A historical review of total knee arthroplasty development
2016-11-05HarrisonCuiWeiWangGuoanLi
Harrison Cui Wei Wang Guoan Li
A historical review of total knee arthroplasty development
Harrison Cui Wei Wang Guoan Li
Authors working place: Bioengineering Laboratory,Department of Orthopaedic Surgery,Massachusetts General Hospital and Harvard Medical School,Boston,MA,USA(Harrison Cui,Guoan Li).Department of Orthopaedic Surgery,The second affiliated hospital,Xi’an JiaoTong University(Wei Wang)
Introduction
Total knee replacement has become one of the most commonly performed surgeries in the United States with an estimate of 4.7 million Americans living with knee implants as of 2010[1].As the amount of arthritic knees rises with the growing lifespan of humans due to advanced medicine,the total knee arthroplasty plays an increasingly important role in public health.As of 2030,it is estimated that 3.48 million total knee arthroplasties will be performed annually[2].Recently,patients younger than 60s have begun to choose TKA as an option for treatment of severe knee diseases[3].These patients have higher expectation for quality of life and require prolonged component longevity.To meet the increasing patient needs,various design concepts have been proposed that target different geometric features,motion patterns,or functional characteristics of human knees,including PCL retaining,PCL substituting,mobile bearing,medial pivoting,bicruciate retaining,high flexion,etc.To fully understand the different development rationales of different components,it is important to understand the historical development of the total knee arthroplasty so that we can continue to improve upon the modern total knee arthroplasty to match the rising demand and increasing patient expectations.In this article,we intend to present a historical review of TKA development and discuss future developments of TKA designs.
Early interposition arthroplasty
In the late19th and early 20th century before the advent of total knee arthroplasty,practitioners resorted to interposition arthroplasty to repair the knee joint’s articular surface.This method was first offered by Verneuil in1860 who proposed the use of soft tissue to repair the diseased knees[4].Initially,surgeons like Murphy and Campbell resorted to autotransplanting tissue such as fascia lata,fat,and prepatellar bursa in the interposition arthroplasty[5-6].In Murphy’s case,he sutured a flap of the patient’s fat and fascia lata over the articulating surfaces of the femur to prevent bony contact with the tibia and patella[5].However,the soft tissues yielded poor results,and practitioners continued to experiment with other materials,such as chromicized pig bladder,nylon,cellophane,and metal,in interposition arthroplasty[4].Such materials yielded similar poor results as did the soft tissues,as patients with Baer’s chromicized pig bladder had issues with fever,
Total knee arthroplasty(TKA)has evolved significantly into one of the most widely performed and important surgeries today as the treatment modality for end-stage osteoarthritis or other severe diseases of the knee.This paper briefly reviews the history of TKA development and discusses possible future development of TKA designs.
Arthroplasty,replacement,knee;Knee prosthesis;Knee joint;Arthroplasty,replacement;Total knee arthroplasty
全膝关节置换术的研究进展 【摘要】 全膝关节置换(total knee arthroplasty,TKA)目前为止发展迅速,已成为治疗终末期膝骨关节炎或其它严重膝关节疾患的一种临床上广泛应用的、重要的治疗方法。现就TKA 的发展史及将来 TKA 设计的进展综述如下。
Hinge components
During the1950s,practitioners began to abandon the interposition surface arthroplasty which provided poor outcomes and pursued the mechanical hinged design.The first hinged knee design constructed out of ivory and cemented with colophony,pumice,and plaster of Paris was proposed by Themistocles Gluck in1890(Fig.1)[12].Although Gluck’s prosthesis enjoyed short-term success in his patients,the choice of materials for the implant was poor and the patients suffered from chronic infection in the long-term[12].Thus,the mechanical hinged design was set aside until the1950s.One of the first hinged designs of the time period was the Walldius Prosthesis[4],introduced in1951(Fig.2).The original design employed tibial and femoral components connected by a stainless steel transverse axle with three stabilizing pins extending from the implant’s central portion to be inserted into the medullary cavities and the condyles[13].The implant’s femoral component also has a convex anterior surface for the patella to move alongside[13].The design was initially constructed out of acrylic.However,the prosthesis was later revised to be made out of the more durable stainless steel and cobalt chrome alloy after the acrylic implant fractured[4].
Various modifications to the Walldius hinge design were made by surgeons,including Seddon,Shier,McKee,Young,et al,throughout the1950s and1960s[4].In1970,a group of orthopedic surgeons in Paris developed the Guepar hinged prosthesis to correct some design flaws of the earlier Walldius variations[14].The prosthesis was designed with the goals of minimizing bone loss with less bone resection,reducing constraint for functional purposes,having the tibia roll under the femur in flexion,preserving patellar tracking,dampening contact between parts,and recreating normal knee axes with a valgus tilting of the femur stem[14].
Although the initial hinged prostheses in the1950s and1960s proved to obtain better clinical results than other knee arthroplasty designs of the time period,they suffered from many complications including infection,loosening,subsidence,fractures,skin necrosis,and more.These early hinged prostheses were designed to be highly constrained as to provide stability,but such constraint induced additional stress on the cemented locations of contact between the implant and the bone.This excessive stress contributed to early loosening of the implant.The highly constrained design also only allowed patients to perform simple flexion and extension.Furthermore,the early designs were composed completely from metal,creating metal-on-metal articulations that result in mechanical failure.The uniaxial rotation of these early simple hinge joints also generates high torsional loads that put pressure on the interfaces of contact and contribute to early loosening[15].Overall,the major complications of these early prostheses led to high early failure rates.
In1973,the spherocentric knee was introduced as the first rotating-hinge design[16]—a contained “ball in a socket” concept(Fig.3).The contained “ball in a socket”design allowed for rotational motion in all rotatory planes with condylar outriggers to limit the uncontrolled rotation to that of normal knee function[16].Like most other prostheses of the1970s and1980s,the spherocentric knee reduced the constraint of earlier prostheses by incorporating axial rotation and varus-valgus motion into its design[15].The introduction of polyethylene components in prostheses created metal-onplastic contact to reduce mechanical failure.Although the less constrained prostheses of the1970s and1980s generally had successful early outcomes,failures from infection,loosening,and fractures still occurred during the mid to long terms[15].In the1990s,the Finn,S-ROM,and Zimmer NexGen RHK Prostheses were introduced[15].These prostheses introduced modularity and multiple sizes to customize implants as well as deepened anterior femoral grooves for improved patellar tracking.The link between the tibial and femoral components in these modern hinged prostheses is also unweighted with most of the weight transferred through a conforming polyethylene bearing.Knee arthroplasties with hinged prostheses now constitute less than1% of all knee arthroplasties performed in the United States[15].Although less constrained unlinked designs are generally more favorable to constrained hinged designs,hinged prostheses are still necessary in the rare cases of soft tissue or bone deficiency.
Surface Replacements
The hinged design began to fall out of favor with the emergence of unlinked surface replacements in the early1970s.The first surface replacement was the polycentric knee introduced in1971 by Frank Gunston(Fig.4)[17].
Gunston attempted to simulate normal knee movement with his prosthesis with separate components and by maintaining all collateral and cruciate ligaments.Although the polycentric knee showed initial promising results,the prosthesis faced issues with loosening and infection[18].

Fig.1 Gluck’s ivory knee design(From Eynon-Lewis[12])
Three condylar surface replacement designs—the duo condylar prosthesis,the geometric prosthesis,and the anatomic total knee prosthesis—in the early1970s have laid the foundation of modern total knee arthroplasty.Developed by Peter Walker and colleagues at the Hospital for Special Surgery in1971,the duocondylar prosthesis had essentially no restraint and preserved the cruciate ligaments(Fig.5a)[19].The prosthesis consists of two unicompartmental metal surfaces for the medial and lateral femoral condyles joined anteriorly by a bar and a tibial component composed of two separate polyethylene implants[19].The duocondylar prosthesis showed problems with loosening of the all-polyethylene tibial component,instability of the knee,and patellofemoral joint crepitation[20].

Fig.2 Frontal and lateral view of the Walldius hinge prosthesis(From Fig.2 of Chapter 2 of The Adult Knee[4])

Fig.3 Spherocentric knee(From Matthews.L.S.[16])
The geometric knee introduced by Coventry and colleagues in1972 preserved the cruciate ligaments(Fig.5b)[21].Similar to the duocondylar prosthesis,the geometric knee consists of two Vitallium spherical surfaces joined by a bar and a concave polyethylene tibial plateau which receives the convex femoral component[21].However,the intrinsic constraint of the congruent-surfaced design caused rapid loosening[22].

Fig.4 Gunston’s polycentric knee design(From Gunston,F.H.[17])
Charles Townley developed the anatomic total knee prosthesis which retained both cruciate ligaments and introduced the patellar button in1972(Fig.5c)[23].Townley also explored various sizing options for patients’ knees in his prosthesis by offering five different sizes of the anatomic prosthesis[23].Similar to the duocondylar knee,the anatomic total knee prosthesis showed problems with loosening of the tibial component[23].
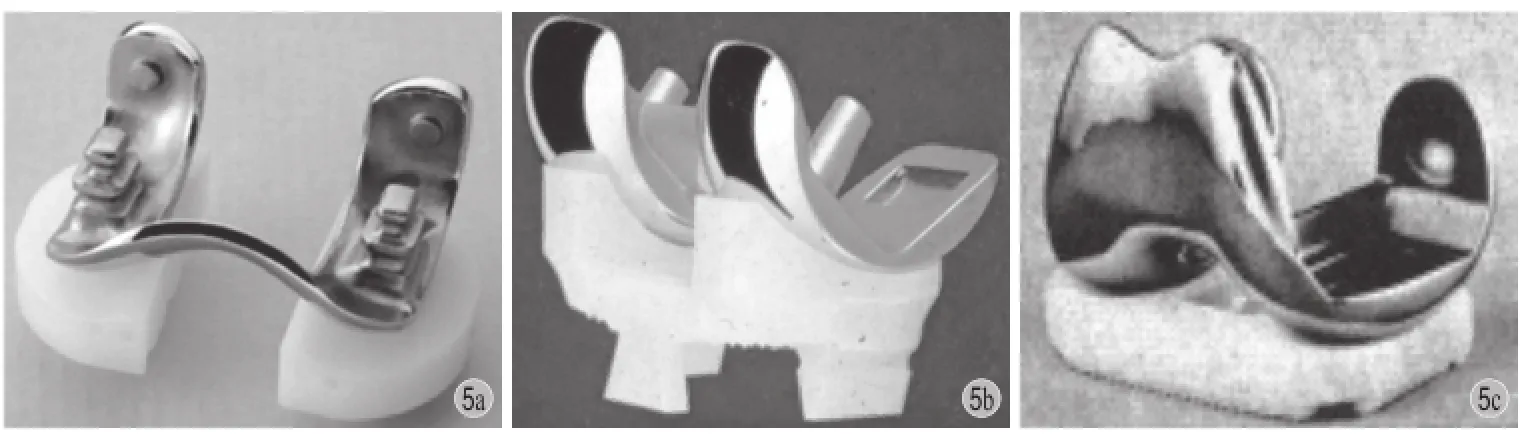
Fig.5 a: The duocondylar prosthesis; b: The geometric knee; c: The anatomic total knee(From Fig.8 of Chapter 2 of The Adult Knee[4])
The duocondylar prosthesis was later modified to the total condylar prosthesis in1973 by the Hospital for Special Surgery to resolve the issues of patellofemoral joint pain,loosening tibial components,and surgical techniques(Fig.6)[24].The total condylar prosthesis removes both cruciate ligaments and adopts a polyethylene patellar button as well as a central tibial stem.Most modern prostheses are largely based upon the total condylar knee.

Fig.6 Components of the total condylar knee
Diverging Design Philosophies
Several different design philosophies have emerged in the development of modern total knee arthroplasty.Beginning in the1970s and continuing into the present,knee prosthesis designers debated over the issue of maintaining normal knee kinematics with prostheses in the “kinematic conflict”[4].Thus,knee prostheses have diverged into two categories—functionaland anatomical.Prostheses of the functional approach typically resect the posterior cruciate ligament and have evolved into the posterior stabilized prostheses.Posterior stabilized prosthetic designs were developed to have a less technically demanding procedure,a more stable component interface,and a larger motion range[25].Prostheses of the anatomical approach attempt to preserve normal knee motion by retaining the posterior cruciate ligament and soft tissues constraint.Cruciate retaining prostheses were developed for the purpose of preserving more bone,having more normal knee kinematics,and allowing greater proprioception[25].Although each type of prosthesis has certain advantages over the other,studies are inconclusive as to whether one knee design is superior to the other.
Another divergence in knee prostheses was the introduction of mobile bearings in total knee arthroplasty.Major contributors to arthroplasty failures were polyethylene wear and loosening due to either high contact stress or high constraint force.Goodfellow and O’Connor first decided to tackle the issue of polyethylene wear in1976 with their Oxford knee prosthesis[4,26].The design employed a polyethylene tibial component composed of a freely moving meniscal bearing on a metal tray,but the implant encountered a new problem of a dislocated meniscal bearing[26].In a two to six year follow-up of one hundred twenty-five Oxford knee implants,Goodfellow et al.[26]reported that five knees required revision surgery due to dislocation of the meniscal bearing.
In1977 Fred Buechel and Michael Pappas resolved this issue by designing a rotating platform that performed the same function as the meniscal bearing in their low contact stress knee(Fig.7)[27].Through conformity and mobility in the tibiofemoral bearing surface,the mobile bearing design theoretically decreases polyethylene wear and loosening by reducing contact stress and constraint.However,survivorship studies of mobile bearing knee designs have not proven its superiority over fixed bearing designs,and surgeons are advised to choose based on their surgical experience and the patient’s age[28].
The method of bone fixation in knee arthroplasty is also a debated issue among orthopedics.The most common method of fixation for knee implants is the use of bone cement,polymethyl methacrylate,which was first approved by the FDA in the1970s.However,practitioners have begun to explore cementless fixation techniques as well as hybrid fixation techniques.In1980,David Hungerford developed the porous-coated anatomic prosthesis that introduced the cementless concept of bone ingrowth fixation[4].The technology of cementless implants is over three times more expensive than that of cemented implants,but cementless procedures potentially have reduced surgical times,preserve more bone stock,and are easier to revise[29-30].Bone cement is also potentially harmful to tissue and may cause thermal necrosis during polymerization[30].However,no evidence currently supports that one method of fixation produces superior results to the other.
Future Developments
Total knee arthroplasty has become one of the most successful procedures with survival rates of over 90% at follow up times of10 to 20 years[25].However,the growing demand for total knee arthroplasties prompts the need for improvement.Most modern arthroplasty failures are a result of aseptic loosening,instability,infection,and malalignment[31-32].Furthermore,studies suggest approximately one in five patients are not satisfied with the results of their knee replacements[33].There has also been a rise in total knee replacement among younger patients under 60 years of age who have the risk of higher failure rates due to their more physically demanding lifestyles[3].Another issue is that modern knee implants typically consist of a metal femoral component and a polyethylene tibial insert attached to a metal tibial baseplate.The composition of metal and plastic raises concerns of polyethylene wear,in vivo oxidation,and metal hypersensitivity.
To address these issues,biomedical engineers are exploring implant geometry and implant materials for more natural feeling prosthetic knee while extending implant longevity.For implant geometry,orthopedics are focusing on femoral implant radii,tibial baseplate symmetry,the tibial articular surface,and restoration of the anterior cruciate ligament function.For implant materials,biomedical engineers are experimenting with ceramics,polyether ether ketone,crosslinked polyethylene,and antioxidant stabilized polyethylene.
One example is the development of Biomimetic total knee implant[34-35].To restore normal knee kinematics,orthopedics have recently designed the bicruciate retaining biomimetic total knee implant compatible with normal soft tissue envelopment and normal knee kinematics by reverse engineering a biomimetic articular surface with the in vivo kinematics of healthy knees(Fig.8)[34-35].An analysis of the biomimetic implant and other contemporary cruciate retaining designs by the LifeModeler KneeSIM software in simulations of normal knee activities suggest that ACL preservationand biomimetic implants could closely restore normal knee function,but further long-term clinical trials are necessary to determine the value of biomimetic designs[36-38].

Fig.7 The low contact stress mobile bearing total knee prosthesis(From DePuy Synthes)

Fig.8 Components of the biomimetic bicruciate implant(From Li,G.,et al.[34])
References
[1]Maradit Kremers H,Larson DR,Crowson CS,et al.Prevalence of total hip and knee replacement in the united states.J Bone Joint Surg Am,2015,97(17):1386-1397.
[2]Kurtz S,Ong K,Lau E,et al.Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030.J Bone Joint Surg Am,2007,89(4):780-785.
[3]Losina E,Katz JN.Total knee arthroplasty on the rise in younger patients: Are we sure that past performance will guarantee future success? Arthritis Rheum,2012,64(2): 339-341.
[4]Callaghan,JJ.The Adult Knee.2003: Lippincott Williams & Wilkins.
[5]Murphy JB,I.Arthroplasty.Ann Surg,1913,57(5):593-647.
[6]Campbell WC.Arthroplasty of the knee-report of cases.J Bone Joint Surg,1921,3(9):430-434.
[7]Baer WS.Arthroplasty with the aid of animal membrane.J Bone Joint Surg,1918,16(3):171-199.
[8]Omori.A Case Report of Arthroscopic and Histological Long-Term Evaluation after Resection Interposition Knee Arthroplasty with Chromicized Autogenous Fascia Lata(JK Membrane).1996.
[9]Friedman MJ.UniSpacer.Arthroscopy,2003,19(Suppl1): S120-121.
[10]Bailie AG,Lewis PL,Brumby SA,et al.The Unispacer knee implant: early clinical results.J Bone Joint Surg,2008,90(4):446-450.
[11]Sisto DJ,Mitchell IL.UniSpacer arthroplasty of the knee.J Bone Joint Surg Am,2005,87(8):1706-1711.
[12]Eynon-Lewis NJ,Ferry D,Pearse MF,et al.Themistocles Gluck: an unrecognised genius.BMJ,1992.19-26,305(6868):1534-1536.
[13]Walldius B.Arthroplasty of the knee joint employing an acrylic prosthesis.Acta Orthop Scand,1953,23(2):121-131.
[14]Mazas FB.Guepar total knee prosthesis.Clin Orthop Relat Res,1973,(94):211-221.
[15]Manning DW,Chiang,Freiberg,et al.Hinge Implants in Revision Total Knee Arthroplasty,JVBono and RD Scott2005,Springer New York 219-236.
[16]Matthews LS.Spherocentric Knee Arthroplasty: Development and Clinical Experience.Lowa Orthop J,1981(1):28-31.
[17]Gunston FH.Polycentric knee arthroplasty.Prosthetic simulation of normal knee movement.J Bone Joint Surg Br,1971,53(2):272-277.
[18]Gunston FH,MacKenzie RI.Complications of polycentric knee arthroplasty.Clin Orthop Relat Res,1976,(120):11-17.
[19]Ranawat CS,Shine JJ.Duo-condylar total knee arthroplasty.Clin Orthop Relat Res,1973,(94):185-195.
[20]Ranawat CS,Insall J,Shine J,et al.Duo-condylar knee arthroplasty: hospital for special surgery design.Clinl Orthop Relat Res,1976,(120):76-82.
[21]Coventry MB,Finerman GA,Riley LH,et al.A new geometric knee for total knee arthroplasty.Clin Orthop Relat Res,1972,83:157-162.
[22]Rand JA,Coventry MB.Ten-year evaluation of geometric total knee arthroplasty.Clin Orthop Relat Res,1988,(232):168-173.[23]Townley CO.The anatomic total knee resurfacing arthroplasty.Clin Orthop Relat Res,1985,(192):82-96.
[24]Insall J,Ranawat CS,Scott WN,et al.Total condylar knee replacment: preliminary report.Clin Orthop Relat Res,1976,(120):149-154.
[25]Kolisek FR,McGrath MS,Marker DR,et al.Posteriorstabilized versus posterior cruciate ligament-retaining total knee arthroplasty.Iowa Orthop J,2009,29:23-27.
[26]Goodfellow JW,O’Connor J.Clinical results of the Oxford knee.Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis.Clin Orthop Relat Res,1986,(205):21-42.
[27]Buechel FF,Pappas MJ.The New Jersey Low-Contact-Stress Knee Replacement System: biomechanical rationale and review of the first123 cemented cases.Arch Orthop Trauma Surg,1986,105(4):197-204.
[28]Huang CH,Liau JJ,Cheng CK.Fixed or mobile-bearing total knee arthroplasty.J Orthop Surg,2007,(2):1.
[29]Aprato A,Risitano S,Sabatini L,et al.Cementless total knee arthroplasty.Ann Transl Med,2016,4(7):129.
[30]Matassi F,Carulli C,Civinini R,et al.Cemented versus cementless fixation in total knee arthroplasty.Joints,2014,1(3):121-125.
[31]Sharkey PF,Lichstein PM,Shen C,et al.Why are total knee arthroplasties failing today - has anything changed after10 years? J Arthroplasty,2014,29(9):1774-1778.
[32]Thiele K,Perka C,Matziolis G,et al.Current failure mechanisms after knee arthroplasty have changed: polyethylenewear is less common in revision surgery.J Bone Joint Surg Am,2015,97(9):715-720.
[33]Bourne RB,Chesworth BM,Davis AM,et al.Patient Satisfaction after Total Knee Arthroplasty: Who is Satisfied and Who is Not? Clin Orthop Relat Res,2010,468(1):57-63.
[34]Li G,Rubash HE,Varadarajan KM.Implant for restoring normal range flexion and kinematics of the knee.2014,Google Patents.
[35]Varadarajan KM,Zumbrunn T,Rubash HE,et al.Reverse engineering nature to design biomimetic total knee implants.J Knee Surg,2015,28(5):363-369.
[36]Zumbrunn T,Varadarajan KM,Rubash HE,et al.Regaining native knee kinematics following joint arthroplasty: a novel biomimetic design with ACL and PCL preservation.J Arthroplasty,2015,30:2143-2148.
[37]Varadarajan KM,Zumbrunn T,Rubash HE,et al.Cruciate retaining implant with biomimetic articular surface to reproduce activity dependent kinematics of the normal knee.J Arthroplasty,2015,30:2149-2153.
[38]Zumbrunn T,Varadarajan KM,Rubash HE,et al.Biomimetic total knee arthroplasty with anterior cruciate ligament(ACL)preservation restores normal kinematics.Orthop Proceedings,2013,95-B(SUPP 34):603-603.
(本文编辑:李贵存)
10.3969/j.issn.2095-252X.2016.10.010
R687.4
关节成形术,置换,膝;人工膝关节;膝关节;关节成形术,置换;全膝关节置换术delayed wound healing,and sinus formation[7-8].The concept of interposition arthroplasty was revisited in the early 2000s by Center Pulse Orthopedics in their UniSpacer knee design,similar to the early metallic interposition arthroplasty designs of MacIntosh and McKeever[9].Advantages offered by the UniSpacer knee include no bone resection or bone fixation as well as ease of revision[9-10].However,clinical results indicated a high rate of revision surgery as a result of pain,swelling,instability,dislocation,and medial erosion[10-11].
(2016-08-16)
Guoan Li,Email: Gli1@mgh.harvard.edu