唐山市体检人群脂肪肝患病率调查分析
2017-12-16孟昱林张海艳宋宝国周惠兰金秀平史国辉
孟昱林, 张海艳, 宋宝国, 周惠兰, 金秀平, 史国辉
(华北理工大学附属医院, 河北 唐山 063000)
唐山市体检人群脂肪肝患病率调查分析
孟昱林, 张海艳, 宋宝国, 周惠兰, 金秀平, 史国辉
(华北理工大学附属医院, 河北 唐山 063000)
目的探究唐山市体检人群脂肪肝患病率情况,以期为脂肪肝的预防和调治提供合理依据。方法采集2014年3月-2016年2月唐山市12 808例体检人群资料,其中脂肪肝有3540例。统计年龄、性别、BMI、空腹血糖(FBG)、TC、TG、LDL-C以及肝脏超声检查结果。计数资料组间比较采用χ2检验;计量资料组间比较采用t检验。结果7151例男性体检者中脂肪肝2750例(38.46%),5657例女性体检者中脂肪肝790例(13.96%),男性与女性患病率比较差异有统计学意义(χ2=947.25,P<0.01)。不同年龄段(18~29岁、30~39岁、40~49岁、≥50岁)男女间脂肪肝检出率比较差异均有统计学意义(χ2值分别为337.58、474.06、449.38、12.86,P值均<0.01)。男性、女性在不同BMI[肥胖(BMI≥28)、超重(24≤BMI<28)、正常(BMI<24))]间脂肪肝的检出率比较差异有统计学意义(χ2值分别为1104.01、500.23,P值均<0.01)。分别对肥胖(BMI≥28)、超重(24≤BMI<28)、正常(BMI<24)体检者中男性与女性脂肪肝检出率进行比较,差异均有统计学意义(χ2分别为71.24、87.97、323.84,P值均<0.01)。男性、女性体检者中肥胖及超重人群脂肪肝检出率均显著高于正常人群(P值均<0.01)。脂肪肝组与非脂肪肝组FPG、TC、TG、LDL-C比较,差异均有统计学意义(t值分别为17.482、13.698、22.133、27.334,P值均<0.001)。男性体检者中,脂肪肝与非脂肪肝体检者间FPG、TC、TG、LDL-C水平比较,差异均有统计学意义(t值分别为11.288、8.652、11.671、20.118,P值均<0.01);女性体检者中,脂肪肝与非脂肪肝体检者间FPG、TC、TG、LDL-C水平比较,差异均有统计学意义(t值分别为16.816、5.532、15.154、18.507,P值均<0.01)。结论唐山市成人体检人群脂肪肝患病率为男性明显高于女性。导致脂肪肝的主要因素可能是超重或肥胖、高脂血症、糖代谢异常。
脂肪肝; 患病率; 数据说明, 统计
随着居民膳食结构(高脂肪、高热量饮食)、生活方式(多坐少动,运动减少)的改变,代谢性疾病(肥胖症、糖尿病以及代谢综合征等)逐年增加,渐进地影响人们的健康。特别是脂肪肝检出率逐年上升,不管是酒精性脂肪肝还是非酒精性脂肪肝均有进展到肝硬化、肝癌甚至肝衰竭的危害[1]。在我国成年人中,脂肪肝的检出率为12%~15%,脂肪肝通过超声总体检出率约为10%,其中因为代谢因素导致脂肪肝检出的约占90%。在过去近10年里,多个城市的脂肪肝患病率增长了1倍[2]。唐山市作为经济发达工业城市,目前没有脂肪肝相关流行病学调查,本研究对体检成人中脂肪肝检出情况进行统计并分析相关影响因素,以期为大众健康宣教、健康管理及促进提供数据支持。
1 资料与方法
1.1 研究对象 收集2014年3月-2016年2月在本院参加体检的成人12 808例,其中男7151例,女5657例,年龄18~88岁,平均(43.19±14.16)岁。18~29岁2393例,男1160例,女1233例;30~39岁3372例,男1734例,女1638例;40~49岁3286例,男1869例,女1417例;50岁以上3757例,男2388例,女1369例。
1.2 观察指标 BMI、空腹血糖(FPG)、TC、TG、LDL-C、腹部彩超。
1.3 排除标准 (1)未满18岁的未成年人;(2)患有病毒性肝炎、药物性肝炎、恶性肿瘤、慢性胰腺炎、急性感染、肾病综合征以及有长期应用糖皮质激素史的体检者。
1.4 诊断标准 超重或肥胖: 24≤BMI<28为超重,BMI≥28为肥胖。血脂异常[3]:TC≥5.7 mmol/L,TG≥1.7 mmol/L,LDL-C≥3.7 mmol/L。血糖异常:根据WHO[4](1999年)糖尿病诊断、糖代谢状态分类标准[4],血糖≥6.1 mmol/L。脂肪肝[5]:根据超声影像学表现,符合以下3项表现中的2项者诊断为弥漫性脂肪肝:(1)肝脏近场回声弥漫性增强(“明亮肝”),回声强于肾脏;(2)肝内管道结构显示不清;(3)肝脏远场回声逐渐衰减。

2 结果
2.1 不同年龄段男性和女性体检者的脂肪肝检出率
12 808例体检者中共检出脂肪肝3540例,总体检出率为27.64%,其中男2750例,检出率38.46%,女790例,检出率13.96%,男性与女性患病率比较差异有统计学意义(χ2=947.25,P<0.01)。不同年龄段男女间脂肪肝检出率比较差异均有统计学意义(P值均<0.01)。脂肪肝在不同性别、年龄段检出情况详见表1。

表1 脂肪肝在不同性别、年龄段检出情况[例(%)]
注:与40~49岁比较,1)P<0.01;与≥50岁比较,2)P<0.01
2.2 不同BMI男性和女性体检者的脂肪肝检出率 男性、女性在不同BMI脂肪肝的检出率比较差异有统计学意义(P值均<0.01)。分别对肥胖、超重、正常体检者中男性与女性脂肪肝检出率进行比较,差异均有统计学意义(χ2分别为71.24、87.97、323.84,P值均<0.01)。男性、女性体检者中肥胖及超重人群脂肪肝检出率均显著高于正常人群(P值均<0.01)(表2)。
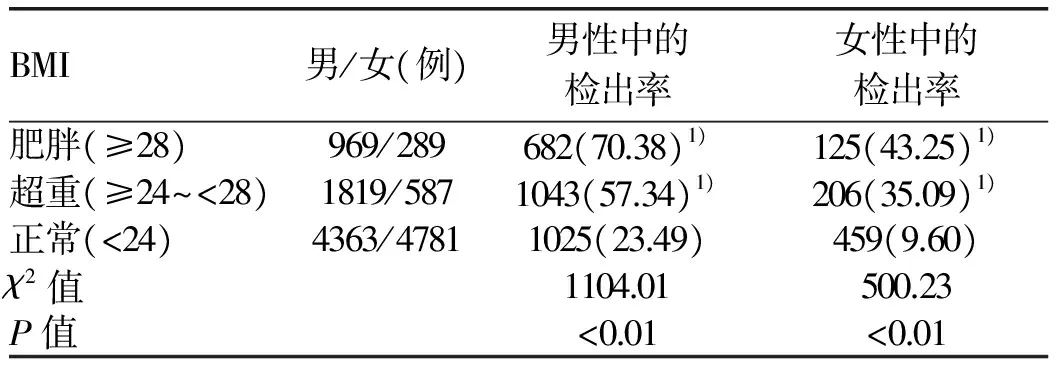
表2 不同BMI男性和女性体检者的脂肪肝检出率[例(%)]
注:与正常组比较,1)P<0.01
2.3 脂肪肝与非脂肪肝体检者间各项指标的比较 12 808例体检者分为脂肪肝组(n=3540)、非脂肪肝组(n=9268),脂肪肝与非脂肪肝组FPG、TC、TG、LDL-C比较,差异均有统计学意义(P值均<0.001)(表3)。

表3 脂肪肝和非脂肪肝血糖及血脂指标的比较
2.4 不同性别的体检者间各项指标的比较 男性体检者中,脂肪肝与非脂肪肝体检者间FPG、TC、TG、LDL-C水平比较,差异均有统计学意义(P值均<0.01);女性体检者中,脂肪肝与非脂肪肝体检者间FPG、TC、TG、LDL-C水平比较,差异均有统计学意义(P值均<0.01)(表4)。
3 讨论
脂肪肝是多种因素导致肝脏脂肪(主要为甘油三酯成分)积累过多、代谢平衡失调的病理状态,是一种以肝细胞大泡性脂肪变性为病理特征的异质性疾病[6]。唐山市健康人群脂肪肝检出率为27.64%,其中女性检出率为13.96%,男性检出率为38.46%。脂肪肝的检出率总体上随年龄增长而增加,其中女性高发年龄段为50岁以上(检出率为32.80%), 明显高于49岁以前; 男性高发年龄段为40~49岁(检出率为46.76%);男性在不同年龄段脂肪肝检出率明显比女性高,与相关文献报道一致[7]。原因可能为男性进入30 岁以后,因为工作压力大、应酬多、不良生活习惯(如吸烟、饮酒、高脂、高糖饮食等)以及运动量少等因素引起超重或肥胖,这些都是促成脂肪肝形成的重要因素;而女性50岁以后基本进入围绝经期,因为卵巢功能减弱、体内激素紊乱、雌激素水平不同程度地减少、导致脂质代谢异常,容易引起肥胖、糖尿病和脂肪肝的发生[8]。均与性激素的作用有关,雄激素是内脏脂肪增加的促进因子,而雌激素是内脏脂肪增加的抑制因子[9]。
脂肪肝的检出率具有地区性差异,唐山市脂肪肝27.64%的检出率低于东北沈阳38.1%[10]以及东南沿海深圳30.75%[11]和汕头28.02%[12]的检出率;但高于西北延安地区25.69%[13]、乌鲁木齐市26.80%[14]、以及西南重庆地区15.55%[15]和华东上海市20.82%[16]、赣州市15.8%[17]的检出率。在同省内比较,唐山市脂肪肝的检出率也高于石家庄地区23.8%[18]以及河北沿海城镇21.47%[19]的检出率。通过比较不同检出率存在的因素应该与不同地域的社会经济发展程度、饮食文化、生活习惯差异密切相关。
脂肪肝作为一种临床症状,不是独立的疾病,临床以超声检查最为便捷,但是对脂肪肝程度的判定需要结合其他相关检查综合评估。体检人群中脂肪肝常见酒精性脂肪肝和非酒精性脂肪肝,临床防治主要针对原发病因进行干预、调整饮食等综合措施[20]。因为不良生活习惯如长期饮酒导致并加重肝细胞内脂肪沉积,所以酒精性脂肪肝应该戒酒,以此可以改善脂肪肝的症状并降低相关风险[21]。因为经济社会发展、生活水平的提高,非酒精性脂肪肝越来越多,国内国外都逐渐成为常见的慢性肝脏疾病[22],其中最常见病因主要是肥胖和高脂血症,应该以控制饮食(低脂低糖饮食)和加强体育运动为主,达到减重、降脂的效果,降低脂肪肝的危害。精神压力和不良情绪等精神心理状态是身心疾病研究的切入点,所以保持良好心态对于防治脂肪肝同样重要[23]。超重或肥胖、血糖以及血脂代谢异常是导致脂肪肝的主要因素。在今后的临床科研中,应该扩大对脂肪肝的调查样本量和样本范围,继续观察健康干预对脂肪肝的影响,以期为临床、科研提供更加科学、客观的依据,达到积极防治脂肪肝的目的。

表4 不同性别脂肪肝、非脂肪肝与血糖、血脂异常等因素分析
[1] CLARK JM, DIEHL AM. Defining non-alcoholic fatty liver disease: implications for epidemiologic studies[J]. Gastroenterology, 2003, 124(1): 248-250.
[2] FAN JG, FARRELL GC. Epidemiology of non-alcoholic fatty liver disease in China[J]. J Hepatol, 2009, 50(1): 204-210.
[3] Joint Committee for Developing Chinese Guidelines on prevention and treatment of dyslipidemia in adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults[J]. Chin J Cardiol, 2007, 35(5): 390-419. (in Chinese)
中国成人血脂异常防治指南制订联合委员会. 中国成人血脂异常防治指南[J]. 中华心血管病杂志, 2007, 35(5): 390-419.
[4] Report of the expert committee on the diagnosis and classification of diabetes mellitus[J]. Diabetes Care, 1997(7): 1183-1197.
[5] Group of Fatty Liver and Alcoholic Liver Diseases, Society of Hepatology, Chinese Medical Association. Guidelines for management of non-alcoholic fatty liver disease[J]. J Clin Hepatol, 2010, 26(2): 120-124.(in Chinese)
中华医学会肝脏病学分会脂肪肝和酒精性肝病学组. 非酒精性脂肪性肝病诊疗指南[J]. 临床肝胆病杂志, 2010, 26(2): 120-124.
[6] FAN JG, YAN SY. Metabolic syndrome and fatty liver[J]. J Clin Hepatol, 2016, 32(3): 407-410. (in Chinese)
范建高, 颜士岩. 代谢综合征与脂肪肝[J]. 临床肝胆病杂志, 2016, 32(3): 407-410.
[7] ZHENG XY, WANG YH, LUO R, et al. Association research between metabolism syndrome and fatty liver of 5782 health examination cohort in Chongqing[J]. J Chongqing Med Univ, 2010, 35(5): 727-730. (in Chinese)
郑晓雅, 王永红, 罗蓉, 等. 重庆市5782例体检人群代谢综合征与脂肪肝的相关性研究[J].重庆医科大学学报, 2010, 35(5): 727-730.
[8] GU WG, FENG JY. Prevalence of nonalcoholic fatty liver disease in overweight and obese populations and related risk factors [J]. Gansu Med J, 2015, 34(2): 109-112. (in Chinese)
顾伟根, 冯静亚. 超重和肥胖人群非酒精性脂肪肝的流行现状及相关危险因素分析[J]. 甘肃医药, 2015, 34(2): 109-112.
[9] HE LY, GUO LJ. Metabolic features and adjustment of female blood lipids[J]. Clin Focus (Med J ), 2006, 21(23): 1689-1691. (in Chinese)
何立芸, 郭丽君. 女性血脂代谢特点及处理[J]. 临床荟萃, 2006, 21(23): 1689-1691.
[10] JIN P, DING YY, WANG BY, et al. Epidemiological survey of prevalence of fatty liver disease and its risk factors in urban population of northeast China[J]. Chin J Gastroenterol Hepatol, 2011, 20(7): 617-620, 623. (in Chinese)
金萍, 丁媛媛, 王炳元, 等. 东北地区城市脂肪肝的患病率及其危险因素的流行病学调查[J].胃肠病学和肝病学杂志, 2011, 20(7): 617-620, 623.
[11] WANG HW, ZOU CC, LI JH, et al. Risk factors for fatty liver disease and related nursing measures: an analysis of 8884 individuals undergoing physical examination in Shenzhen, China[J]. J Nurs, 2013, 20(5A): 38-41. (in Chinese)
王红卫, 邹长翠, 李瑾虹, 等. 深圳市8884例体检者脂肪肝危险因素分析及护理[J]. 护理学报, 2013, 20(5A): 38-41.
[12] CHEN QY. Analysis of the prevalence of fatty liver in shantou area[J]. Guangzhou Med J, 2014, 45(6): 72-75. (in Chinese)
陈秋妍. 汕头地区脂肪肝患病现状分析[J]. 广州医药, 2014, 45(6): 72-75.
[13] QIAO LN, DAI GR, ZHANG J, et al. An epidemiological survey of prevalence and risk factors for fatty liver disease in adults residing in Yan′an, China[J]. J Clin Hepatol, 2015, 10(1): 82-87. (in Chinese)
乔丽娜, 戴光荣, 张锦, 等. 延安地区成人脂肪肝患病率及其危险因素的探讨[J]. 临床肝胆病杂志, 2015, 10(1): 82-87.
[14] NIU CY, YAN R, TIAN Y, et al. The prevalence of fatty liver disease and its relationship with metabolic syndrome[J]. J Clin Hepatol, 2010, 26(2): 167-169.(in Chinese)
牛春燕, 闫蓉, 田宇, 等. 乌鲁木齐地区脂肪肝发病率及非酒精性脂肪肝与代谢综合征的关系[J]. 临床肝胆病杂志, 2010, 26(2): 167-169.
[15] XIE WB, WANG XL, LUO R, et al. The distribution of fatty liver diseases among adult residents in Chongqing by B-ultrasound[J]. J Chongqing Med Univ, 2010, 35(10): 1601-1603. (in Chinese)
谢微波, 王小林, 罗蓉, 等. 重庆市成人居民脂肪肝分布特点[J]. 重庆医科大学学报, 2010, 35(10): 1601-1603.
[16] FAN JG, ZHU J, LI XJ, et al. Epidemiological survey of prevalence of fatty liver and its risk factors in a general adult population of Shanghai[J]. Chin J Hepatol, 2005, 13(2): 83-88. (in Chinese)
范建高, 朱军, 李新建, 等. 上海市成人脂肪肝患病率及其危险因素流行病学调查[J]. 中华肝脏病杂志, 2005, 13(2): 83-88.
[17] LI N, SUN WH, YUAN ZH. Fatty liver of urban residents in Gan Zhou city and its risk factors analysis[J]. J Gannan Med Uni, 2013, 33(2): 273-275. (in Chinese)
李宁, 孙蔚华, 袁招红. 赣州市城镇居民脂肪肝患病率及其危险因素分析[J]. 赣南医学院学报, 2013, 33(2): 273-275.
[18] LI GH. Prevalence of fatty liver disease among residents in Shijiazhuang, China and related risk factors[D]. Hebei: Hebei Medical University, 2012. (in Chinese)
李桂红. 石家庄市人群脂肪性肝病流行率及相关因素研究[D]. 河北: 河北医科大学, 2012.
[19] ZHI LX, DUAN DS, HAN JW, et al. Prevalence of fatty liver disease in coastal towns in Hebei Province, China and related risk factors [J]. Hebei Med J, 2015, 37(1): 114-116. (in Chinese)
智利霞, 段冬生, 韩俊武, 等. 河北沿海城镇脂肪肝患病率及危险因素调查研究[J]. 河北医药, 2015, 37(1): 114-116.
[20] LI YP, ZHANG X. Risk factors for different degrees of fatty liver disease[J]. Mod Med Health, 2015, 31(14): 2167-2169. (in Chinese)
李艳萍, 张霞. 不同程度脂肪肝的相关危险因素分析[J]. 现代医药卫生, 2015, 31(14): 2167-2169.
[21] JIA Y, FU YJ, LIU XY, et al. Research progress of alcoholic fatty liver disease in China[J]. Chin J Gastroenterol Hepatol, 2014, 23(4): 376-379. (in Chinese)
贾艳, 付怡静, 刘晓阳, 等. 我国酒精性脂肪肝的研究进展[J]. 胃肠病学和肝病学杂志, 2014, 23(4): 376-379.
[22] AHMED MH, HUSAIN NE, ALMOBARAK AO .Non-alcoholic fatty liver disease and risk of diabetes and cardiovascular disease: what is important for primary care physicians[J]. J Family Med Prim Care, 2015, 4(1): 45-52.
[23] XIN SL, XU KS. A new understanding of the pathogenesis of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2017, 33(8): 1581-1583. (in Chinese)
辛晟梁, 徐可树. 非酒精性脂肪性肝病发病机制新认识[J]. 临床肝胆病杂志, 2017, 33(8): 1581-1583.
AninvestigationoftheprevalencerateoffattyliverdiseaseamongpeopleundergoingphysicalexaminationinTangshan,China
MENGYulin,ZHANGHaiyan,SONGBaoguo,etal.
(TheAffiliatedHospitalofNorthChinaUniversityofScienceandTechnology,Tangshan,Hebei063000,China)
ObjectiveTo investigate the prevalence rate of fatty liver disease among people undergoing physical examination in Tangshan, China, and to provide a reasonable basis for the prevention and treatment of fatty liver disease.MethodsThe clinical data of 12 808 individuals who underwent physical examination in Tangshan from March 2014 to February 2016 were collected, and among these individuals, 3540 had fatty liver disease. The data including age, sex, body mass index (BMI), fasting plasma glucose (FPG), total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), and liver ultrasound findings were analyzed. Thet-test was used for comparison of continuous data between groups and the chi-square test was used for comparison of categorical data between groups.Results
Of all 7151 male individuals who underwent physical examination, 2750 (38.46%) had fatty liver disease, and of all 5657 female individuals, 790 (13.96%) had fatty liver disease; there was a significant difference in the prevalence rate of fatty liver disease between male and female individuals (χ2=947.25,P<0.01). There was a significant difference in the detection rate of fatty liver disease between male and female individuals in each age group of 18-29, 30-39, 40-49, and ≥50 years (χ2=337.58, 474.06, 449.38, and 12.86, allP<0.01). There was a significant difference in the detection rate of fatty liver disease between male or female individuals with different BMIs [obese (BMI ≥28), overweight (24≤BMI<28), and normal (BMI<24)] (χ2=1104.01 and 500.23, bothP<0.01). In the three groups of obese (BMI ≥28), overweight (24≤BMI<28), and normal (BMI<24) individuals who underwent physical examination, there was a significant difference in the detection rate of fatty liver disease between male and female individuals in each group (χ2=71.24, 87.97, and 323.84, allP<0.01). Male and female individuals with obesity (BMI ≥28) and overweight (24≤BMI<28) had a significantly higher detection rate of fatty liver disease than those with normal BMI (bothP<0.01). There were significant differences in FPG, TC, TG, and LDL-C between the fatty liver group and the non-fatty liver group (t=17.482, 13.698, 22.133, and 27.334, allP<0.001). In male individuals who underwent physical examination, there were significant differences in FPG, TC, TG, and LDL-C between the individuals with and without fatty liver disease (t=11.288,8.652,11.671, and 20.118, allP<0.01); in female individuals, there were also significant differences in FPG, TC, TG, and LDL-C between the individuals with and without fatty liver disease (t=16.816, 5.532, 15.154, and 18.507, allP<0.01).ConclusionAmong the adults undergoing physical examination in Tangshan, male adults have a significantly higher prevalence rate of fatty liver disease than female adults. Overweight or obesity, hyperlipidemia, and abnormal glucose metabolism are major causes of fatty liver disease.
fatty liver; prevalence; data interpretation statistical
R575.5
A
1001-5256(2017)12-2376-05
10.3969/j.issn.1001-5256.2017.12.024
2017-08-15;修回日期:2017-09-05。 基金项目:唐山市科技局资助课题(14130217a);唐山市科技局资助课题(13130265Z) 作者简介:孟昱林(1979-),男,主治医师,主要从事中西医结合临床及研究工作。
引证本文:MENG YL, ZHANG HY, SONG BG, et al. An investigation of the prevalence rate of fatty liver disease among people undergoing physical examination in Tangshan, China[J]. J Clin Hepatol, 2017, 33(12): 2376-2380. (in Chinese)
孟昱林, 张海艳, 宋宝国, 等. 唐山市体检人群脂肪肝患病率调查分析[J]. 临床肝胆病杂志, 2017, 33(12): 2376-2380.
(本文编辑:林 姣)