Research progress in the total knee arthroplasty
2016-11-08FeiLiu
Fei Liu
. 综述 Review.
Research progress in the total knee arthroplasty
Fei Liu
Authors working place: 37996 TN,University of Tennessee,527 Andy Holt Tower,Knoxvill
Total knee arthroplasty(TKA)is one of the reliable options for patients with end stage osteoarthritis.The robots,patient specific cutting guides,preoperative software and computer-assisted surgery have been introduced in order to improve the accuracy of operative prosthesis positioning in TKA.Therefore,optimal restored normal kinematics can be achieved.Overall limb alignment is taken as critical standard to obtain a successful outcome of TKA.Some studies suggested that the improvements in treatments for TKA may lead to optimal clinical outcomes and longer implant survivorship,while some other studies suggest that these technologies may not make a difference for well trained and high volume surgeons.To better understand the subtle nature of such treatments,the effect of robots,patient specific cutting guides,preoperative software and computer-assisted surgery have been reviewed.Outcomes of the total knee arthroplasty and future trend outlook also have been discussed.Although some criteria of the TKA(i.e.lower limb alignment)can be fulfilled via these technologies,long-term follow-up studies on patients’ satisfaction,complications and clinical outcomes are needed.
Arthroplasty,replacement,knee;Knee prosthesis;Knee joint;Arthroplasty,replacement;Total knee arthroplasty
Total knee arthroplasty(TKA)has been widely considered as one of the most successful surgical performances in treating primary osteoarthritis.The demand for TKA has increased significantly over the past few decades and it is estimated that in the USA itself,the demand for TKA will grow 673% from 2005 to 2030,which accounts for 524 600 and 3480 000 respectively[1-2].With the increasing number of TKA,it is necessary to keep TKA reliable.However,it is reported that nearly19% of patients remain dissatisfied post TKA[3].Possible reasons could be pain and revision due to wear,loosening and instability.There are some key factors affecting the durability and long-term survivorship of TKA,such as lower limb alignment,component positioning,patient characteristics and soft tissue balancing[4-5].Amongst them,implant positioning and lower limb alignment should be controlled precisely[6].As the malposition of the implants usually result in unsatisfactory clinical outcomes in TKA,rotational malalignment leads to impaired patellar tracking,stability and joint biomechanics[7].
To launch new means for enhanced outcomes of primary TKA and reduced proportion of revision TKA,implants have been produced with improved designs,sizing and material selections[8].However,the most recent advance in TKA has involved the digital instrumentations,which have become one of the mainstay of the orthopedic surgical rooms[9].The most prominent technologies currently used in TKA are
全膝关节置换术的研究进展 刘非 University of Tennessee,527 Andy Holt Tower,Knoxvill,TN,37996
robots,patient specific cutting guides,preoperative software and computer-assisted surgery.It is critical that both clinical efficacy and cost effectiveness of these technologies should be fully evaluated with the aim of providing valid and affordable treatments for the patients.
By using PubMed,a cursory search has been conducted and 819 peer reviewed papers have been collected regarding robots,patient specific cutting guides,preoperative software and computer-assisted surgery in TKA.Despite the adequate volume of literature,most studies have shortcomings that result in knowledge gaps about each treatments.Additionally,published studies on the accuracy achieved with such technologies sometimes contradict each other when compared to manual instrumentations.
Therefore,a systematic review about the development of robots,patient specific cutting guides,preoperative software and computer-assisted surgery has been done for better interpretation of these treatments.The historical perspective,mechanical axis,component positioning,center of rotation and cost-effectiveness of each technique have been assessed and compared in this paper.As the variability in means and data is high,all comparisons have been executed in qualitative manner.
Surgical Robots
Since introduced over 20 years ago,surgical robotic systems have been designed for improved accuracy of the implant placement by enhancing the surgeon’s ability to reduce the less-accurate freehand surgical errors[10].The surgical tools are still under surgeons’ control and those tools are positioned by the robotic system based on a detailed preoperative plan[10-12].
Although safety concerns have been risen,surgical robotics have undergone obvious improvements[13-16].For example,robotic-assisted surgery has been most popular in total and unicompartmental arthroplasty(UKA)total hip arthroplasty(THA)and TKA,which again has greater accuracy but similar clinical outcomes when compared with conventional techniques.Other than robotics applied in TKA,there are several other manufacturers who provide robotics for spine surgeries,such as ROSA System[17],Mazor[18]and Tinavi[19].
As shown in Tab.1,mainly two types of robotic systems have been summarized,including a robotic arm,robotic-guided cutting jigs,and robotic milling systems with a diversity of different navigation strategies using autonomous or haptic control instruments.It has been studied that semi-active haptic robotics are able to provide intraoperative tactile feedback to the surgeons[20].In terms of the radiographic outcomes,reduced malalignment of the lower limb and improved tissue balance have been found[12].
Abbreviation: TKA,total knee arthroplasty; THA,total hip arthroplasty; UKA,unicompartmental knee arthroplasty.
As shown in Fig.1,the MAKO robotic system is a haptic,CT based surgical system for UKA,TKA and THA applications[21].A preoperative surgical plan is used for identifying the size and position of the components and bony resection according to a patient’s anatomy.During the surgical process,the robotic system gives semiautonomous haptic feedback to avoid bone resection out of the surgical plan[10].Initially used in UKA applications,MAKO has received FDA approval for TKA applications recently and serve as an integrated closed system[15,21].
As shown in Fig.2,ROBODOC robotic system is an autonomous,CT based surgical system for TKA and THA applications[12].Clinically used in1992,ROBODOC is the first robotic system for joint arthroplasty[10].The surgical markers are utilized as a reference as the ROBODOC system is located to the patient and the surgeon is able to check where the robot is milling[12].
Liow et al.have assessed the mechanical axis accuracy and mechanical outliers by using the ROBODOC robotic surgical and conventional instrumentation in TKA process.The difference between preoperative and postoperative alignment is statistically significant for ROBODOC method and conventional method(for joint line outliners > 5 mm,ROBODOC method generates 3.23% joint line outliers while conventional method generates 20.6% joint outliers,P = 0.049)[29].However,it is also reported that compared to conventional TKA,ROBODOC system does obtain different short-term functional outcomes and quality of life.It is suggested that subtle improvement of quality of life can be improved and the measurement of quality of life is more sensitive than functional outcomes for evaluating the effect of robotic surgical process and conventional TKA instrumentations[14].
Early studies have indicated that by using robotic systems,mechanical alignment can be obtained accurately and constantly,which can contribute to longer survivorship of the knee implants[12,15].However,it cannot be ignored that the critical debate over the usage routine of surgical robotic systems,such as additional cost and longer operation times.It is reported that the investment of a robotic surgical system was€ 400 000(~ $ 545 000)and the operating cost per case was€1000(~ $1360)[12].
Such additional cost might result in resistance to accept the new technology.
Patient specific cutting guides
In the beginning of 21st century,the PSI was developed for several considerations:(1)To make the expense of CAS reduced and the complex protocol associated with registering makers simplified[9,30-31].(2)To help place the components of femur and tibia implants accurately[8-9].(3)To reduce the surgical period,blood loss and wound area of the patients[8,32].
The workflow of PSI is summarized below:
● 2D CT / MRI data acquisition;
● 3D model reconstruction;
● Bony resection simulation;
● PSI cutting guide design;
● 3D Printing;
● Application in TKA.
Allied with the preoperative CT or MRI performed on the knees of the patients.PSI has been introduced as a means of making accurate bone cuts through 3D printing technique[8,32-33].With a specific software program as shown in Tab.1,engineering stuff members of the medical device companies can transform the 2D images into 3D models based on each patient’s unique anatomy.With these reconstructed 3D models,the anatomical landmark of patients’ knees can be identified conveniently.

Tab.1 The summary of surgical robots,patient specific cutting guide and preoperative plan software for THA at the moment of publishing
Based on the reconstructed 3D models,a preoperative plan is generated with resected surface of femur and tibia by specific software(i.e.mimics,and Arigin3D Surgical Templating)and then provided to the surgeons for evaluation,modification and conformation[8,22].As Fig.3 shown,the preoperative plan with bony resection is executed by Arigin3D Surgical Templating.
After the surgical plan is approved,customized cutting guides designed to fit patients’ knees are ready to produce.The PSI cutting guide are manufactured by 3D printing technology.Depending on the design software and production means used,it could take 3 weeks[8]or1 day[22].Fig.4 demonstrated five current cutting guides available on the market[8,22].When the surgery is performed,the PSI cutting guides are utilized to obtain accurate location of pins for the primary distal femoral and proximal tibial resection.The postoperative results can be evaluated using radiography[1,28,34].

Fig.1 Current typical roboticsystem savailable for TKA a: MAKO robotic system;b: ROBODOC robotic system

Fig.2 Illustration of ROBODOC robot milling the femur in TKA
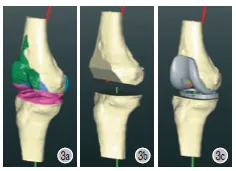
Fig.3 The pre-operative plan with bony resection is executed by Arigin 3D Surgical Templating a: Simulation of bony resection; b: Result of bony resection; c: Installation of components
Qiu,et al.[22]have investigated the accuracy of PSI guides based on the assistance of medical image reconstruction software,surgical templating software and 3D printing technique.It has been found that the Arigin3D Pro software can reconstruct a 3D model of the lower limb efficiently.The preoperative plan and PSI design software Arigin3D.
Surgical Templating software can accurately pinpoint associated lower limb axis,including limb alignment,rotation axis of the femur and osteotomy reference point.PSI cutting guide fit femoral condyle and tibial plateau tightly without significant movement during midst operation.The deviation of patients’ lower limb alignment has been found to be less than 3° post operation.
In terms of guiding landmark registration,it is reported that compared to PSI,conventional TKA procedure has difficulties to predict the position of lower limb alignment,size of the implant component and boney resections precisely[22-24,32].However,divided opinion from some other studies suggested that routine use of PSI is not recommended due to extra cost,waiting time and no significant radiological and clinical benefit among PSI,conventional instrumentation or CAS[1,35-36].
Patient-specific instrumentation aims to improve threedimensional implant positioning while reducing overall costs of instrumentation[7].The precise orientation and component rotation of the pre-defined template can be achieved,leading to decreased number of instrument trays and improved component alignment.Less blood loss and fat embolism can be caused as that the PSI does not rely on the intramedullary rods[10,13].Thus,it is possible that the PSI will be a promising alternative method of CI due to the projected increase of PSI applications[2].
However,better understanding on PSI is needed as both advantages[3-4,13,32]and disadvantages[13,37-39]have been reported in terms of the surgical efficiency,blood loss,and alignment.For consistent assessing of PSI,several aspects should be considered,such as the experience of surgeons,the technical consistencies in anatomic landmarking,the accuracy of patient-specific guides,processing errors and manufacturing errors[40].
Preoperative plan software
Preoperative planning is a critical step of TKA for accurate bony resection and reproducible functional outcomes[26].Preoperative plan software in TKA help surgeons determine the need of non-standard implants,prophesies the bony resections and anticipate the intraoperative plan.Herein,the preoperative plan software refer to 2D digital radiography and 3D templating preoperative plan software[41].Tab.1 showcases the preoperative plan software for THA at the moment of publishing.
The use of such software in TKA continues to become widespread for several reasons:(1)For the financial considerations,the use of digital templating has recently increased due to their advantages compared to picture archiving and communication system(PACS)[26,42].(2)They can execute the surgical plan with streamlined intraoperative instruments,such as the surgical trays can be minimized based on the preoperative plan.(3)They can improve preoperative planning by reducing errors in component sizing and alignment[26,28].
It is reported that by using radiographic based 2D preoperative surgical software among 48 cases of TKA,54% of implants have been predicted correctly,92% of implants have been predicted within1 size of the final implant and 99% of implants have been predicted within 2 size of the final implant[42].
Kobayashi A et al.have compared the accuracy of 2D and 3D preoperative planning software by analyzing100 primary TKA cases.Accuracies regarding the predicted and actual implant sizes were determined for each procedure.The 3D preoperative planning software has been found to be more accurate(59%)than the 2D preoperative planning software(56%)in predicting implant size,but no statically significant difference has been found(P = 0.67)[41].

Fig.4 Current PSI cutting guides available on the market a: PSI,Zimmer Biomet; b: Surgical templates,Arigin Medical Co; c: GMK MyKnee,Medacta International; d: TruMatch,DePuySynthes; e: Visionaire,Smith& Nephew
Recent attention has been paid to an emerging preoperative planning approach using Arigin3D Surgical Templating software.Medical image data of patients were collected using CT or magnetic resonance scanning equipment.The 3D reconstruction of the bone was conducted by 2D medical image processing technology.The preoperative plan has been conducted on the software platform as the associated lower limb axis,including limb alignment,rotation axis of the femur and osteotomy reference point can be identified precisely.The deviation of patients’ limb alignment have been limited within 3° post TKA[22-24].Allied with 3D printing technique,Arigin 3D Surgical Templating software can generate PSI for TKA,which is discussed in the following section.
Computer-assisted surgery
Computer-assisted surgery(CAS)or computer navigation has been firstly reported to improve the precision of the implant positioning and lower-limb alignment in1997 by Krackow et al[43].Since then,various CAS systems have been developed[6,21].In The CAS for TKA is comprised of navigation tools,tracker,monitor and work station; usually the CAS can be classified into two types of systems according to its compatibility with other instrumentation manufactures.Open systems of CAS can work regardless of the manufactures while the closed systems of CAS can only work with specific instruments[9].
The workflow of the CAS is summarized below:
● The patients enter surgery;
● The registration of makers define the position in space based on the 3D model;
● The CAS triangulates the location of each marker;
● Makers provide information regarding location of anatomic landmarks,mechanical axes,component positioning and center of rotation.
During the navigation process,the accuracy of all marker pins placement in distal femur and proximal tibia is important for construction the anatomy by CAS[9].It has been reported that when compared with manual,non-computer navigation procedure,CAS can guide the positioning of the cutting jib with less errors in the sagittal plane for tibia and femur component of the knees.Novak EJ et al.have reported that by using CAS,coronal alignment precision(within 3 degrees of neutral mechanical axis)has been improved by14%,and revision rates at fifteen years with coronal malalignment have been increased from 4.7% to 54%[4].
CAS can be also used for examining the bone resection and implantation amid TKA[44].Such successful outcomes are believed to be highly dependent on reproducible anatomic accuracy.Most short-term studies have demonstrated superior accuracy when compared with conventional techniques[9].
From the aspect of financial consideration,the expense of CAS of navigation is quite high and there is a debate on the cost-effectiveness of the CAS procedure[4,30,32].A typical system expense is consisted of the hardware,the software and annual service fee.It has been reported that CAS could cause an additional cost of $1500 per procedure and the incremental cost of could reach up to $45,554 annually[4].Some studies have attempted to analyze the cost-effectiveness by assessing the frequency of use and low volume units do not seem to get financial benefit from the CAS systems as CAS is an expensive technique which may only be cost-effective for high-volume hospitals[30,45].However,some other published papers have used a variety of clinical outcomes introducing uncertainty in determining the cost-effectiveness,even though CAS has some advantages over conventional instrumentation[9,46].For example,learning and retention of CAS for beginners could be complicated and very few studies have shown better clinical outcomes.For the surgeons who perform high volume operations,CAS has not improved them to a greater degree as compared to the lower volume surgeons[9,12,30].
Recently,novel navigation systems have been developed using accelerometer electronic components such as the iASSIST system by Zimmer Biomet.As shown in Fig.5,it relies on accelerometer-based navigation instead of computed tomographyguided,image-based,or imageless navigation technologies used in most CAS systems[47-48].

Fig.5 The use of iASSIST to guide the tibial resection.When compared to computer assisted systems,no significant differences has been found in clinical outcomes or satisfaction rates six months post operation.The duration of surgery was significantly shorter in the iASSIST group,while added cost of iASSIST system was approximately $1000 per operation[47]
Discussions
Poor survivorship of the knee implants and patients dissatisfaction have been considered associated with the component malalignment,which result in micro motion and loosening[15].The purpose of this study is to evaluate the functional,clinical and financial outcomes of using treatments.The digital techniques such as CAS,preoperative plan software,PSI and robotic systems have made it possible for surgeons to simplify the conventional TKA procedure and lessen the impact of associated subjectivity.To emerge these treatments,various criteria should be considered,not only their accuracy and resultant outcomes,but also their impact on providers to deliver the best and most cost-effective care to as many patients as possible.
In this article,we have conducted a systemic review on whether or not the proposed benefits of implementing these technologies would outweigh the necessary additional cost.Comparisons have been made between each technique.The accuracy the execution of preoperative plan and the deviations of post-operative parameters have been discussed.
CAS has been used to attempt to obtain optimized TKA outcomes.It is suggested that by using computer navigation,type II and type III valgus deformity,which accounts for10% of the TKA could be treated with good mid-term and radiograph outcomes of regardless of the medial or lateral approach[37].However,more studies of general TKA have questioned the waiting time,mechanical alignment and positioning effect of CAS,as no better results have been obtained[9,49].
Surgical templating software,PSI and robotic systems have been developed to conquer the shortcomings of the CAS.Studies on functional outcomes of such new technologies suggest that operative time,incision length,and number of used instrument trays could be decreased by using PSI[32,50].
Accompanied by navigation software,CAS used for primary TKA could be applied for revision TKA and the surgeons can modify the preoperative plan[51].Preoperative surgical planning software have been used as effective means to predict the size of the TKA implants[27].Both 2D and 3D digital templating software have provided feasible options for saving surgical time.Additionally,it is reported that the impact of training level showed excellent reliability among all training level of examiners[42].
Compared to conventional instrumentation,robotic systems in TKA have been found to be useful for improved joint line accuracy; however,there are no significant difference in terms of complications and clinical outcome[14,29].It is suggested that in the long run,robotic technology will be introduced to every industry,including medical care industry,which will result in increased production capacity,reduced cost and optimized accuracy[10,20].However,before agreeing with the cautions optimistic prediction,many questions are still needed to be answered,such as(1)how is the handling of soft tissues? It could influence the postoperative function of the knee.(2)Whether the system should be open to different implants[4,52]?
It is well known that utilizing new technologies will bring necessary additional cost.Against this background and with respect to further cost-benefit analyses,each new technology for TKA applications should be reviewed critically.For the case of CAS,it is believed that the goal of cost-savings can be met the additional cost is less than $629 per surgical procedure[4].PSI has been developed to change the impact of high cost brought by CAS,and it is reported that the profit could increase1.45 fold by switching CAS to PSI[9,53-54].In terms of financial consideration of Robotic surgical systems,it has been reported that it could cost €1000(~ $1360)each case[12].As the techniques are still developing and quite new,systemic analysis should be executed before wide adoption[7,16,52,55].
The limitations to this review article include:(1)the treatment means mentioned in this review are generally image data dependent,they are only as good as the data they have.However,when surgeon perform the TKA,they do not always have good data due to various reasons.(2)Knee implants with different types were used in the original studies.Surgical plans could be different due to such reasons.(3)The mechanical axis is widely used to quantify the limb alignment[1],however,mechanical axis has been doubted to be too simplistic as a parameter and the kinematic alignment may be a considerable alternative[36].(4)Quantitative analysis has not been performed due to the variability of the scope of surgical process and topics discussed would have made statistical evaluation difficult.To avoid improper application of statistics,only qualitative analysis has been used.(5)To date,no long-term results are available regarding a definitive statement about lower revision rates,declining numbers of aseptic loosening,cost-effectiveness and clinical outcomes following CAS,preoperative plan software,PSI and robotic systems.
To conclude,the short-term functional results warrant further analysis regarding surgical and clinical outcomes and cost of the treatments technologies are necessary.Until the day that those new technologies showcase a definite mid- and long-term benefit,manual TKA is still the surgical process with cost-effectiveness and good value to patients.
Reference
[1]Cavaignac E,Pailhé R,Laumond G,et al.Evaluation of the accuracy of patient-specific cutting blocks for totalknee arthroplasty: a meta-analysis.Int Orthop,2015,39(8):1541-1552.
[2]Shang P,Zhang L,Hou Z,et al.Morphometric measurement of the patella on 3D model reconstructed from CT scan images for the southern Chinese population.Chin Med J(Engl),2014,127(1):96-101.
[3]Bourne RB,Chesworth BM,Davis AM,et al.Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res,2010,468(1):57-63.
[4]Novak EJ,Silverstein MD,Bozic KJ.The cost-effectiveness of computer-assisted navigation in total knee arthroplasty.J Bone Joint Surg Am,2007,89(11):2389-2397.
[5]Jiang J,Kang X,Lin Q,et al.Accuracy of patient-specific instrumentation compared with conventional instrumentation in total knee arthroplasty.Orthopedics,2015,38(4):e305-313.
[6]Sharkey PF,Lichstein PM,Shen C,et al.Why are total knee arthroplasties failing today--has anything changed after10 years? J Arthroplasty,2014,29(9):1774-1778.
[7]Mannan A,Smith TO.Favourable rotational alignment outcomes in PSI knee arthroplasty: a level1 systematic review and meta-analysis.Knee,2016,23(2):186-190.
[8]Camarda L,D’Arienzo A,Morello S,et al.Patient-specific instrumentation for total knee arthroplasty: a literature review.Musculoskeletal Surg,2015,99(1):11-18.
[9]Leone WA,Elson LC.A Systematic Literature Review of Three Modalities in Technologically Assisted TKA.Anderson CR.Adv Orthop,2015,2015:719091.
[10]Jacofsky DJ,Allen M.Robotics in Arthroplasty: A Comprehensive Review.J Arthroplasty,2016,pii: S0883-5403(16)30164-4.
[11]Van der List JP,Chawla H,Pearle AD.Robotic-Assisted Knee Arthroplasty: An Overview.Am J Orthop(Belle Mead NJ),2016,45(4):202-211.
[12]Liow MH,Chin PL,Tay KJ,et al.Early experiences with robot-assisted total knee arthroplasty using the DigiMatch™ROBODOC® surgical system.Singapore Med J,2014,55(10):529-534.
[13]Lonner JH.Robotically assisted unicompartmental knee arthroplasty with a handheld imagefree sculpting tool.Orthop Clin North Am,2016,47(1):29-40.
[14]Liow MH,Goh GS,Wong MK,et al.Robotic-assisted total knee arthroplasty may lead to improvement inquality-of-life measures: a 2-year follow-up of a prospective randomizedtrial.Knee Surg Sports Traumatol Arthrosc,2016.
[15]Banerjee S,Cherian JJ,Elmallah RK,et al.Robotic-assisted knee arthroplasty.Expert Rev Med Devices,2015,12(6): 727-735.
[16]Sparmann M,Wolke B.Value of navigation and robot- guided surgery in total knee arthroplasty.Orthopade,2003,32(6): 498-505.
[17]Chenin L,Peltier J,Lefranc M,et al.Minimally invasive transforaminal lumbar Interbody fusion with the ROSA(TM)Spine robot and intraoperative flat-panel CT guidance.Acta Neurochir(Wien),2016,158(6):1125-1128.
[18]Dreval’ ON,Rynkov IP,Kasparova KA,et al.Results of using Spine Assist Mazor in surgical treatment of spine disorders.Zh Vopr Neirokhir Im N N Burdenko,2014,78(3):14-20.
[19]Wang J,Han W,Lin H,et al.Femoral fracture reduction with a parallel manipulatorrobot on a traction table.Int J Med Robot,2013,9(4):464-471.
[20]Netravali NA,Shen F,Park Y,et al.A perspective on robotic assistance for knee arthroplasty.Adv Orthop,2013,2013: 970703.
[21]Roche M.Robotic-assisted unicompartmental knee arthroplasty: the MAKO experience.Clin Sports Med,2014,33(1):123-132.
[22]Qiu B,Tang B,Deng B,et al.Intelligentized surgery based on 3D printing technology for personalized total knee athroplasty.Chin J Orthop Trauma,2016,18(1):35-41.
[23]Qiu B,Zhang M,Tang B,et al.A novel intergrated patient specific instrumentation system and its application for total knee arthroplasty.Chin J Orthop,2016,36.
[24]Qiu B,Zhang M,Tang B,et al.Total knee arthroplasty based on the assistance of three- dimensional-printing personalized surgical navigation template.Chin J Tiss Eng Res,2015,19:7731-7735.
[25]Mattei L,Pellegrino P,Calò M,et al.Patient specific instrumentation in total knee arthroplasty: a state of the art.Ann Transl Med,2016,4(7):126.
[26]Hsu AR,Gross CE,Bhatia S,et al.Template-directed instrumentation in total knee arthroplasty: cost savings analysis.Orthopedics,2012,35(11):e1596-1600.
[27]Levine B,Fabi D,Deirmengian C.Digital templating in primary total hip and kneearthroplasty.Orthopedics,2010,33(11):797.
[28]Peek A,Bloch B,Auld J.How useful is templating for total knee replacement component sizing.Knee,2012,19(4): 266-269.
[29]Liow MH,Xia Z,Wong MK,et al.Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis.a prospective randomised study.J Arthroplasty,2014,29(12):2373-2377.
[30]Calliess T,Ettinger M,Windhagen H.Computer-assisted systems in total knee arthroplasty.Useful aid or only additional costs.Orthopade,2014,43(6):529-533.
[31]Howell SM,Kuznik K,Hull ML,et al.Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients.Orthopedics,2008,31(9):857-863.
[32]Watters TS,Mather R,Browne J,et al.Analysis of procedurerelated costs and proposed benefits of using patient-specificapproach in total knee arthroplasty.J Surg Orthop Adv,2011,20(2):112-116.
[33]Xiao J,Wang C,Zhu L,et al.Improved method for planning intramedullary guiding rod entry point in total knee arthroplasty.Arch Orthop Trauma Surg,2014,134(5):693-698.
[34]Kniesel B,Konstantinidis L,Hirschmuller A,et al.Digital templating in total knee and hip replacement: an analysis of planning accuracy.Int Orthop,2014,38(4):733-739.
[35]Yan CH,Chiu KY,Ng FY,et al.Comparison between patientspecific instruments and conventional instruments and computer navigation in total knee arthroplasty: a randomized controlled trial.Knee Surg Sports Traumatol Arthrosc,2015,23(12): 3637-3645.
[36]Calliess T,Bauer K,Stukenborg-Colsman C,et al.PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective,randomized study.Knee Surg Sports Traumatol Arthrosc,2016.
[37]Kornilov N,Kulyaba T,Petukhov A,et al.Computer navigation helps achieving appropriate gap balancing and restoration of alignment in total knee arthroplasty for fixed valgus knee osteoarthritis irrespective of the surgical approach.Acta Orthop Belg,2015,81(4):673-681.
[38]Conteduca F,Iorio R,Mazza D,et al.Patient-specific instruments in total knee arthroplasty.Int Orthop,2014,38(2): 259-265.
[39]Schwarzkopf R,Brodsky M,Garcia GA,et al.Surgical and functional outcomes in patients undergoing total knee replacement with patient-specificimplants compared with“off-the-shelf” implants.Orthop J Sports Med,2015,3(7): 2325967115590379.
[40]Fu H,Wang J,Zhou S,et al.No difference in mechanical alignment and femoral component placement between patientspecific instrumentation and conventional instrumentation in TKA.Knee Surg Sports Traumatol Arthrosc,2015,23(11): 3288-3295.
[41]Kobayashi A,Ishii Y,Takeda M,et al.Comparison of analog 2D and digital 3D preoperative templating for predicting implant size in total knee arthroplasty.Comput Aided Surg,2012,17(2):96-101.
[42]Hsu AR,Kim JD,Bhatia S,et al.Effect of training level on accuracy of digital templating in primary total hip and knee arthroplasty.Orthopedics,2012,35(2):e179-183.
[43]Krackow KA,Serpe L,Phillips MJ,et al.A New Technique for Determining Proper Mechanical Axis Alignment During Total Knee Arthroplasty: Progress Toward Computer-Assisted TKA.Orthopedics,1999,22(7):698-702.
[44]Chua KHZ,Chen Y,Lingaraj K.Navigated total knee arthroplasty: is it error-free? Knee Surg Sports Traumatol Arthrosc,2014,22(3):643-649.
[45]Gothesen O,Slover J,Havelin LI,et al.An economic model to evaluate cost- effectiveness of computer assisted knee replacement surgery in Norway.BMC Musculoskelet Disord,2013,14:202.
[46]Venkatesan M,Mahadevan D,Ashford R.Computer-assisted navigation in knee arthroplasty: a critical appraisal.J Knee Surg,2013,26(5):357-361.
[47]Goh GS,Liow MHL,Lim WS,et al.Accelerometer-based navigation is as accurate as optical computer navigation in restoring the joint line and mechanical axis after total knee arthroplasty: a prospective matched study.J Arthroplasty,2016,31(1):92-97.
[48]Desseaux A,Graf P,Dubrana F,et al.Radiographic outcomes in the coronal plane with iASSIST™ versus optical navigation for total knee arthroplasty: A preliminary case-control study.Orthop Traumatol Surg Res,2016,102(3):363-368.
[49]Shin Y,Kim H,Ko Y,et al.Minimally invasive navigationassisted versus conventional total knee arthroplasty: a metaanalysis.Knee Surg Sports Traumatol Arthrosc,2016 Feb 9.[Epub ahead of print].
[50]Noble JW,Moore CA,Liu N.The value of patient-matched instrumentation in total knee arthroplasty.J Arthroplasty,2012,27(1):153-155.
[51]Hoffart HE,Dinges H,Kolbeck S,et al.Novel computerassisted method for revision arthroplasty of the knee.World J Orthop,2015,6(10):821-828.
[52]Adili A.Robot-Assisted Orthopedic Surgery.Semin Laparosc Surg,2004,11(2):89-98.
[53]Lionberger DR,Crocker CL,Chen V.Patient Specific Instrumentation.J Arthroplasty,2014,29(9):1699-1704.
[54]Jauregui JJ,Cherian JJ,Kapadia BH,et al.Patients pecific instrumentation in total knee arthroplasty.J Knee Surg,2014,27(3):177-183.
[55]Parratte S,Blanc G,Boussemart T,et al.Rotation in total knee arthroplasty: no difference patient-specific and conventional instrumentation.Knee Surg Sports Traumatol Arthrosc,2013,21(10):2213-2219.
(本文编辑:李贵存)
10.3969/j.issn.2095-252X.2016.10.009
R687.4
全膝关节置换术(total knee arthroplasty,TKA)是一种治疗骨关节炎的有效方法。近年来,为了提高 TKA 的假体的位置精度,手术机器人、个性化手术导板、术前规划软件和计算机导航系统被广泛使用。重建良好的下肢力线被认为是判断 TKA 是否成功的标准之一。有研究表明,手术机器人、个性化手术导板、术前规划软件和计算机导航系统的使用可以提高手术效果,延长假体使用寿命。但也有另外一些研究表报道了以上方法对经验充分、手术数量多的医生并没有显著提高手术效果。此综述的目的是进一步深入理解手术机器人、个性化手术导板、术前规划软件和计算机导航系统对膝关节手术效果的影响。目前以上方法可以满足 TKA 的指标(如下肢力线重建),但是仍需要关于长期手术效果和患者满意度的随访报道来进一步确认手术机器人、个性化手术导板、术前规划软件和计算机导航系统的有效性。
关节成形术,置换,膝;人工膝关节;膝关节;关节成形术,置换
(2016-08-16)