Hepatopancreatoduodenectomy for advanced hepatobiliary malignancies: a single-center experience
2017-08-16WingChiuDaiKennethSHChokTanToCheungAlbertCYChanSeeChingChanandChungMauLo
Wing Chiu Dai, Kenneth SH Chok, Tan To Cheung, Albert CY Chan, See Ching Chan and Chung Mau Lo
Hong Kong, China
Hepatopancreatoduodenectomy for advanced hepatobiliary malignancies: a single-center experience
Wing Chiu Dai, Kenneth SH Chok, Tan To Cheung, Albert CY Chan, See Ching Chan and Chung Mau Lo
Hong Kong, China
BACKGROUND:Hepatopancreatoduodenectomy is a complicated and challenging procedure but necessary for curative resection for advanced hepatobiliary malignancies. This retrospective study was to examine the safety and survival outcomes of hepatopancreatoduodenectomy in our center.
METHODS:Prospectively collected data of 12 patients who underwent hepatopancreatoduodenectomy for advanced hepatobiliary malignancies in our hospital from January 1998 to December 2014 were analyzed. The primary endpoints are treatment-related morbidity and mortality and the secondary endpoints are overall survival and disease-free survival.
RESULTS:Curative resection was achieved in 11 (91.7%) patients. Complications developed in 10 (83.3%) patients. Three hospital deaths resulted from multiorgan failure secondary to postoperative pancreatic fi stula or hepaticojejunostomy leakage. Six of the nine remaining patients had disease recurrence. The nine patients had a median survival of 39.8 (5.3-151.8) months. The 1-, 3- and 5-year overall survival rates were 66.7%, 55.6% and 27.8%, respectively. The corresponding disease-free survival rates were 55.6%, 44.4% and 29.6%, respectively.
CONCLUSIONS:Morbidity and mortality after hepatopancreatoduodenectomy were signif i cant. With R0 resection, the 5-year overall survival and disease-free survival rates were 27.8% and 29.6%, respectively.
(Hepatobiliary Pancreat Dis Int 2017;16:382-386)
hepatectomy; hepatopancreatoduodenectomy; malignancy; pancreaticojejunostomy; pancreatoduodenectomy
Introduction
Hepatopancreatoduodenectomy (HPD) is the combination of major hepatectomy and pancreatoduodenectomy (PD). The use of this procedure was fi rst reported by Takasaki et al[1]in 1980. With the improvements of surgical techniques and intensive care, many centers can perform pancreatic resection or partial hepatic resection with a mortality rate of <5%.[2-4]However, HPD is not a widely applied procedure because of its high mortality rate (14%-50%)[5-10]resulting mainly from pancreatic fi stula or liver failure related to resected liver volume and operative blood loss. Indications for HPD and the role of this operation have not been adequately analyzed. This study is to review our experience with this complicated procedure.
Methods
We analyzed the prospectively collected data of the 12 patients who underwent HPD for advanced hepatobiliary malignancies at our center from January 1998 to December 2014. The primary endpoints of the study are treatment-related morbidity and mortality and the secondary endpoints are overall survival and disease-free survival.
The indications for HPD were mainly cholangiocarcinoma and carcinoma of the gallbladder. In certain cases of extensive liver tumor involving the duodenum or pancreas, the decision to proceed to HPD was at thediscretion of the chief operating surgeon (who must be an experienced hepatobiliary surgeon) during operation.
Our criteria for patient selection for major hepatectomy have been described elsewhere.[11,12]In general, we assessed the patients’ general condition, tumor status and liver function and estimated the volume of their future liver remnant. For patients with jaundice, preoperative endoscopic or percutaneous biliary drainage was performed to reduce the serum total bilirubin level to below three times the upper limit of normal value. For patients with an estimated liver remnant volume of less than 30% of standard volume, portal vein embolization of the liver lobe harboring the tumor was performed to induce hypertrophy of the contralateral lobe.[1]Liver function assessment was based largely on indocyanine green clearance test. An indocyanine green retention rate of 14% at 15 minutes after intravenous injection was deemed acceptable for major hepatectomy.
Our surgical techniques of hepatectomy and PD have been described in our earlier studies.[11,13]Usually hepatectomy was performed before PD. In cases where PD was the initial plan but liver involvement was discovered during operation, hepatectomy followed. Liver transection was mainly done with an ultrasonic dissector. The chief surgeon decided on conventional or pylorus-preserving PD to perform. An end-to-side, duct-to-mucosa, two-layer pancreaticojejunostomy (PJ) was constructed using interrupted fi ne Prolene sutures. Pancreatic stenting was employed if the pancreatic duct was small. Two drains were placed routinely, one anterior and the other posterior to the PJ.
Postoperative pancreatic fi stula was def i ned as an amylase concentration in the drain fl uid (obtained on or after postoperative day 3) greater than three times the standard serum amylase concentration.[14]Data were expressed as median and range for continuous variables and as proportions for categorical variables. Overall survival and disease-free survival were estimated by the Kaplan-Meier method. Statistical comparison of survival distribution was analyzed by the log-rank test.Pvalues<0.05 were considered statistically signif i cant. Statistical analyses were performed with PASW Statistics 18.
Results
There are 12 patients in the cohort. Their demographic and perioperative data can be found in Table 1. Three patients had preoperative right portal vein embolization due to inadequate future liver remnant. All patients underwent PD with PJ done with the duct-to-mucosa technique. Concurrent hepatectomy was also conducted:seven patients had right hepatectomy, three had resec-tion of segments 4 and 5, and two had right trisectionectomy. Four patients received portal vein resection and primary anastomosis due to suspected tumor invasion of the portal vein. Two patients had tumor invasion of the colon and thus received partial colectomy (Table 2).

Table 1. Clinical data of the cohort (n=12)
Three (25.0%) patients died of multiorgan failure secondary to leakage from hepaticojejunostomy or pancreatic fi stula (Table 2). Ten (83.3%) out of 12 patients had complications (Table 3). The most common complication was wound infection, followed by postoperative pancreatic fi stula (n=4), three underwent relaparotomy and one was managed conservatively.
Curative resection was achieved in 11 of the 12 patients. Six out of the nine survivors had tumor recurrence (Table 2). The nine patients had a median survival of 39.8 (range 5.3-151.8) months. Fig. 1 is a Kaplan-Meier plot for overall survival. The 1-, 3- and 5-year overall survival rates were 66.7%, 55.6% and 27.8%, respectively. Fig. 2 is a Kaplan-Meier plot for disease-free survival. The 1-, 3- and 5-year disease-free survival rates were 55.6%, 44.4% and 29.6% (at fi ve years, two patients survived and both were disease-free, but the overall survival rate was lower than the disease-free survival rate in statistical calculation), respectively.
Discussion
HPD has high morbidity and mortality rates. At our center, a tertiary referral center in Hong Kong with extensive experience in hepatobiliary surgery, the mortality rates for major hepatectomy or PD are <5%.[2,15]However, in the present study where the two procedures were combined, the mortality rate was 25.0% and the morbidity rate was 83.3%.

Table 2. Clinical details of each of the 12 patients

Table 3. Complications in the 10 patients
HPD was fi rst introduced in 1980. In the early 1990s, it carried a morbidity rate of 90%-100% and a mortality rate of 25%-29%.[16,17]Later, major HPD was reported to carry a mortality rate of 14%-50%,[7,18-22]but at the same time low or even zero mortality was also reported.[5,23-25]In a recent systematic review of 18 studies of HPD for biliary and gallbladder cancers, the morbidity and mortality rates in the 397 patients were 78.9% and 10.3%, respectively.[26]It is important to note the heterogeneity of operations and procedures in these studies; there weredistal pancreatectomy and minor hepatectomy, and some patients underwent complete external drainage of pancreatic juice before PJ. It is therefore not surprising that the results found were quite different from the results of our present study.

Fig. 1. Overall survival of the nine patients who survived HPD.
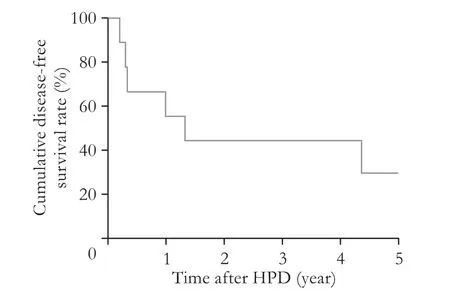
Fig. 2. Disease-free survival of the nine patients who survived HPD.
HPD is so complicated and challenging that under no circumstances should it be performed by surgeons without ample experience and a high level of skills, and PJ is the Achilles’ heel of HPD. Most post-HPD deaths were caused by pancreatic fi stula due to PJ leakage. In the present study, four patients developed postoperative pancreatic fi stula; three of them required relaparotomy and one was managed conservatively. Totally four patients in the study underwent relaparotomy due to pancreatic fi stula or hepaticojejunostomy leakage and three of them ended up in hospital death. Apart from pancreatic fi stula, wound infection (n=5), subphrenic abscess/collection (n=3) and pleural effusion (n=4) were also the common complications in this study. Liver failure is another common cause of post-HPD deaths. Some studies found that patients who died of liver failure following major hepatectomy had postoperative infectious complications which exacerbated liver dysfunction.[7,27,28]
Appropriate preoperative biliary drainage following portal vein embolization to optimize residual liver function has been shown to improve outcomes.[29-31]Regarding pancreatic fi stula, it has been suggested that external drainage of pancreatic juice followed by PJ as a secondstage operation would be helpful,[20,23]especially when concurrent vascular resection is required for curative tumor resection in patients with a thin pancreatic duct and soft pancreatic parenchyma. On the other hand, there is the suggestion that one-stage operation with reconstruction is to be performed as a fi nal step so that if the Pringle maneuver is required to control bleeding during hepatectomy, it would not affect the integrity of the various anastomoses due to venous congestion.
In the literature, the main indications for HPD are diffuse bile duct cancer and advanced gallbladder neoplasm, and there are also cases of major HPD for resection of the pancreas and liver metastases from different metachronous primary tumors.[32,33]In the present study, indications for HPD also varied, with carcinoma of the gallbladder (n=5) and cholangiocarcinoma (n=4) predominating.
Early reports did not endorse HPD for diffuse bile duct cancer due to the lack of long-term survivors.[16,17]In recent reports, 5-year survival came at a low of 16% to as high as 80% in patients without residual tumor and lymph node metastasis.[5,23,25,34]For carcinoma of the gallbladder, many centers advocated extended resection, including HPD for advanced stage-3 or stage-4 disease, for better tumor clearance,[19,20,35]and 5 year survival rates were 29%-42.9% after HPD.[18,23,36]
There might be inherent differences between gallbladder cancer and extrahepatic cholangiocarcinoma, but long-term survival of patients with either of the diseases has been consistently demonstrated to be independently associated with curative resection.[37-39]In the present cohort, although disease recurrence was common, there still were long-term survivors. We believe that lymph node metastasis is not a contraindication to HPD in patients with biliary carcinoma when a potentially curative resection (R0) is achievable.
This study cannot serve as an endorsement for the wide application of HPD since the cohort was small and the complication and mortality rates were high. However, as there is no alternative curative treatment for advanced hepatobiliary malignancies, HPD should be considered for carefully selected patients if the expertise is available and a curative resection (R0) is feasible.
Contributors: DWC designed the study, collected and analyzed data, and drafted and critically revised the manuscript. CKSH designed the study and collected data. CTT, CACY and CSC collected data. LCM collected data and supervised the study. All authors approved the submitted manuscript. DWC is the guarantor.
Funding: None.
Ethical approval: Not needed.
Competing interest: No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Takasaki K, Kobayashi S, Mutou H, Akimoto S, Toda K, Asado S. Our experiences (5 cases) of extended right lobectomy combined with pancreatoduodenectomy for the carcinoma of the gallbladder (in Japanese). Tan to Sui 1980;1:923-932.
2 Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, et al. Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg 1999;229:322-330.
3 Kimura W. Strategies for the treatment of invasive ductal carcinoma of the pancreas and how to achieve zero mortality for pancreaticoduodenectomy. J Hepatobiliary Pancreat Surg 2008;15:270-277.
4 Kamiyama T, Nakanishi K, Yokoo H, Kamachi H, Tahara M, Yamashita K, et al. Perioperative management of hepatic resection toward zero mortality and morbidity: analysis of 793 consecutive cases in a single institution. J Am Coll Surg 2010;211:443-449.
5 Yoshimi F, Asato Y, Amemiya R, Shioyama Y, Itabashi M. Comparison between pancreatoduodenectomy and hepatopancreatoduodenectomy for bile duct cancer. Hepatogastroenterology 2001;48:994-998.
6 Nakamura S, Suzuki S, Serizawa A, Sakaguchi T, Konno H, Baba S, et al. Hepatopancreatoduodenectomy for superf i cially spreading bile duct carcinoma: a report of two 5 year survivals. Hepatogastroenterology 1996;43:138-142.
7 D’Angelica M, Martin RC 2nd, Jarnagin WR, Fong Y, DeMat-teo RP, Blumgart LH. Major hepatectomy with simultaneous pancreatectomy for advanced hepatobiliary cancer. J Am Coll Surg 2004;198:570-576.
8 Araida T, Yoshikawa T, Azuma T, Ota T, Takasaki K, Hanyu F. Indications for pancreatoduodenectomy in patients undergoing lymphadenectomy for advanced gallbladder carcinoma. J Hepatobiliary Pancreat Surg 2004;11:45-49.
9 Hirono S, Tani M, Kawai M, Ina S, Uchiyama K, Yamaue H. Indication of hepatopancreatoduodenectomy for biliary tract cancer. World J Surg 2006;30:567-575.
10 Chijiiwa K, Nishiyama K, Takashima M, Mizumoto K, Noshiro H, Shimizu S, et al. Diffuse bile duct carcinoma treated by major hepatectomy and pancreatoduodenectomy with the aid of pre-operative portal vein embolization. Report of two cases. Hepatogastroenterology 1999;46:1634-1638.
11 Fan ST, Mau Lo C, Poon RT, Yeung C, Leung Liu C, Yuen WK, et al. Continuous improvement of survival outcomes of resection of hepatocellular carcinoma: a 20-year experience. Ann Surg 2011;253:745-758.
12 Poon RT, Fan ST. Hepatectomy for hepatocellular carcinoma:patient selection and postoperative outcome. Liver Transpl 2004;10:S39-45.
13 Cheung TT, Poon RT, Chok KS, Chan AC, Tsang SH, Dai WC, et al. Pancreaticoduodenectomy with vascular reconstruction for adenocarcinoma of the pancreas with borderline resectability. World J Gastroenterol 2014;20:17448-17455.
14 Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fi stula: an international study group (ISGPF) def i nition. Surgery 2005;138:8-13.
15 Poon RT, Fan ST, Lo CM, Ng KK, Yuen WK, Yeung C, et al. External drainage of pancreatic duct with a stent to reduce leakage rate of pancreaticojejunostomy after pancreaticoduodenectomy:a prospective randomized trial. Ann Surg 2007;246:425-435.
16 Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A, et al. Hepatopancreatoduodenectomy for advanced carcinoma of the biliary tract. Hepatogastroenterology 1991;38:170-175.
17 Tsukada K, Yoshida K, Aono T, Koyama S, Shirai Y, Uchida K, et al. Major hepatectomy and pancreatoduodenectomy for advanced carcinoma of the biliary tract. Br J Surg 1994;81:108-110.
18 Shirai Y, Ohtani T, Tsukada K, Hatakeyama K. Combined pancreaticoduodenectomy and hepatectomy for patients with locally advanced gallbladder carcinoma: long term results. Cancer 1997;80:1904-1909.
19 Kondo S, Nimura Y, Hayakawa N, Kamiya J, Nagino M, Uesaka K. Extensive surgery for carcinoma of the gallbladder. Br J Surg 2002;89:179-184.
20 Miyagawa S, Makuuchi M, Kawasaki S, Hayashi K, Harada H, Kitamura H, et al. Outcome of major hepatectomy with pancreatoduodenectomy for advanced biliary malignancies. World J Surg 1996;20:77-80.
21 Ishihara S, Miyakawa S, Takada T, Takasaki K, Nimura Y, Tanaka M, et al. Status of surgical treatment of biliary tract cancer. Dig Surg 2007;24:131-136.
22 Ebata T, Nagino M, Nishio H, Arai T, Nimura Y. Right hepatopancreatoduodenectomy: improvements over 23 years to attain acceptability. J Hepatobiliary Pancreat Surg 2007;14:131-135.
23 Miwa S, Kobayashi A, Akahane Y, Nakata T, Mihara M, Kusama K, et al. Is major hepatectomy with pancreatoduodenectomy justif i ed for advanced biliary malignancy? J Hepatobiliary Pancreat Surg 2007;14:136-141.
24 Addeo P, Oussoultzoglou E, Fuchshuber P, Rosso E, Nobili C, Langella S, et al. Safety and outcome of combined liver and pancreatic resections. Br J Surg 2014;101:693-700.
25 Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg 2012;256:297-305.
26 Zhou Y, Zhang Z, Wu L, Li B. A systematic review of safety and eff i cacy of hepatopancreatoduodenectomy for biliary and gallbladder cancers. HPB (Oxford) 2016;18:1-6.
27 Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 2002;236:397-407.
28 Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808-819.
29 Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg 2006;243:364-372.
30 Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg 2003;238:84-92.
31 Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, et al. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg 2003;238:73-83.
32 Sugiura T, Nagino M, Ebata T, Arai T, Oda K, Yuasa N, et al. Treatment of colorectal liver metastasis with biliary and portal vein tumor thrombi by hepatopancreatoduodenectomy. J Hepatobiliary Pancreat Surg 2006;13:256-259.
33 De Jong MC, Farnell MB, Sclabas G, Cunningham SC, Cameron JL, Geschwind JF, et al. Liver-directed therapy for hepatic metastases in patients undergoing pancreaticoduodenectomy:a dual-center analysis. Ann Surg 2010;252:142-148.
34 Urahashi T, Yamamoto M, Ohtsubo T, Katsuragawa H, Katagiri S, Takasaki K. Hepatopancreatoduodenectomy could be allowed for patients with advanced intrahepatic cholangiocarcinoma. Hepatogastroenterology 2007;54:346-349.
35 Todoroki T, Kawamoto T, Takahashi H, Takada Y, Koike N, Otsuka M, et al. Treatment of gallbladder cancer by radical resection. Br J Surg 1999;86:622-627.
36 Sasaki R, Takahashi M, Funato O, Nitta H, Murakami M, Kawamura H, et al. Hepatopancreatoduodenectomy with wide lymph node dissection for locally advanced carcinoma of the gallbladder--long-term results. Hepatogastroenterology 2002;49:912-915.
37 Murakami Y, Uemura K, Sudo T, Hayashidani Y, Hashimoto Y, Nakamura H, et al. Adjuvant gemcitabine plus S-1 chemotherapy improves survival after aggressive surgical resection for advanced biliary carcinoma. Ann Surg 2009;250:950-956.
38 Chan SY, Poon RT, Lo CM, Ng KK, Fan ST. Management of carcinoma of the gallbladder: a single-institution experience in 16 years. J Surg Oncol 2008;97:156-164.
39 Kaneoka Y, Yamaguchi A, Isogai M, Kumada T. Survival benef i t of hepatopancreatoduodenectomy for cholangiocarcinoma in comparison to hepatectomy or pancreatoduodenectomy. World J Surg 2010;34:2662-2670.
June 4, 2016
Accepted after revision December 16, 2016
Author Aff i liations: Department of Surgery, Queen Mary Hospital, The University of Hong Kong, 102 Pok Fu Lam Road, Hong Kong, China (Dai WC, Chok KSH, Cheung TT, Chan ACY, Chan SC and Lo CM)
Wing Chiu Dai, MBBS, Department of Surgery, Queen Mary Hospital, The University of Hong Kong, 102 Pok Fu Lam Road, Hong Kong, China (Tel: +852-22553025; Fax: +852-28165284; Email: jeffdai02@yahoo.com.hk)
© 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(17)60039-0
Published online July 13, 2017.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Indocyanine green fl uoroscopy and liver transplantation: a new technique for the intraoperative assessment of bile duct vascularization
- Effects of multimodal fast-track surgery on liver transplantation outcomes
- Characteristics of recipients with complete immunosuppressant withdrawal after adult liver transplantation
- Predictive value of C-reactive protein/albumin ratio in acute pancreatitis
- Bilioenteric anastomotic stricture in patients with benign and malignant tumors: prevalence, risk factors and treatment
- Interaction between insulin-like growth factor binding protein-related protein 1 and transforming growth factor beta 1 in primary hepatic stellate cells
