊娠期、哺乳期女性;⑤合并肾肝功能障碍;⑥存在认知障碍或神经系统病变,无法配合本研究手术及随访。
1.4 方法
1.4.1 对照组 施行腹腔镜手术治疗,操作如下:气管插管全麻,采用5孔法建立腹腔镜下操作环境,即脐孔置镜,分别为剑突与脐连线中点、左右髂窝、左右锁骨中线肋缘下约3 cm位置分别戳孔,以Hasson技术建立脐下人工气腹;根据患者实际情况切开肝胃韧带,并进行胃结肠韧带开窗、部分胰床松动、胰腺被膜切开减压、部分坏死组织清除等术式;术中应用5000~10 000 mL生理盐水反复冲洗腹腔、胰周小网膜囊,冲净后吸尽生理盐水,选择一根引流管经文氏孔置入直至小网膜囊内、一根引流管自胃结肠韧带开窗处置入直至胰床下缘、一根引流管置入盆底,均为硅胶引流管;术后常规进行腹腔冲洗引流,待患者症状、体征恢复正常,腹腔引流管无液体引出后拔出引流管。
1.4.2 实验组 施行腹腔镜手术+内镜鼻胆(胰)引流治疗,腹腔镜手术操作同对照组,内镜鼻胆(胰)引流操作如下:术前3 d内行十二指肠镜下逆行胰胆管造影,选用多侧孔聚乙烯塑料鼻胆(胰)引流管(Olympus公司,PR-5Z型)进行内镜鼻胆(胰)引流治疗,每天胆汁胰液引流量为300~900 mL,导管留置7~32 d,术后定期观察记录引流液性质及引流量。
1.5 观察指标
1.5.1 血清淀粉酶 两组术前、术后32 d均抽取3 mL肘静脉血液,常溫下高速离心处理(3000 r/min,10 min),分离血清,并置于-80℃环境下贮存待测,以速率法测定血清淀粉酶水平,并严格遵循试剂盒(VITROS公司)操作说明书。
1.5.2 手术效果 疗效评定:以症状基本消失,血清淀粉酶恢复至正常水平,即<115 U/L为显效;症状有所好转,血清淀粉酶明显下降,且趋于正常水平为有效;未达到上述标准为无效[9]。总有效率=(显效+有效)/总例数×100%。
1.5.3 并发症 统计两组术后并发症发生率,包括胰漏、消化道出血、急性肾功能障碍、急性呼吸窘迫综合征。
1.5.4 血清炎性因子 两组术前、术后32 d均抽取3 mL肘静脉血,常温下高速离心处理(3000 r/min),10 min,分离血清,并置于-80℃环境下贮存待测,以酶联免疫吸附试验测定血清肿瘤坏死因子(TNF)-α、白介素(IL)-6、C反应蛋白(CRP)、IL-8水平,并严格遵循试剂盒(Sekisiui公司)操作说明书。
1.5.5 术后病死率 随访3年,统计两组术后1、3年病死率。
1.6 统计学方法
采用SPSS 19.0对所得数据进行统计学分析,计量资料采用均数±标准差(x±s)表示,组间比较采用t检验,计数资料采用百分率表示,组间比较采用χ2检验。以P < 0.05为差异有统计学意义。
2 结果
2.1 两组手术前后血清淀粉酶水平比较
术前两组血清淀粉酶水平比较差异无统计学意义(P > 0.05)。术后32 d两组血清淀粉酶水平较术前明显下降,且实验组明显低于对照组,差异有高度统计学意义(P < 0.01)。见表1。
2.2 两组手术效果比较
实验组手术总有效率(89.19%)明显高于对照组(67.57%),差异有统计学意义(P < 0.05)。见表2。
