Effects of multimodal fast-track surgery on liver transplantation outcomes
2017-08-16JianHuaRaoFengZhangHaoLuXinZhengDaiChuanYongZhangXiaoFengQianXueHaoWangandLingLu
Jian-Hua Rao, Feng Zhang, Hao Lu, Xin-Zheng Dai, Chuan-Yong Zhang, Xiao-Feng Qian, Xue-Hao Wang and Ling Lu
Nanjing, China
Effects of multimodal fast-track surgery on liver transplantation outcomes
Jian-Hua Rao, Feng Zhang, Hao Lu, Xin-Zheng Dai, Chuan-Yong Zhang, Xiao-Feng Qian, Xue-Hao Wang and Ling Lu
Nanjing, China
BACKGROUND:Fast-track surgery and enhanced recovery after surgery have been applied to many surgical procedures; however, data on fast-track surgery and enhanced recovery after surgery following liver transplantation is limited. This study aimed to conduct a prospective study to determine the effects of fast-track surgery on prognosis after liver transplantation.
METHODS:This was a prospective, single-blinded, randomized study. One hundred twenty-eight patients undergoing liver transplantation were selected for the fast-track (FT group,n=54) or conventional process (NFT group,n=74). The primary endpoints were intensive care unit (ICU) stay and hospital stay. The secondary endpoints were as follows: operative time, anhepatic phase time, intraoperative blood loss, intraoperative blood transfusion volume, postoperative complications, readmission rate, and postoperative mortality.
RESULTS:There was no signif i cant difference in preoperative demographics between the two groups. The median ICU stay was 2 days (range 1-7 days) in the FT group and 5 days (range 3-12 days) in the NFT group (P<0.01). Furthermore, the hospital stay was also signif i cantly reduced in the FT group (P<0.01). The operative time, anhepatic phase time, intraoperative blood loss, and intraoperative blood transfusion volume were decreased in the FT group compared with the NFT group (P<0.05). Based on Spearman correlation analysis, the ICU stay and hospital stay may be positively correlated with operative time, anhepatic phase time and intraoperative blood loss. There were no differences in the incidence of postoperative complications, readmissions, and postoperative mortality between the two groups.
CONCLUSION:Fast-track procedures effectively reduce the ICU stay and hospital stay without adversely affecting prognosis. This study demonstrated that fast-track protocols are safe and feasible in liver transplantation.
(Hepatobiliary Pancreat Dis Int 2017;16:364-369)
fast-track surgery; liver transplantation; surgical drainage; ICU days; hospital stay
Introduction
The fi rst human orthotopic liver transplantation was performed by Starzl in the 1960s.[1]According to the U.S. Department of Health and Human Services Organ Procurement and Transplantation Network, >5000 orthotopic liver transplantations have been performed per year since 2000,[2]and data from the China Liver Transplantation Registry suggest that more than 20000 liver transplantations have been performed in China to date. It is clear that liver transplantation, as the only curative therapeutic method for patients with end-stage liver disease, brings the hope of survival for a large number of patients. Due to the complexity of liver transplantation, the associated trauma and the inf l uence of the primary disease, patients often need to stay in the intensive care unit (ICU) and hospital for long-term treatment postoperatively.
Fast-track surgery was proposed in the 1990s, and has been applied to cardiothoracic surgery,[3,4]gynecologic surgery[5-7]and gastrointestinal surgery, especially colorectal surgery.[8]Fast-track surgery has many advantages: improving the quality of care, shortening theICU stay and hospital stay for patients, and decreasing total treatment costs.[9]Fast-track surgery was theoretically def i ned as a procedure that accelerates the recovery progress from preoperative preparation of the patient throughout surgery and early discharge from hospital. In general, a fast-track program includes comprehensive preoperative education, no bowel preparation, no nasogastric tube placement, restriction of drainage after surgery, prevention of intraoperative hypothermia, minimally invasive incisions, early ambulation postoperatively, and nutrition enhancement.[9-12]
To date, fast-track surgery has been widely accepted amongst the different surgical disciplines, including liver transplantation. Preliminary attempts have been made in some centers;[13-15]however, the relevance of fast-track surgery with respect to liver transplantation is still unclear because of study limitations, such as sample size and research direction. Herein, we designed a prospective study to explore the impact of fast-track surgery on the prognosis of liver transplantation.
Methods
Patients
This study was approved by the Ethics Committee of First Aff i liated Hospital of Nanjing Medical University. We enrolled patients who were scheduled for liver transplantation in our center between January 2012 and December 2013. The inclusion criteria were as follows:i) the cause of end-stage liver disease was liver cirrhosis or primary hepatocellular carcinoma based on the Milan criteria;[16]ii) a modif i ed piggyback liver transplantation; and iii) the fi rst liver transplantation. The exclusion criteria were as follows: i) age ≤16 years and ≥70 years; ii) more than one liver transplantation; and iii) hepatic artery intubation chemotherapy embolism or radiofrequency ablation treatment pre- or postoperatively. One hundred twenty-eight patients of liver transplantation met the study criteria. These patients were single-blind randomized divided into fast-track (FT;n=54) and nonfast-track (NFT,n=74) groups. Of the 128 patients, 70 had hepatitis-related cirrhosis, 16 had alcoholic liver cirrhosis, and 42 had primary hepatocellular carcinoma. This study was a randomized single-blind study.
Peri-operative management
Preoperative treatment measures were the same in both groups, including comprehensive preoperative communication about the overall surgical procedure and postoperative care, elimination of preoperative bowel preparation and prophylactic antibiotic administration, preoperative solid food fasting for 6 hours, preoperative liquid fasting for 2 hours, intravenous administration of glucose, and non-use of a nasogastric tube. In the FT group, all patients had a shortened anesthesia time, controlled hypotension (central venous pressure <5 mmHg), improved heat preservation measures, and avoidance of excessive infusions intraoperatively. The portal vein clamping time in the FT group was shortened as much as possible intraoperatively and surgical drainage tubes were not used postoperatively. In contrast, the NFT group received conventional intraoperative anesthetic and surgical treatments. The operative method was a modif i ed piggyback liver transplantation. In the FT group, the endotracheal intubation was removed in the ICU during the early phase, and the patients were transferred to the general ward for further treatment. Early exercise and enteral nutrition were also encouraged. The intravenous infusion was restricted and the urine catheter was removed early. The patients in the NFT group were treated according to a traditional approach. The details of the peri-operative treatments are shown in Table 1.
Outcome measures
The primary outcome measures included ICU stay and hospital stay. The secondary outcome measures included operative time, anhepatic phase time, intraoperative blood loss, intraoperative blood transfusion volume, postoperative mortality, readmission rate, and postoperative complications (incision infections, abdominal hemorrhage, ascites, pneumonia and delayed incision healing). The discharge criteria were stable vital signs, healing incision, tolerating a regular diet, no sleep disturbances, no abdominal distension, and no pain. All patients were followed for 3 months.
Statistical analysis
SPSS 12.0 software (SPSS, Inc., Chicago, IL, USA) was used for statistical analyses. Normally-distributed data are shown as the mean±standard deviation (SD). Skewed distribution data are shown as median and 1st-3rd quartile. A Chi-square test was used to compare rates. Student’sttest and the Mann-WhitneyUtest were used to compare the mean and median, respectively. Spearman’s rank correlation analysis was used to evaluate the relationship between treatment measures and clinical parameters. Stepwise logistic regression was used to assess the association between variable and clinical parameters (all continuous dependent variables were transformed into categorical variables). AP<0.05 (two-sided) was considered statistically signif i cant.
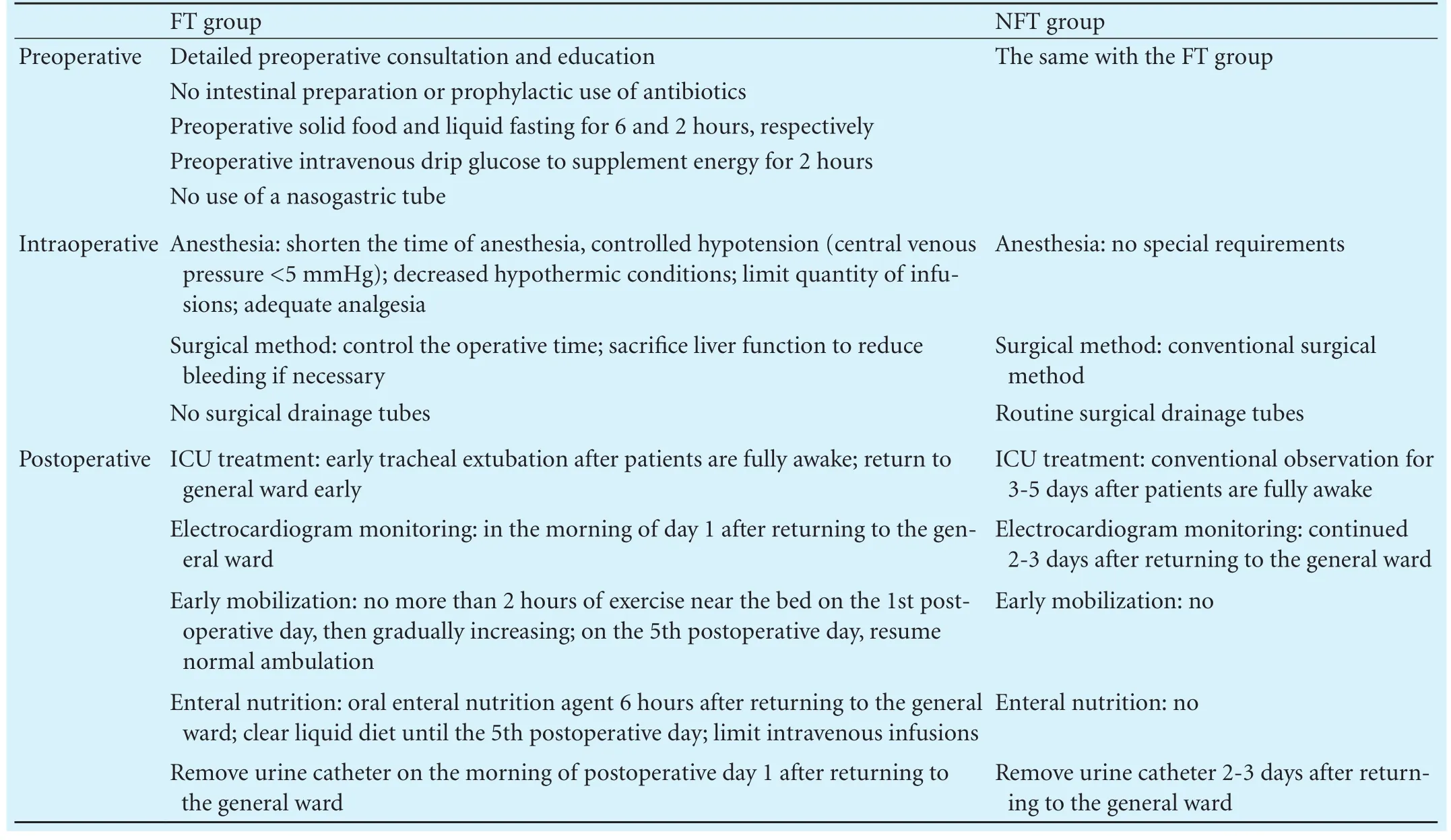
Table 1. Peri-operative management of the two groups
Results
General information
There were no signif i cant differences between the two groups, including gender, age, ASA grade, primary cause for end-stage liver disease, and MELD score (P>0.05); however, signif i cant differences were demonstrated intraoperatively (Table 2). Compared with the NFT group, the operative time (265 vs 325 minutes,P=0.018) and anhepatic phase time (45 vs 60 minutes,P=0.006) were shortened signif i cantly in the FT group. The intraoperative blood loss (1100 vs 2900 mL,P=0.025) and blood transfusion volume >1000 mL (59.3% vs 86.5%,P=0.035) in the FT group were signif i cantly less than those in the NFT group. In addition, patients in the FT group recovered better; specif i cally, the postoperative ICU stay and hospital stay were decreased. There was no signif i cant difference in the postoperative complication rate between the two groups. No readmissions and postoperative mortality occurred during the follow-up period.
Spearman correlation of treatment and prognostic indicators
As shown in Table 3, the operative time was positively correlated with the following four indicators: anhepatic phase time, intraoperative blood loss, ICU stay, and hospital stay. A correlation between operative time and intraoperative blood loss was suggested. Moreover, the ICU stay and hospital stay were positively correlated with intraoperative blood loss; however, there was no correlation between the incidence of postoperative complications and clinical parameters.
Recovery
Postoperative management in the FT group, which reduced the ICU stay and hospital stay, was benef i t factors (Table 4); however, there were no apparent targets serving as predictive factors for postoperative complications.
Discussion
The fast-track program, which can be viewed as an enhanced recovery program, includes detailed pre-surgery counseling education, improvements in surgical and anesthetic methods, early ambulation, strengthened enteral nutrition, and other measures during the peri-operative period. The fast-track program has been conf i rmed to shorten hospital stay and reduce costs for patients, but does not increase the rate of postoperative readmissions or the postoperative recurrence and mortality rates.[17,18]Recently, fast-track management has also been used in pancreatic surgery, which demonstrates that the fasttrack program is safe and has the potential to reduce the waiting time for surgery, the overall number of biliary drainage procedures, and the associated complications.[19-21]In liver surgery, especially liver transplantation,relevant research is limited. Therefore, in the current study, the role of the fast-track program in liver transplantation was studied.

Table 2. Characteristics of enrolled patients
Liver transplantation, as the only curative treatment for end-stage liver disease, has been widely accepted; however, liver transplantation often causes serious intraoperative bleeding owing to the complexity and diff i culty of the procedure. Excessive bleeding leads to excessive transfusion. As reported, the probability of acute respiratory distress syndrome/acute lung injury are positively related to the total volume of transfusion, as well as mortality and multiple organ failure.[22]Transfusionrelated acute lung injury is the most frequent and severe complication in patients receiving excessive transfusions.[23]This leads to prolonged ICU stay and hospital stay, increases the economic burden, and decreases the utilization rate of hospital beds. In fact, the continuation of hemodynamic, respiratory, and metabolic support for a variable period after liver transplantation in the ICU is considered routine by many transplant programs.[24]To avoid this troublesome complication, controlled hypotension is used in our fast-track program. In addition, improvements in surgical and anesthetic techniquesin recent decades have reduced the patient acuity after transplant surgery. In addition, patients require less invasive monitoring and intensive care. Our results showed that the anhepatic phase time had been signif i cantly shortened in most patients in the FT group compared to the NFT group, but in some complicated cases, vascular anastomoses led to a prolonged anhepatic phase time, which caused aggravated ischemia-reperfusion injuries of the intestinal and liver grafts. Furthermore, the operative time was signif i cantly reduced in the FT group compared with the NFT group based on a shorter anhepatic phase time and less intraoperative blood loss. These factors favored shortened ICU stay and hospital stay. Spearman correlation analysis showed that the operative time, anhepatic phase time, and blood loss were indicators of shortening ICU stay and hospital stay. Thus, there was a decline in therapeutic costs and increased utilization rate of hospital beds as a result of fast-track management.

Table 3. Spearman correlation analysis of therapeutic measures and recovery index
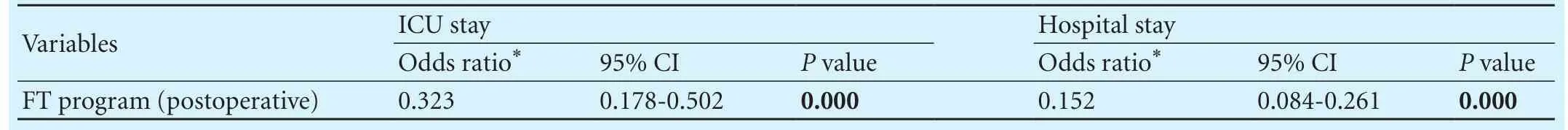
Table 4. Logistic stepwise regression analysis of recovery index
Postoperative management is an important part of the fast-track program. As reported, continuous positivepressure ventilation might result in an elevated incidence of pleural effusion and ascites;[25,26]however, we showed no signif i cant difference in the incidence of postoperative complications between the two groups. Prolonged ICU stay might lead to pulmonary infections and emboli. Early ambulation promotes the functional recovery of the kinetic and respiratory systems, reduces pleural exudate formation, and prevents pulmonary infections, bedsores, and emboli. In addition, early enteral nutrition improves the recovery of gastrointestinal function, alleviates postoperative nausea and vomiting, and avoids intestinal paralysis. In the current study, the patients in the FT group were encouraged to ambulate near the bed the fi rst day after liver transplantation. Intravenous fl uids were gradually reduced with a corresponding increased liquid diet. Other measures, such as non-use of surgical drainage tubes and early removal of urethral catheters, also favored early ambulation. Indeed, placement of surgical drainage tubes and urethral catheters might cause retrograde infections. Finally, logistic stepwise regression analysis of the recovery index showed that fast-track programs signif i cantly reduced ICU stay and hospital stay, which helped to increase the utilization rate of hospital beds. There are other potential elements, including patient education, intraoperative body temperature, and postoperative analgesia that can play a role in the peri-operative management and outcomes of recipients, which will be analyzed in future detailed analyses.
In the current study, both groups of patients received the same preoperative treatment program. This study demonstrates that fast-track surgery in patients undergoing liver transplantation can shorten the operative time and anhepatic phase, reduce the intraoperative blood loss, and reduce the ICU stay and hospital stay, but does not increase the incidence of postoperative complications. Fast-track surgery in patients undergoing liver transplantation is safe and feasible, which is still demonstrated in more patients.
Contributors: RJH and ZF contributed equally to this article. RJH, ZF and LL proposed the study. RJH and ZF wrote the fi rst draft. LH and DXZ collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. LL is the guarantor.
Funding: This study was supported by grants from the Foundation of Jiangsu Collaborative Innovation Center of Biomedical Functional Materials, Basic Research Program-Youth Fund Project of Jiangsu Province (BK20140092), and the National Natural Science Foundation of China (81400650, 81470901, 81273261 and 81270583).
Ethical approval: The study was approved by the Ethics Committee of First Aff i liated Hospital of Nanjing Medical University.
Competing interest: No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Starzl TE, Marchioro TL, Vonkaulla KN, Hermann G, Brittain RS, Waddell WR. Homotransplantation of the liver in humans. Surg Gynecol Obstet 1963;117:659-676.
2 Pai SL, Aniskevich S, Rodrigues ES, Shine TS. Analgesic considerations for liver transplantation patients. Curr Clin Pharmacol 2015;10:54-65.
3 Podore PC, Throop EB. Infrarenal aortic surgery with a 3-day hospital stay: A report on success with a clinical pathway. J Vasc Surg 1999;29:787-792.
4 Tovar EA, Roethe RA, Weissig MD, Lloyd RE, Patel GR. Oneday admission for lung lobectomy: an incidental result of a clinical pathway. Ann Thorac Surg 1998;65:803-806.
5 Marx C, Rasmussen T, Jakobsen DH, Ottosen C, Lundvall L, Ottesen B, et al. The effect of accelerated rehabilitation on recovery after surgery for ovarian malignancy. Acta Obstet Gynecol Scand 2006;85:488-492.
6 Møller C, Kehlet H, Friland SG, Schouenborg LO, Lund C, Ottesen B. Fast track hysterectomy. Eur J Obstet Gynecol Reprod Biol 2001;98:18-22.
7 Ottesen M, Sørensen M, Rasmussen Y, Smidt-Jensen S, Kehlet H, Ottesen B. Fast track vaginal surgery. Acta Obstet Gynecol Scand 2002;81:138-146.
8 Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-617.
9 Stoot JH, van Dam RM, Busch OR, van Hillegersberg R, De Boer M, Olde Damink SW, et al. The effect of a multimodal fast-track programme on outcomes in laparoscopic liver surgery: a multicentre pilot study. HPB (Oxford) 2009;11:140-144.
10 Kennedy EP, Grenda TR, Sauter PK, Rosato EL, Chojnacki KA, Rosato FE Jr, et al. Implementation of a critical pathway for distal pancreatectomy at an academic institution. J Gastroin-test Surg 2009;13:938-944.
11 Lin DX, Li X, Ye QW, Lin F, Li LL, Zhang QY. Implementation of a fast-track clinical pathway decreases postoperative length of stay and hospital charges for liver resection. Cell Biochem Biophys 2011;61:413-419.
12 van Dam RM, Hendry PO, Coolsen MM, Bemelmans MH, Lassen K, Revhaug A, et al. Initial experience with a multimodal enhanced recovery programme in patients undergoing liver resection. Br J Surg 2008;95:969-975.
13 Glanemann M, Busch T, Neuhaus P, Kaisers U. Fast tracking in liver transplantation. Immediate postoperative tracheal extubation: feasibility and clinical impact. Swiss Med Wkly 2007;137:187-191.
14 Konstantinov IE, McNeil K, Yeung S, Fawcett J, Mullany D, Dunning J. Fast track recovery following en bloc heartlung-liver transplantation in a patient with cystic fi brosis complicated by severe portal hypertension. Heart Lung Circ 2008;17:154-156.
15 Ng KK, Lo CM, Chan SC, Chok KS, Cheung TT, Fan ST. Liver transplantation for hepatocellular carcinoma: the Hong Kong experience. J Hepatobiliary Pancreat Sci 2010;17:548-554.
16 Ahn CS, Moon DB, Lee SG, Hwang S, Kim KH, Ha TY, et al. Survival differences between Milan criteria after downstaging and De novo Milan in living donor liver transplantation for hepatocellular carcinoma. Hepatogastroenterology 2014;61:187-191.
17 King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH, et al. Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 2006;93:300-308.
18 Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 2011;254:868-875.
19 Zouros E, Liakakos T, Machairas A, Patapis P, Agalianos C, Dervenis C. Improvement of gastric emptying by enhanced recovery after pancreaticoduodenectomy. Hepatobiliary Pancreat Dis Int 2016;15:198-208.
20 French JJ, Mansf i eld SD, Jaques K, Jaques BC, Manas DM, Charnley RM. Fast-track management of patients undergoing proximal pancreatic resection. Ann R Coll Surg Engl 2009;91:201-204.
21 Wichmann MW, Roth M, Jauch KW, Bruns CJ. A prospective clinical feasibility study for multimodal “fast track” rehabilitation in elective pancreatic cancer surgery. Rozhl Chir 2006;85:169-175.
22 Patel SV, Kidane B, Klingel M, Parry N. Risks associated with red blood cell transfusion in the trauma population, a metaanalysis. Injury 2014;45:1522-1533.
23 Lee YL, King MB, Gonzalez RP, Brevard SB, Frotan MA, Gillespie MN, et al. Blood transfusion products contain mitochondrial DNA damage-associated molecular patterns: a potential effector of transfusion-related acute lung injury. J Surg Res 2014;191:286-289.
24 Taner CB, Willingham DL, Bulatao IG, Shine TS, Peiris P, Torp KD, et al. Is a mandatory intensive care unit stay needed after liver transplantation? Feasibility of fast-tracking to the surgical ward after liver transplantation. Liver Transpl 2012;18:361-369.
25 Jullien T, Valtier B, Hongnat JM, Dubourg O, Bourdarias JP, Jardin F. Incidence of tricuspid regurgitation and vena caval backward fl ow in mechanically ventilated patients. A color Doppler and contrast echocardiographic study. Chest 1995;107:488-493.
26 Kaisers U, Langrehr JM, Haack M, Mohnhaupt A, Neuhaus P, Rossaint R. Hepatic venous catheterization in patients undergoing positive end-expiratory pressure ventilation after OLT:technique and clinical impact. Clin Transplant 1995;9:301-306.
December 15, 2015
Accepted after revision November 30, 2016
Author Aff i liations: Liver Transplantation Center, First Aff i liated Hospital of Nanjing Medical University; Key Laboratory of Living Donor Liver Transplantation of Ministry of Public Health, Nanjing 210029, China (Rao JH, Zhang F, Lu H, Dai XZ, Zhang CY, Qian XF, Wang XH and Lu L)
Ling Lu, MD, PhD, Liver Transplantation Center, First Aff i liated Hospital of Nanjing Medical University; Key Laboratory of Living Donor Liver Transplantation of Ministry of Public Health, #300 Guangzhou Road, Nanjing 210029, China (Tel: +86-25-83718836ext6476; Fax: +86-25-83672106; Email: lvling@njmu.edu.cn)
© 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(17)60020-1
Published online May 18, 2017.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Indocyanine green fl uoroscopy and liver transplantation: a new technique for the intraoperative assessment of bile duct vascularization
- Characteristics of recipients with complete immunosuppressant withdrawal after adult liver transplantation
- Predictive value of C-reactive protein/albumin ratio in acute pancreatitis
- Bilioenteric anastomotic stricture in patients with benign and malignant tumors: prevalence, risk factors and treatment
- Interaction between insulin-like growth factor binding protein-related protein 1 and transforming growth factor beta 1 in primary hepatic stellate cells
- Hepatopancreatoduodenectomy for advanced hepatobiliary malignancies: a single-center experience
