The International Study Group of Pancreatic Surgery def i nition of delayed gastric emptying and the effects of various surgical modif i cations on the occurrence of delayed gastric emptying after pancreatoduodenectomy
2017-08-16RajeshPanwarandSujoyPal
Rajesh Panwar and Sujoy Pal
New Delhi, India
The International Study Group of Pancreatic Surgery def i nition of delayed gastric emptying and the effects of various surgical modif i cations on the occurrence of delayed gastric emptying after pancreatoduodenectomy
Rajesh Panwar and Sujoy Pal
New Delhi, India
BACKGROUND:A number of def i nitions have been used for delayed gastric emptying (DGE) after pancreatoduodenectomy and the reported rates varied widely. The International Study Group of Pancreatic Surgery (ISGPS) def i nition is the current standard but it is not used universally. In this comprehensive review, we aimed to determine the acceptance rate of ISGPS def i nition of DGE, the incidence of DGE after pancreatoduodenectomy and the effect of various technical modif i cations on its incidence.
DATA SOURCE:We searched PubMed for studies regarding DGE after pancreatoduodenectomy that were published from 1 January 1980 to 1 July 2015 and extracted data on DGE def i nition, DGE rates and comparison of DGE rates among different technical modif i cations from all of the relevant articles.
RESULTS:Out of 435 search results, 178 were selected for data extraction. The ISGPS def i nition was used in 80% of the studies published since 2010 and the average rates of DGE and clinically relevant DGE were 27.7% (range: 0-100%; median: 18.7%) and 14.3% (range: 1.8%-58.2%; median: 13.6%), respectively. Pylorus preservation or retrocolic reconstruction were not associated with increased DGE rates. Although pyloric dilatation, Braun’s entero-enterostomy and Billroth II reconstruction were associated with signif i cantly lower DGE rates, pyloric ring resection appears to be most promising with favorable results in 7 out of 10 studies.
CONCLUSIONS:ISGPS def i nition of DGE has been used in majority of studies published after 2010. Clinically relevant DGE rates remain high at 14.3% despite a number of proposed surgical modif i cations. Pyloric ring resection seems to offer the most promising solution to reduce the occurrence of DGE.
(Hepatobiliary Pancreat Dis Int 2017;16:353-363)
pancreatoduodenectomy; delayed gastric emptying; ISGPS def i nition; pyloric ring resection
Introduction
Pancreatoduodenectomy (PD) is a complex surgical procedure which is indicated for malignant lower end biliary obstruction, malignant pancreatic head tumors and certain benign conditions like chronic pancreatitis and cystic neoplasms of pancreas. The procedure has greatly evolved since its initial description and has become a reasonably safe procedure with mortality rate of less than 5% in high volume centers but it is still associated with signif i cant morbidity.[1,2]
Although post-operative pancreatic fi stula is the most dreaded complication after PD, delayed gastric emptying (DGE) remains the most common complication.[1,2]DGE, although not imminently life threatening, is an annoying complication which causes signif i cant discomfort and results in prolongation of hospital stay and readmission and thus increased hospital costs.[3,4]Pathophysiology of DGE has not been completely understood but itsoccurrence has been related to a number of factors like functional obstruction caused by stomach dysrhythmia due to vagal denervation and disruption of neural connections between stomach and intestine, absence of motilin due to duodenal resection and improper alignment after reconstruction for primary DGE and the development of other complications such as pancreatic anastomotic failure or retrogastric collection for secondary DGE.[5-7]A number of modif i cations in the reconstructive technique have been proposed in order to decrease the incidence of DGE. In this review, we attempted to assess the magnitude of the problem due to DGE and investigate the effect of various technical modif i cations in the surgical technique on the occurrence of DGE.
Methods
We searched PubMed for relevant articles published from 1 January 1980 to 1 July 2015 with “pancreatoduodenectomy/pancreaticoduodenectomy/Whipple procedure” AND“delayed gastric emptying/DGE/gastroparesis” as the search terms. The studies meeting the following criteria were included: 1) human studies; 2) English language; 3) DGE rates clearly mentioned; 4) minimum of 50 PDs (only for DGE rate calculation, not applicable for relevant comparative studies).
The initial search revealed 435 studies (Fig.). Out of these, 2 duplicate studies were removed and 211 studies were excluded after title and abstract review. Out of the remaining 222 studies, 44 were excluded after fulltext review. Relevant articles were further selected for individual queries (mentioned under respective headings). In case there were multiple studies from the same center or author with overlapping patients, we selected the study with higher number of cases or higher quality depending on the needs of the given query. A total of 178 studies were included in this review. Data collected from each of the study included name of fi rst author, institution, year of publication, study period, def i nition of DGE, technique of PD, comparison groups, number of cases (overall and each group), number of patients with DGE (overall and each group) and grade wise distribution of DGE (for the International Study Group for Pancreatic Surgery def i nition only). In order to provide a comprehensive picture of the published literature, we did not attempt to reject studies on the basis of heterogeneity or the risk of bias. Also, we did not attempt to do a metaanalysis as there are already several published systematic reviews and meta-analyses for each query that has been discussed in this review. Except for the calculation of DGE rates, where pooled data was used, data from the selected studies have been presented and interpreted individually. Wherever available, the results of systematic reviews and meta-analyses have also been presented separately. APvalue of <0.05 was considered statistically signif i cant. ThePvalue was calculated using Chi-square or Fisher’s exact test as applicable in case it was not mentioned in the included study.
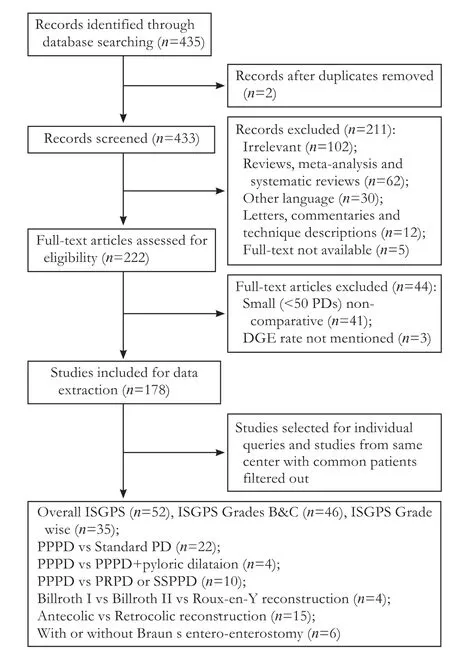
Fig. Flow diagram of studies selection.
Current def i nition and classif i cation of DGE
DGE or gastroparesis occurs due to impaired motor function of the stomach which clinically presents as vomiting, high nasogastric tube output or intolerance to oral diet. Many def i nitions of DGE have been reported in literature and most of them are based on the time to nasogastric tube removal or time to resumption of oral diet (Table 1).[4,8-28]There are considerable differences among these def i nitions which makes the comparisons across studies impossible. The International Study Group of Pancreatic Surgery (ISGPS) def i ned DGE as the requirement or re-insertion of nasogastric tube after postoperative day 3 or failure to resume oral diet by postoperative day 7.[29]The ISGPS def i nition further divided DGE into grades A, B and C in order of increasing severity. Wetried to fi nd out the acceptance rate of ISGPS def i nition from the studies published from 2010 to 2015. Out of all included studies, 97 were published in or after 2010 and ISGPS def i nition was used in 63. Another 16 studies used modif i ed ISGPS (only grades B and C). Thus, ISGPS def i nition was used to calculate DGE rates in more than 80% of the studies published in or after 2010.
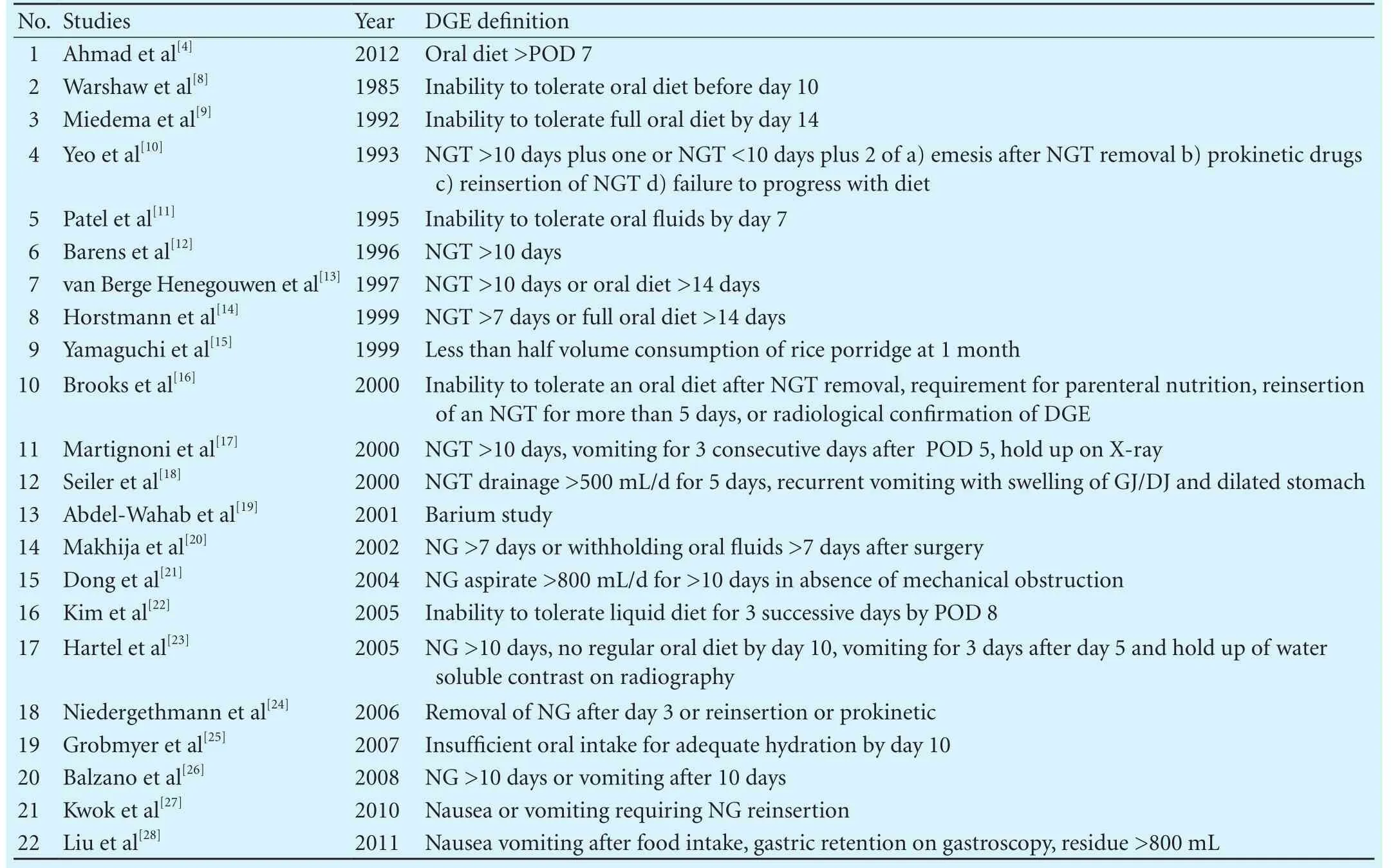
Table 1. Def i nitions of DGE used by different studies
Incidence of DGE after PD
There is a wide variation in the incidence of DGE after PD because of the heterogeneity in the surgical technique as well as the def i nition of DGE. The reported incidence of DGE in studies including 500 or more PDs ranges from 3.2% to 59.0% (Table 2).[1,2,4,6,15,26,30-36]The def i nition of DGE varies among these studies. Using our search strategy, we looked at all the studies which included 50 or more PDs and had def i ned DGE according to the ISGPS classif i cation. We compiled data from 52 studies with 11669 PDs. DGE occurred in 3234 cases with an average incidence of 27.7% (range: 0-100%; median: 18.7%). Among these, 35 studies with 8124 PDs had information regarding overall incidence of DGE (2589 cases; 31.9%) as well as individual grades of DGE with grade A in 1499 (18.5%), grade B in 589 (7.3%) and grade C in 501 (6.2%) patients.
Many authors consider only grades B and C DGE to be clinically relevant and some do not even mention the rates of grade A DGE.[37,38]The mean incidence of clinically relevant DGE (grades B and C) in 46 studies with 10013 cases was 14.3% (range: 1.8%-58.2%; median: 13.6%).
Thus, there is a wide variation in the reported DGE rates even after standardization of the def i nition of DGE. Some of this variation may be explained by the fact that some centers routinely keep nasogastric tube for >3 days and thus all patients would qualify for grade A DGE. However, the variation in DGE incidence persists even if we exclude grade A DGE.
Surgical techniques and DGE
PPPD vs standard PD
Pylorus preserving pancreatoduodenectomy (PPPD) was reintroduced in order to decrease the morbidity of standard PD. Although pylorus preservation provides some short-term and long-term advantages over the standardPD, the initial reports suggested a higher incidence of DGE.[8]A number of studies have been conducted to address this issue. We found 4 randomized controlled trials (RCTs), 3 prospective non-randomized study and 15 retrospective studies that compared DGE rates between PPPD and standard PD, out of which 2 RCTs and 5 retrospective studies found higher incidence of DGE after PPPD (Table 3).[8,11,13,18,20,22,24,27,39-52]However, there was no difference in the DGE rates between PPPD and standard PD in a Cochrane review by Diener et al[53]which included 203 PPPD and 209 standard PD patients from 5 RCTs.

Table 2. Reported incidence of DGE in the various retrospective series of PD with more than 500 cases
Pylorus and DGE
The increased DGE rates after PPPD were because of pylorospasm.[22]Hence, modif i cations like pyloromyotomy or pyloric dilatation and pylorus resection were introduced. One prospective non-randomized and 3 retrospective studies compared DGE incidence between PPPD and PPPD with pyloric dilatation (Table 4).[22,54-56]Pyloric dilatation was associated with signif i cantly reduced incidence of DGE as compared to PPPD alone in all the four studies.
The concept of pyloric ring resection was introduced to preserve the reservoir function of the stomach and simultaneously tackle the problem of pylorospasm without the need for pyloromyotomy or pyloric dilatation. As compared to PPPD in which the fi rst part of duodenum is divided thus preserving whole of the stomach, pylorus and proximal duodenum, in pylorus resecting pancreatoduodenectomy (PRPD) or subtotal stomach preserving pancreatoduodenectomy (SSPPD), the stomach is divided 2 to 3 cm proximal to the pylorus. Three RCTs and 7 retrospective studies compared DGE rates after PPPD and PRPD or SSPPD (Table 5).[49,57-65]PRPD was associated with signif i cantly lower DGE rates in 1 RCT and 6 retrospective studies. The main drawback of the published RCTs is the small sample size which may not be suff i ciently powered to detect a smaller benef i t. We also found 3 meta-analyses aimed at investigating the differences in DGE rates after PPPD and PRPD.[64,66,67]All 3 meta-analyses found a lower incidence of DGE after PRPD. However, most of these results are based on retrospective studies and a few RCTs which are mostly from Japan. Thus, although the available data favors PRPD, further high quality randomized trials are needed to validate the above observations.
It is interesting that although the higher incidence of DGE in PPPD has not been proven, the resection or dilatation of pylorus has been associated with decreased DGE rates. Does this mean that PRPD or SSPPD has lower incidence of DGE as compared to standard PD as well? This question remains unanswered at present, however, theoretically PRPD may preserve the motor innervation to the body of stomach and which along with the absence of pylorus may actually hasten the gastric emptying.
Billroth I vs Billroth II vs Roux-en-Y reconstruction
Billroth I reconstruction is believed to be more physiological because the sequence of anastomoses is similar to the normal anatomy. However, all the three anatomoses lie in very close proximity due to limitation
of available space which could impair gastric emptying. Billroth II and Roux-en-Y reconstructions, on the other hand, place the gastrojejunal anastomosis away from the pancreatic and biliary anastomosis. Thus, theoretically Billroth I reconstruction may be associated with higher risk of DGE. From the selected studies, we searched for studies that compared DGE rates between Billroth I, Billroth II and Roux-en-Y construction. We found 3 retrospective studies,[68-70]all of which found signif icantly higher DGE rates with Billroth I reconstruction as compared to Billroth II reconstruction in two studies and Roux-en-Y reconstruction in one study. One RCT[71]found signif i cantly higher DGE rates with Roux-en-Y as compared to Billroth II reconstruction (Table 6). Thus, published data suggest that Billroth II reconstruction is associated with lower incidence of DGE as compared to Billroth I or Roux-en-Y reconstruction.
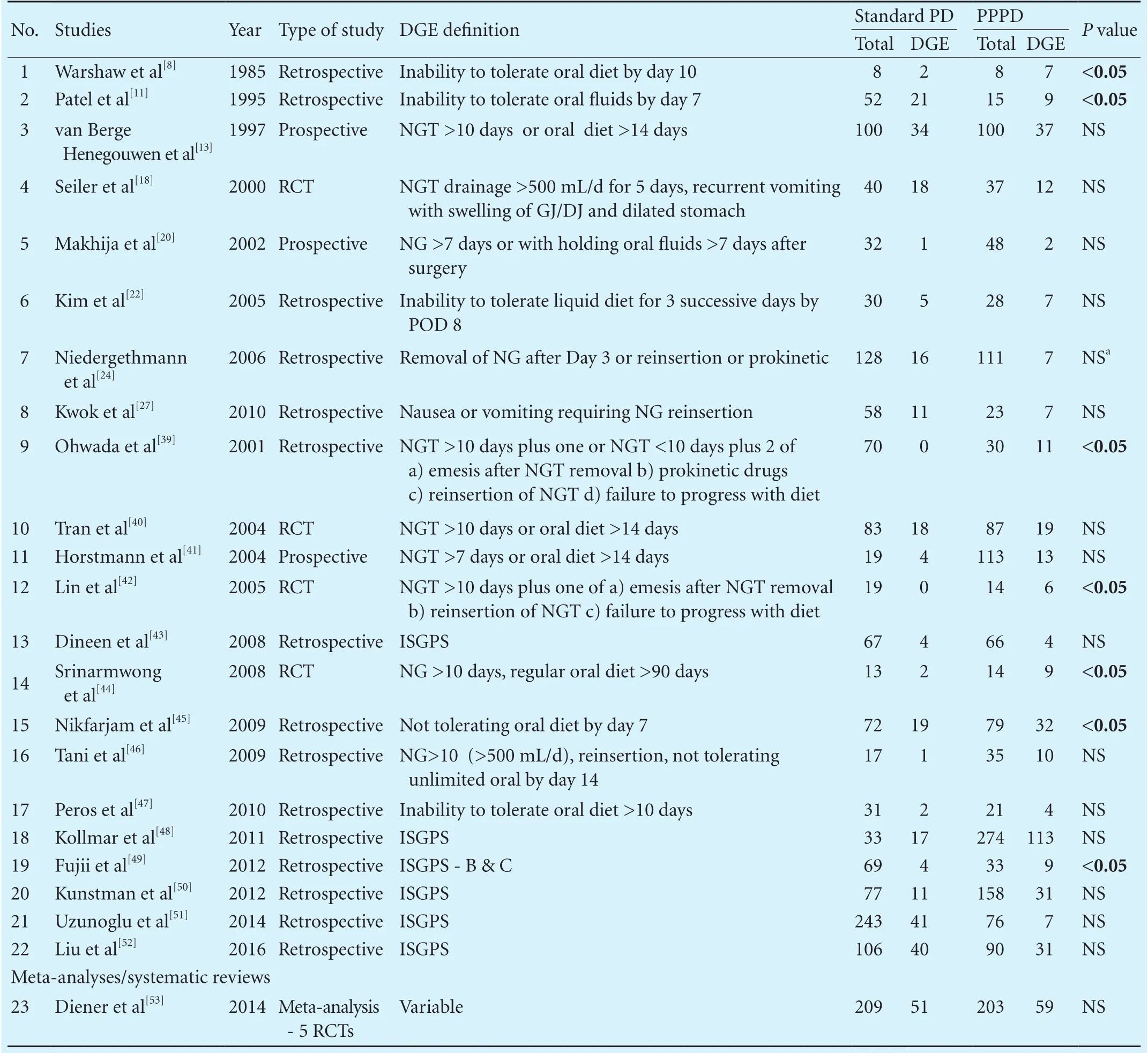
Table 3. Studies comparing DGE rates between standard PD and PPPD

Table 4. Studies comparing DGE rates between PPPD and PPPD with pyloric dilatation
Antecolic vs retrocolic gastrojejunal anastomosis
Antecolic route for gastrojejunostomy has been considered superior to retrocolic route with regard to DGE rates. Antecolic route has some theoretical advantages such as presence of colon between pancreato-enteric and gastrojejunal anastomoses which may obviate the negative impact of minor pancreatic anastomotic leak on gastric emptying. Further, there are less chances of angulation or kinking of gastrojejunostomy and there is no venous congestion in the jejunal loop due to absence of compression effect of mesocolon. From the selected studies, we searched for the studies that had compared DGE rates after antecolic or retrocolic reconstruction. We found 7 RCTs and 8 retrospective studies[1,23,36,45,72-82]that compared DGE rates between antecolic and retrocolic reconstruction. Antecolic route was associated with lower incidence of DGE as compared to retrocolic routein 2 RCTs and 6 retrospective studies (Table 7). Although a meta-analysis published in 2012[83]found antecolic route to be superior to retrocolic regarding DGE rates, majority of studies included in this meta-analysis were non-randomized. A subsequent meta-analysis which included only RCTs failed to show any signif i cant effect of reconstruction route on the incidence of DGE after PD.[84]Our experience has been similar and we believe that the anterior or posterior location of the gastrojejunostomy has little role in the genesis or prevention of DGE.[76]

Table 5. Studies comparing DGE rates between PPPD and PRPD or SSPPD
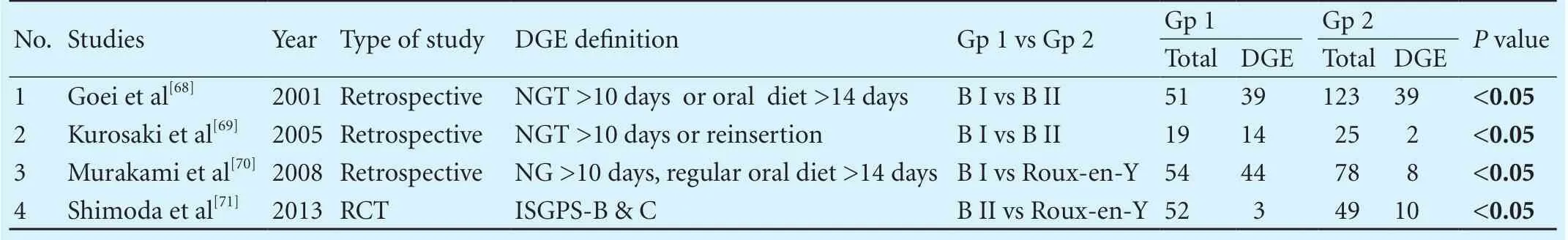
Table 6. Studies comparing DGE rates between Billroth I, Billroth II and Roux-en-Y reconstruction
Braun’s entero-enterostomy
Bile ref l ux into stomach has also been thought to be involved in the pathogenesis of DGE.[85]Braun’s technique involves an additional jejuno-jejunal anastomosis between the afferent and efferent loop of gastrojejunostomy in order to divert alkaline bile away from the stomach and thus may decrease DGE rates. We searched the selected studies comparing DGE rates after reconstruction with or without Braun’s entero-enterostomy. We found 6 retrospective studies (Table 8)[52,85-89]and Braun’ s entero-enterostomy was associated with signif i-cantly lower incidence of DGE in four studies and higher incidence in one study. A recent meta-analysis also found that Braun’s entero-enterostomy had signif i cantly lower rate of clinically relevant DGE (grades B and C), however, there was no difference in the incidence of overall DGE (grades A, B and C).[90]

Table 7. Studies comparing DGE rates between antecolic and retrocolic reconstruction
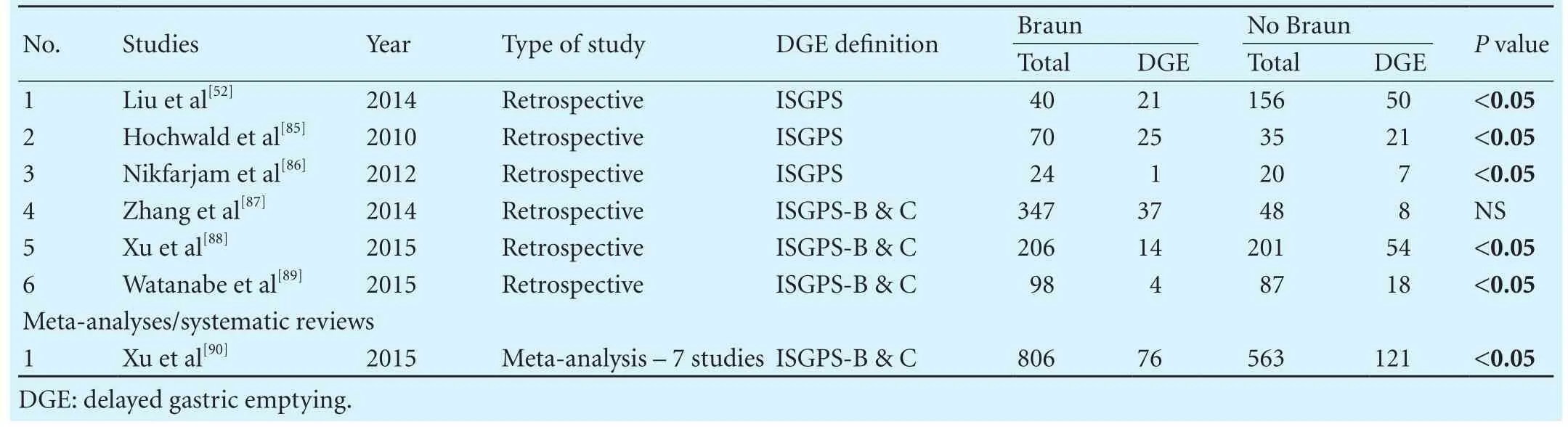
Table 8. Studies comparing DGE rates between Braun’s and no Braun’s entero-enterostomy
Other modif i cations
A number of other modif i cations like stapled gastrojejunostomy[91-93], double Roux-en-Y reconstruction[51], omental wrapping[94], preservation of left gastric vein to prevent venous congestion[95]and preservation of right gastric artery and innervations along lesser curvature in order to prevent ischemia of the pyloroduodenal complex and maintain antro-pyloric pump mechanism[96]have been attempted by various authors in order to decrease DGE. These are mostly retrospective case series from one or two centers and results have not been repeated by others.
Conclusions
DGE is the most common complication following PD[1,2]and results in signif i cant patient discomfort, increased hospital stay and costs. ISGPS def i nition of DGE has been used in majority of studies published after 2010. There is a wide variation in the reported incidence rates despite standardization of the def i nition by the ISGPS. Grade A DGE is usually not clinically signif i cant. There may be a case to exclude grade A DGE and to consider only clinically signif i cant (grades B and C) DGE as an outcome measure for comparative trials.
The initial concern of increased incidence of DGE after PPPD as compared to standard PD has not been proven conclusively. Pyloric dilatation, Billroth II reconstruction and Braun’s entero-enterostomy have been found to be associated with decreased incidence of DGE but these results are mostly based on retrospective data and hence should be interpreted with caution. Although the superiority of antecolic reconstruction over retrocolic reconstruction with regards to DGE has been shown in retrospective studies, the randomized trials have failed to demonstrate a clear advantage. Thus, it is very diff i cult to draw any meaningful conclusion from the available literature to categorically prove or reject the benef i t of surgical modif i cations like pyloric dilatation, Billroth II reconstruction, Braun’s entero-enterostomy and antecolic reconstruction. Pyloric ring resection was associated with signif i cantly lower DGE rates in 7 out of 10 studies and 3 meta-analyses. The good results of most of the other technical modif i cations (e.g. stapled gastrojejunostomy, double Roux-en-Y reconstruction etc.) have not yet been repeated.
Thus, DGE remains a tenacious problem and the solution remains elusive despite constant efforts on the part of hepato-pancreato-biliary surgeons. Pyloric ring resection seems to be the most promising surgical modifi cation but needs to be tested in high quality randomized trials with suf fi cient sample size.
Contributors: PR proposed the study. PR and PS performed the search and wrote the fi rst draft. PR extracted and analyzed the data. Both authors contributed to the design and interpretation of the study and to further drafts. PR is the guarantor.
Funding: None.
Ethical approval: Not needed.
Competing interest: No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 El Nakeeb A, Askr W, Mahdy Y, Elgawalby A, El Sorogy M, Abu Zeied M, et al. Delayed gastric emptying after pancreaticoduodenectomy. Risk factors, predictors of severity and outcome. A single center experience of 588 cases. J Gastrointest Surg 2015;19:1093-1100.
2 Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg 2015;220:530-536.
3 Malleo G, Crippa S, Butturini G, Salvia R, Partelli S, Rossini R, et al. Delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy: validation of International Study Group of Pancreatic Surgery classif i cation and analysis of risk factors. HPB (Oxford) 2010;12:610-618.
4 Ahmad SA, Edwards MJ, Sutton JM, Grewal SS, Hanseman DJ, Maithel SK, et al. Factors inf l uencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg 2012;256:529-537.
5 Kang CM, Lee JH. Pathophysiology after pancreaticoduodenectomy. World J Gastroenterol 2015;21:5794-5804.
6 Parmar AD, Sheff i eld KM, Vargas GM, Pitt HA, Kilbane EM, Hall BL, et al. Factors associated with delayed gastric emptying after pancreaticoduodenectomy. HPB (Oxford) 2013;15:763-772.
7 Courvoisier T, Donatini G, Faure JP, Danion J, Carretier M, Richer JP. Primary versus secondary delayed gastric emptying (DGE) grades B and C of the International Study Group of Pancreatic Surgery after pancreatoduodenectomy: a retrospective analysis on a group of 132 patients. Updates Surg 2015;67:305-309.
8 Warshaw AL, Torchiana DL. Delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy. Surg Gynecol Obstet 1985;160:1-4.
9 Miedema BW, Sarr MG, van Heerden JA, Nagorney DM, McIlrath DC, Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg 1992;127:945-950.
10 Yeo CJ, Barry MK, Sauter PK, Sostre S, Lillemoe KD, Pitt HA, et al. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebocontrolled trial. Ann Surg 1993;218:229-238.
11 Patel AG, Toyama MT, Kusske AM, Alexander P, Ashley SW, Reber HA. Pylorus-preserving Whipple resection for pancreatic cancer. Is it any better? Arch Surg 1995;130:838-843.
12 Barens SA, Lillemoe KD, Kaufman HS, Sauter PK, Yeo CJ, Talamini MA, et al. Pancreaticoduodenectomy for benign disease. Am J Surg 1996;171:131-135.
13 van Berge Henegouwen MI, van Gulik TM, DeWit LT, Allema JH, Rauws EA, Obertop H, et al. Delayed gastric emptying after standard pancreaticoduodenectomy versus pylorus-preserving pancreaticoduodenectomy: an analysis of 200 consecutive patients. J Am Coll Surg 1997;185:373-379.
14 Horstmann O, Becker H, Post S, Nustede R. Is delayed gastric emptying following pancreaticoduodenectomy related to pylorus preservation? Langenbecks Arch Surg 1999;384:354-359.
15 Yamaguchi K, Tanaka M, Chijiiwa K, Nagakawa T, Imamura M, Takada T. Early and late complications of pylorus-preserving pancreatoduodenectomy in Japan 1998. J Hepatobiliary Pancreat Surg 1999;6:303-311.
16 Brooks AD, Marcus SG, Gradek C, Newman E, Shamamian P, Gouge TH, et al. Decreasing length of stay after pancreatoduodenectomy. Arch Surg 2000;135:823-830.
17 Martignoni ME, Friess H, Sell F, Ricken L, Shrikhande S, Kulli C, et al. Enteral nutrition prolongs delayed gastric emptying in patients after Whipple resection. Am J Surg 2000;180:18-23.
18 Seiler CA, Wagner M, Sadowski C, Kulli C, Büchler MW. Randomized prospective trial of pylorus-preserving vs. classic duodenopancreatectomy (Whipple procedure): initial clinical results. J Gastrointest Surg 2000;4:443-452.
19 Abdel-Wahab M, Sultan A, elGwalby N, Fathy O, AboElenen A, Zied MA, et al. Modif i ed pancreaticoduodenectomy: experience with 81 cases, Wahab modif i cation. Hepatogastroenterology 2001;48:1572-1576.
20 Makhija R, Tsai P, Kingsnorth A. Pylorus-preserving pancreatoduodenectomy with Billroth I type reconstruction: a viable option for pancreatic head resection. J Hepatobiliary Pancreat Surg 2002;9:614-619.
21 Dong K, Li B, Guan QL, Huang T. Analysis of multiple factors of postsurgical gastroparesis syndrome after pancreaticoduodenectomy and cryotherapy for pancreatic cancer. World J Gastroenterol 2004;10:2434-2438.
22 Kim DK, Hindenburg AA, Sharma SK, Suk CH, Gress FG, Staszewski H, et al. Is pylorospasm a cause of delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? Ann Surg Oncol 2005;12:222-227.
23 Hartel M, Wente MN, Hinz U, Kleeff J, Wagner M, Müller MW, et al. Effect of antecolic reconstruction on delayed gastric emptying after the pylorus-preserving Whipple procedure. Arch Surg 2005;140:1094-1099.
24 Niedergethmann M, Shang E, Farag Soliman M, Saar J, Berisha S, Willeke F, et al. Early and enduring nutritional and functional results of pylorus preservation vs classic Whipple procedure for pancreatic cancer. Langenbecks Arch Surg 2006;391:195-202.
25 Grobmyer SR, Pieracci FM, Allen PJ, Brennan MF, Jaques DP. Def i ning morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J Am Coll Surg 2007;204:356-364.
26 Balzano G, Zerbi A, Braga M, Rocchetti S, Beneduce AA, Di Carlo V. Fast-track recovery programme after pancreaticoduodenectomy reduces delayed gastric emptying. Br J Surg 2008;95:1387-1393.
27 Kwok KH, Rizk J, Coleman M, Fenton-Lee D. Pancreaticoduodenectomy - outcomes from an Australian institution. ANZ J Surg 2010;80:605-608.
28 Liu C, Du Z, Lou C, Wu C, Yuan Q, Wang J, et al. Enteral nutrition is superior to total parenteral nutrition for pancreatic cancer patients who underwent pancreaticoduodenectomy. Asia Pac J Clin Nutr 2011;20:154-160.
29 Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested def i nition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007;142:761-768.
30 Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, et al. Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg 2004;139:718-727.
31 Welsch T, Borm M, Degrate L, Hinz U, Büchler MW, Wente MN. Evaluation of the International Study Group of Pancreatic Surgery def i nition of delayed gastric emptying after pancreatoduodenectomy in a high-volume centre. Br J Surg 2010;97:1043-1050.
32 Hashimoto Y, Traverso LW. Incidence of pancreatic anastomotic failure and delayed gastric emptying after pancreatoduodenectomy in 507 consecutive patients: use of a web-based calculator to improve homogeneity of def i nition. Surgery 2010;147:503-515.
33 Shrikhande SV, Barreto SG, Somashekar BA, Suradkar K, Shetty GS, Talole S, et al. Evolution of pancreatoduodenectomy in a tertiary cancer center in India: improved results from service reconf i guration. Pancreatology 2013;13:63-71.
34 Burkhart RA, Relles D, Pineda DM, Gabale S, Sauter PK, Rosato EL, et al. Def i ning treatment and outcomes of hepaticojejunostomy failure following pancreaticoduodenectomy. J Gastrointest Surg 2013;17:451-460.
35 Beane JD, House MG, Miller A, Nakeeb A, Schmidt CM, Zyromski NJ, et al. Optimal management of delayed gastric emptying after pancreatectomy: an analysis of 1089 patients. Surgery 2014;156:939-946.
36 Sahora K, Morales-Oyarvide V, Thayer SP, Ferrone CR, Warshaw AL, Lillemoe KD, et al. The effect of antecolic versus retrocolic reconstruction on delayed gastric emptying after classic non-pylorus-preserving pancreaticoduodenectomy. Am J Surg 2015;209:1028-1035.
37 Meng HB, Zhou B, Wu F, Xu J, Song ZS, Gong J, et al. Continuous suture of the pancreatic stump and Braun enteroenterostomy in pancreaticoduodenectomy. World J Gastroenterol 2015;21:2731-2738.
38 Eshuis WJ, de Bree K, Sprangers MA, Bennink RJ, van Gulik TM, Busch OR, et al. Gastric emptying and quality of life after pancreatoduodenectomy with retrocolic or antecolic gastroenteric anastomosis. Br J Surg 2015;102:1123-1132.
39 Ohwada S, Ogawa T, Kawate S, Tanahashi Y, Iwazaki S, Tomizawa N, et al. Results of duct-to-mucosa pancreaticojejunostomy for pancreaticoduodenectomy Billroth I type reconstruction in 100 consecutive patients. J Am Coll Surg 2001;193:29-35.
40 Tran KT, Smeenk HG, van Eijck CH, Kazemier G, Hop WC, Greve JW, et al. Pylorus preserving pancreaticoduodenectomy versus standard Whipple procedure: a prospective, randomized, multicenter analysis of 170 patients with pancreatic and periampullary tumors. Ann Surg 2004;240:738-745.
41 Horstmann O, Markus PM, Ghadimi MB, Becker H. Pylorus preservation has no impact on delayed gastric emptying afterpancreatic head resection. Pancreas 2004;28:69-74.
42 Lin PW, Shan YS, Lin YJ, Hung CJ. Pancreaticoduodenectomy for pancreatic head cancer: PPPD versus Whipple procedure. Hepatogastroenterology 2005;52:1601-1604.
43 Dineen SP, Roland CL, Schwarz RE. Pancreatoduodenectomy with or without pyloric preservation: a clinical outcomes comparison. HPB Surg 2008;2008:719459.
44 Srinarmwong C, Luechakiettisak P, Prasitvilai W. Standard whipple’s operation versus pylorus preserving pancreaticoduodenectomy: a randomized controlled trial study. J Med Assoc Thai 2008;91:693-698.
45 Nikfarjam M, Kimchi ET, Gusani NJ, Shah SM, Sehmbey M, Shereef S, et al. A reduction in delayed gastric emptying by classic pancreaticoduodenectomy with an antecolic gastrojejunal anastomosis and a retrogastric omental patch. J Gastrointest Surg 2009;13:1674-1682.
46 Tani M, Kawai M, Hirono S, Ina S, Miyazawa M, Fujita Y, et al. Pylorus-preserving pancreaticoduodenectomy versus conventional pancreaticoduodenectomy for pancreatic adenocarcinoma. Surg Today 2009;39:219-224.
47 Peros G, Giannopoulos GA, Christodoulou S, Konstantoudakis G, Petropoulou K, Sakorafas GH. Good results after major pancreatic resections in a middle-volume center. Pancreas 2010;39:411-414.
48 Kollmar O, Sperling J, Moussavian MR, Kubulus D, Richter S, Schilling MK. Delayed gastric emptying after pancreaticoduodenectomy: inf l uence of the orthotopic technique of reconstruction and intestinal motilin receptor expression. J Gastrointest Surg 2011;15:1158-1167.
49 Fujii T, Kanda M, Kodera Y, Nagai S, Sahin TT, Hayashi M, et al. Preservation of the pyloric ring has little value in surgery for pancreatic head cancer: a comparative study comparing three surgical procedures. Ann Surg Oncol 2012;19:176-183.
50 Kunstman JW, Fonseca AL, Ciarleglio MM, Cong X, Hochberg A, Salem RR. Comprehensive analysis of variables affecting delayed gastric emptying following pancreaticoduodenectomy. J Gastrointest Surg 2012;16:1354-1361.
51 Uzunoglu FG, Reeh M, Wollstein R, Melling N, Perez D, Vashist YK, et al. Single versus double Roux-en-Y reconstruction techniques in pancreaticoduodenectomy: a comparative singlecenter study. World J Surg 2014;38:3228-3234.
52 Liu QY, Li L, Xia HT, Zhang WZ, Cai SW, Lu SC. Risk factors of delayed gastric emptying following pancreaticoduodenectomy. ANZ J Surg 2016;86:69-73.
53 Diener MK, Fitzmaurice C, Schwarzer G, Seiler CM, Hüttner FJ, Antes G, et al. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev 2014;11:CD006053.
54 Fischer CP, Hong JC. Method of pyloric reconstruction and impact upon delayed gastric emptying and hospital stay after pylorus-preserving pancreaticoduodenectomy. J Gastrointest Surg 2006;10:215-219.
55 Manes K, Lytras D, Avgerinos C, Delis S, Dervenis C. Antecolic gastrointestinal reconstruction with pylorus dilatation. Does it improve delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? HPB (Oxford) 2008;10:472-476.
56 Uravić M, Zelić M, Petrošić N, Tokmadžić VS, Stimac D, Sustić A. Effect of pyloric dilatation on gastric emptying after pylorus-preserving pancreaticoduodenectomy. Hepatogastroenterology 2011;58:2144-2147.
57 Hayashibe A, Kameyama M, Shinbo M, Makimoto S. The surgical procedure and clinical results of subtotal stomach preserving pancreaticoduodenectomy (SSPPD) in comparison with pylorus preserving pancreaticoduodenectomy (PPPD). J Surg Oncol 2007;95:106-109.
58 Akizuki E, Kimura Y, Nobuoka T, Imamura M, Nishidate T, Mizuguchi T, et al. Prospective nonrandomized comparison between pylorus-preserving and subtotal stomach-preserving pancreaticoduodenectomy from the perspectives of DGE occurrence and postoperative digestive functions. J Gastrointest Surg 2008;12:1185-1192.
59 Kurahara H, Takao S, Shinchi H, Mataki Y, Maemura K, Sakoda M, et al. Subtotal stomach-preserving pancreaticoduodenectomy (SSPPD) prevents postoperative delayed gastric emptying. J Surg Oncol 2010;102:615-619.
60 Oida T, Mimatsu K, Kano H, Kawasaki A, Kuboi Y, Fukino N, et al. Preventing delayed gastric emptying in pancreaticogastrostomy by a modif i ed subtotal-stomach-preserving pancreaticoduodenectomy: Oida modif i cation. Hepatogastroenterology 2011;58:1384-1388.
61 Kawai M, Tani M, Hirono S, Miyazawa M, Shimizu A, Uchiyama K, et al. Pylorus ring resection reduces delayed gastric emptying in patients undergoing pancreatoduodenectomy: a prospective, randomized, controlled trial of pylorus-resecting versus pylorus-preserving pancreatoduodenectomy. Ann Surg 2011;253:495-501.
62 Hackert T, Hinz U, Hartwig W, Strobel O, Fritz S, Schneider L, et al. Pylorus resection in partial pancreaticoduodenectomy:impact on delayed gastric emptying. Am J Surg 2013;206:296-299.
63 Nanashima A, Abo T, Sumida Y, Tobinaga S, Nonaka T, Takeshita H, et al. Comparison of results between pyloruspreserving pancreaticoduodenectomy and subtotal stomachpreserving pancreaticoduodenectomy: report at a single cancer institute. Hepatogastroenterology 2013;60:1182-1188.
64 Zhou Y, Lin L, Wu L, Xu D, Li B. A case-matched comparison and meta-analysis comparing pylorus-resecting pancreaticoduodenectomy with pylorus-preserving pancreaticoduodenectomy for the incidence of postoperative delayed gastric emptying. HPB (Oxford) 2015;17:337-343.
65 Matsumoto I, Shinzeki M, Asari S, Goto T, Shirakawa S, Ajiki T, et al. A prospective randomized comparison between pylorusand subtotal stomach-preserving pancreatoduodenectomy on postoperative delayed gastric emptying occurrence and longterm nutritional status. J Surg Oncol 2014;109:690-696.
66 Huang W, Xiong JJ, Wan MH, Szatmary P, Bharucha S, Gomatos I, et al. Meta-analysis of subtotal stomach-preserving pancreaticoduodenectomy vs pylorus preserving pancreaticoduodenectomy. World J Gastroenterol 2015;21:6361-6373.
67 Hanna MM, Gadde R, Tamariz L, Allen CJ, Meizoso JP, Sleeman D, et al. Delayed gastric emptying after pancreaticoduodenectomy: is subtotal stomach preserving better or pylorus preserving? J Gastrointest Surg 2015;19:1542-1552.
68 Goei TH, van Berge Henegouwen MI, Slooff MJ, van Gulik TM, Gouma DJ, Eddes EH. Pylorus-preserving pancreatoduodenectomy: inf l uence of a Billroth I versus a Billroth II type of reconstruction on gastric emptying. Dig Surg 2001;18:376-380.
69 Kurosaki I, Hatakeyama K. Clinical and surgical factors inf l uencing delayed gastric emptying after pyloric-preserving pancreaticoduodenectomy. Hepatogastroenterology 2005;52:143-148.
70 Murakami Y, Uemura K, Sudo T, Hayashidani Y, Hashimoto Y, Nakagawa N, et al. An antecolic Roux-en Y type reconstruction decreased delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Gastrointest Surg 2008;12:1081-1086.
71 Shimoda M, Kubota K, Katoh M, Kita J. Effect of billroth II or Roux-en-Y reconstruction for the gastrojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled study. Ann Surg 2013;257:938-942.
72 Sugiyama M, Abe N, Ueki H, Masaki T, Mori T, Atomi Y. A new reconstruction method for preventing delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. Am J Surg 2004;187:743-746.
73 Tani M, Terasawa H, Kawai M, Ina S, Hirono S, Uchiyama K, et al. Improvement of delayed gastric emptying in pyloruspreserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg 2006;243:316-320.
74 Akizuki E, Kimura Y, Nobuoka T, Imamura M, Nagayama M, Sonoda T, et al. Reconsideration of postoperative oral intake tolerance after pancreaticoduodenectomy: prospective consecutive analysis of delayed gastric emptying according to the ISGPS def i nition and the amount of dietary intake. Ann Surg 2009;249:986-994.
75 Chijiiwa K, Imamura N, Ohuchida J, Hiyoshi M, Nagano M, Otani K, et al. Prospective randomized controlled study of gastric emptying assessed by (13)C-acetate breath test after pylorus-preserving pancreaticoduodenectomy: comparison between antecolic and vertical retrocolic duodenojejunostomy. J Hepatobiliary Pancreat Surg 2009;16:49-55.
76 Gangavatiker R, Pal S, Javed A, Dash NR, Sahni P, Chattopadhyay TK. Effect of antecolic or retrocolic reconstruction of the gastro/duodenojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled trial. J Gastrointest Surg 2011;15:843-852.
77 Kurahara H, Shinchi H, Maemura K, Mataki Y, Iino S, Sakoda M, et al. Delayed gastric emptying after pancreatoduodenectomy. J Surg Res 2011;171:e187-192.
78 Eshuis WJ, van Dalen JW, Busch OR, van Gulik TM, Gouma DJ. Route of gastroenteric reconstruction in pancreatoduodenectomy and delayed gastric emptying. HPB (Oxford) 2012;14:54-59.
79 Eshuis WJ, van Eijck CH, Gerhards MF, Coene PP, de Hingh IH, Karsten TM, et al. Antecolic versus retrocolic route of the gastroenteric anastomosis after pancreatoduodenectomy: a randomized controlled trial. Ann Surg 2014;259:45-51.
80 Imamura N, Chijiiwa K, Ohuchida J, Hiyoshi M, Nagano M, Otani K, et al. Prospective randomized clinical trial of a change in gastric emptying and nutritional status after a pyloruspreserving pancreaticoduodenectomy: comparison between an antecolic and a vertical retrocolic duodenojejunostomy. HPB (Oxford) 2014;16:384-394.
81 Tamandl D, Sahora K, Prucker J, Schmid R, Holst JJ, Miholic J, et al. Impact of the reconstruction method on delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy:a prospective randomized study. World J Surg 2014;38:465-475.
82 Cordesmeyer S, Lodde S, Zeden K, Kabar I, Hoffmann MW. Prevention of delayed gastric emptying after pylorus-preserving pancreatoduodenectomy with antecolic reconstruction, a long jejunal loop, and a jejuno-jejunostomy. J Gastrointest Surg 2014;18:662-673.
83 Su AP, Cao SS, Zhang Y, Zhang ZD, Hu WM, Tian BL. Does antecolic reconstruction for duodenojejunostomy improve delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? A systematic review and meta-analysis. World J Gastroenterol 2012;18:6315-6323.
84 Zhou Y, Lin J, Wu L, Li B, Li H. Effect of antecolic or retrocolic reconstruction of the gastro/duodenojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a metaanalysis. BMC Gastroenterol 2015;15:68.
85 Hochwald SN, Grobmyer SR, Hemming AW, Curran E, Bloom DA, Delano M, et al. Braun enteroenterostomy is associated with reduced delayed gastric emptying and early resumption of oral feeding following pancreaticoduodenectomy. J Surg Oncol 2010;101:351-355.
86 Nikfarjam M, Houli N, Tufail F, Weinberg L, Muralidharan V, Christophi C. Reduction in delayed gastric emptying following non-pylorus preserving pancreaticoduodenectomy by addition of a Braun enteroenterostomy. JOP 2012;13:488-496.
87 Zhang XF, Yin GZ, Liu QG, Liu XM, Wang B, Yu L, et al. Does Braun enteroenterostomy reduce delayed gastric emptying after pancreaticoduodenectomy? Medicine (Baltimore) 2014;93:e48.
88 Xu B, Meng H, Qian M, Gu H, Zhou B, Song Z. Braun enteroenterostomy during pancreaticoduodenectomy decreases postoperative delayed gastric emptying. Am J Surg 2015;209:1036-1042.
89 Watanabe Y, Ohtsuka T, Kimura H, Matsunaga T, Tamura K, Ideno N, et al. Braun enteroenterostomy reduces delayed gastric emptying after pylorus-preserving pancreatoduodenectomy: a retrospective review. Am J Surg 2015;209:369-377.
90 Xu B, Zhu YH, Qian MP, Shen RR, Zheng WY, Zhang YW. Braun enteroenterostomy following pancreaticoduodenectomy:a systematic review and meta-analysis. Medicine (Baltimore) 2015;94:e1254.
91 Sakamoto Y, Kajiwara T, Esaki M, Shimada K, Nara S, Kosuge T. Roux-en-Y reconstruction using staplers during pancreaticoduodenectomy: results of a prospective preliminary study. Surg Today 2009;39:32-37.
92 Sakamoto Y, Yamamoto Y, Hata S, Nara S, Esaki M, Sano T, et al. Analysis of risk factors for delayed gastric emptying (DGE) after 387 pancreaticoduodenectomies with usage of 70 stapled reconstructions. J Gastrointest Surg 2011;15:1789-1797.
93 Sato N, Yabuki K, Kohi S, Mori Y, Minagawa N, Tamura T, et al. Stapled gastro/duodenojejunostomy shortens reconstruction time during pylorus-preserving pancreaticoduodenectomy. World J Gastroenterol 2013;19:9399-9404.
94 Shah OJ, Bangri SA, Singh M, Lattoo RA, Bhat MY. Omental fl aps reduces complications after pancreaticoduodenectomy. Hepatobiliary Pancreat Dis Int 2015;14:313-319.
95 Kurosaki I, Hatakeyama K. Preservation of the left gastric vein in delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy. J Gastrointest Surg 2005;9:846-852.
96 Gauvin JM, Sarmiento JM, Sarr MG. Pylorus-preserving pancreaticoduodenectomy with complete preservation of the pyloroduodenal blood supply and innervation. Arch Surg 2003;138:1261-1263.
July 6, 2016
Accepted after revision February 3, 2017
Author Aff i liations: Department of Gastrointestinal Surgery & Liver Transplantation, All India Institute of Medical Sciences, New Delhi, India (Panwar R and Pal S)
Dr. Rajesh Panwar, Department of Gastrointestinal Surgery & Liver Transplantation, Academic Block, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029, India (Tel:+911126593461; Fax: +911126588663; Email: rajeshpanwar81@gmail.com) © 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(17)60037-7
Published online July 1, 2017.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Predictive value of C-reactive protein/albumin ratio in acute pancreatitis
- IgG4-related sclerosing cholangitis and chronic sclerosing sialadenitis mimicking cholangiocarcinoma and neck malignancy
- Hepatopancreatoduodenectomy for advanced hepatobiliary malignancies: a single-center experience
- Interaction between insulin-like growth factor binding protein-related protein 1 and transforming growth factor beta 1 in primary hepatic stellate cells
- Bilioenteric anastomotic stricture in patients with benign and malignant tumors: prevalence, risk factors and treatment
- Effects of multimodal fast-track surgery on liver transplantation outcomes
