胱抑素C和炎症因子在脓毒症致急性肾损伤儿童中的临床价值
2016-09-20赵慧,陈苓
赵 慧,陈 苓
(湖北省妇幼保健院急诊科,湖北 武汉 430070)
胱抑素C和炎症因子在脓毒症致急性肾损伤儿童中的临床价值
赵慧,陈苓
(湖北省妇幼保健院急诊科,湖北 武汉 430070)
目的检测脓毒症致急性肾损伤儿童胱抑素C和炎症因子,并探究其临床意义。方法选择2012年1月至2015年12月在湖北省妇幼保健院诊治的脓毒症致急性肾损伤儿童30例为研究对象(SAKI组),另选择同期诊断为单纯脓毒症(SEP组)和门诊健康体检的正常健康儿童(CON组)各30例为对照。检测三组研究对象的肾功能、胱抑素C和炎症因子,并对检测结果进行比较,对胱抑素C、炎症因子与急性生理学及慢性健康状况评价(APACHEⅡ)的相关性进行分析。结果SEP组儿童的肌酐(Scr)、尿素氮(BUN)和胱抑素C与CON组儿童比较差异均无统计学意义(均P>0.05),肿瘤坏死因子(TNF)-α和白细胞介素(IL)-6均显著高于CON组儿童(t值分别为25.999、11.966,均P<0.05),而IL-10则显著低于CON组儿童(t=7.295,P<0.05)。SAKI组儿童Scr、BUN、胱抑素C、TNF-α和IL-6均显著高于SEP组和CON组(t值分别为3.300~100.390、3.200~99.800,均P<0.05),而IL-10均显著低于SEP组和CON组(t值分别为25.987、18.692,均P<0.05)。经相关性分析表明,SAKI组儿童的胱抑素C、TNF-α和IL-6与APACHEⅡ评分均呈正相关(rs值分别为0.422、0.369、0.417,均P<0.05),IL-10与APACHEⅡ评分呈负相关(rs=-0.381,P<0.05);SEP组儿童TNF-α和IL-6与APACHEⅡ评分均呈正相关(rs值分别为0.314、0.372,均P<0.05),IL-10与APACHEⅡ评分呈负相关(rs=-0.319,P<0.05)。结论胱抑素C和炎症因子在脓毒症致急性肾损伤儿童中显著升高,与病情严重程度紧密相关,可作为其病情及预后评估的标志物。
脓毒症;急性肾损伤;胱抑素C;炎症因子
[Abstract]Objective To study the clinical significance of cystatin C and inflammatory factors in children with sepsis induced acute kidney injury (SAKI). Methods From January 2012 to December 2015 totally 30 children with SAKI were diagnosed and treated in Hubei Provincial Hospital of Health, and they were selected in research subjects (SAKI group). Another 30 cases of simple sepsis (SEP group) and 30 healthy children (CON group) were selected as controls. Renal function, cystatin C and inflammatory factors were detected and compared among three groups. The correlation between serum cystatin C and inflammatory factors with APACHE II score was analyzed. Results The Scr, BUN and cystatin C were not significantly different between SEP group and CON group (allP>0.05), but TNF-α and IL-6 in SEP group were significantly higher than in CON group(tvalue was 25.999 and 11.966, respectively, bothP<0.05)while IL-10 was remarkably lower (t=7.295,P<0.05). In SAKI group Scr, BUN, cystatin C, TNF-α and IL-6 were significantly higher than those in SEP group and CON group (tvalue ranged 3.300-100.390 and 3.200-99.800, respectively, allP<0.05), but IL-10 was remarkably lower (tvalue was 25.987 and 18.692, respectively, bothP<0.05). Correlation analysis showed that in SAKI group cystatin C, TNF-α and IL-6 were positively correlated with APACHE II score (rsvalue was 0.422, 0.369 and 0.417, respectively, allP<0.05) but IL-10 was negatively correlated with APACHEⅡscore (rs=-0.381,P<0.05). In SEP group, TNF-α and IL-6 were positively correlated with APACHEⅡ score (rsvalue was 0.314 and 0.372, respectively, bothP<0.05) but IL-10 was negatively correlated with APACHEⅡscore (rs=-0.319,P<0.05). Conclusion The cystatin C and inflammatory factors in children with sepsis induced acute kidney injury are significantly higher than healthy children, which are closely related with severity of the disease and could act as biomarker for its condition and prognosis evaluation.
[Key words]sepsis;acute kidney injury;cystatin C; inflammatory factor
脓毒症并发急性肾损伤时死亡率高达67.3%,是儿童发生脓毒症后最常见的死亡原因,故寻找反映脓毒症致急性肾损伤病情及预后的标志物对改善其预后具有重要意义[1-2]。业已证实炎症因子可作为脓毒症病情及预后评估的标志物[3],胱抑素C与急性肾损伤病情及预后密切相关[4],推测与成人类似,胱抑素C及炎症因子在儿童脓毒症致急性肾损伤病情及预后中具有重要作用。本研究通过检测脓毒症致急性肾损伤儿童胱抑素C和炎症因子水平,探究其在儿童脓毒症致急性肾损伤中的临床价值。
1资料与方法
1.1临床资料
选择2012年1月至2015年12月在湖北省妇幼保健院诊治的脓毒症致急性肾损伤患儿30例为研究对象(SAKI组),纳入标准:①经血细菌培养及影像学检查确诊为脓毒症,脓毒症诊断参考2001年国际脓毒症定义会议标准;②经肾功能检测诊断为脓毒症致继发性急性肾损伤,符合2005年急性肾损伤网络制定的急性肾损伤诊断标准;③排除既往肾脏病史、其它病因导致的急性肾损伤或合并心脑肺血管疾病。另选择同期诊断为单纯脓毒症(SEP组)和门诊健康体检的正常健康儿童(CON组)各30例为对照。该研究均征的儿童监护人知情同意,并经医院伦理委员会通过。3组研究对象的年龄均在3~15岁,体重均为12~40kg。SAKI组、SEP组和CON组研究对象在性别、年龄和体质量指数方面差异均无统计学意义(均P>0.05),见表1。
表1 各组研究对象一般资料的比较结果
1.2研究指标及检测方法
所有研究对象于空腹8h后取静脉血5mL检测以下指标:①肾功能采用血清肌酐(Scr)和血清尿素氮(BUN)评估,采用全自动生化仪检测;②病情严重程度:采用急性生理学及慢性健康状况评价(APACHEⅡ);③胱抑素C采用胶乳增强型免疫比浊法检测;④炎症因子包括肿瘤坏死因子(TNF)-α、白细胞介素(IL)-6和IL-10,检测方法均为酶联免疫吸附法。
1.3统计学方法
采用Sigmaplot 11.5进行统计学分析。SAKI组、SEP组和CON组间肾功能、胱抑素C和炎症因子比较采用SNK法分别比较;计数资料采用χ2检验。采用Spearman相关分析胱抑素C和炎症因子与APACHEⅡ评分的相关性。以P<0.05认为差异具有统计学意义。
2结果
2.1各组的研究指标检测情况
SAKI组脓毒症致急性肾损伤儿童Scr、BUN、胱抑素C、TNF-α和IL-6均显著高于SEP组和CON组(均P<0.05),而IL-10均显著低于SEP组和CON组(均P<0.05);SEP组脓毒症儿童Scr、BUN和胱抑素C与CON组正常健康儿童比较差异均无统计学意义(均P>0.05),TNF-α和IL-6均显著高于CON组正常健康儿童(均P<0.05),而IL-10显著低于CON组正常健康儿童(P<0.05),见表2。

表2 各组的肾功能、胱抑素C和炎症因子的比较结果±S)
注:t1和t2分别为SAKI组与SEP组、CON组的比较值,均P<0.05;t3为SEP组与CON组的比较值。
2.2胱抑素C和炎症因子与急性生理学及慢性健康状况评价评分的相关性
将SAKI组和SEP组患儿的胱抑素C和炎症因子分别与APACHEⅡ评分行相关性分析,SAKI组脓毒症致急性肾损伤儿童胱抑素C、TNF-α和IL-6与APACHEⅡ评分均呈正相关(均P<0.05),IL-10与APACHEⅡ评分呈负相关(P<0.05);SEP组脓毒症儿童胱抑素C与APACHEⅡ评分无明显相关(P>0.05),TNF-α和IL-6与APACHEⅡ评分均呈正相关(均P<0.05),IL-10与APACHEⅡ评分呈负相关(P<0.05),见表3。
表3SAKI组和SEP组患儿胱抑素C和炎症因子与APACHEⅡ评分的相关性
Table 3Correlation of serum cystatin C and inflammatory factors with APACHEⅡ score in SAKI group and SEP group
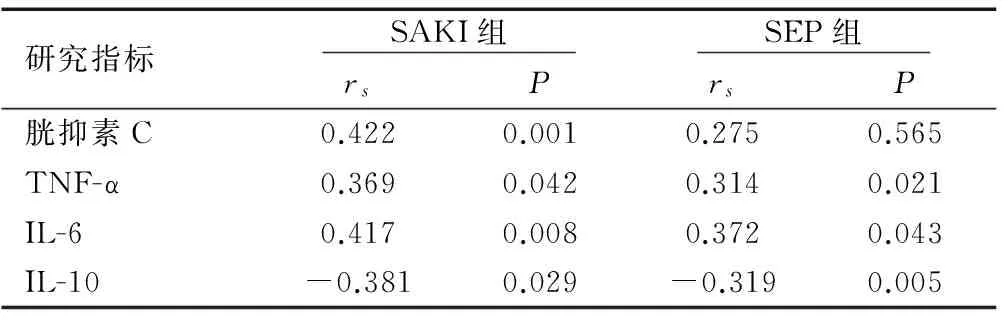
研究指标 SAKI组 SEP组 rsPrsP胱抑素C0.4220.0010.2750.565TNF-α0.3690.0420.3140.021IL-60.4170.0080.3720.043IL-10-0.3810.029-0.3190.005
3讨论
3.1脓毒症与胱抑素C和炎症因子关系
脓毒症时炎症细胞激活后可分泌TNF和IL等炎症因子,引起系统性全身炎症反应,诱导肾小管上皮合成补体导致系统性全身炎症反应,IL和血管舒张-收缩等炎症因子可促进肾小球分泌炎性介质,造成肾小球损伤,同时导致肾小球血管舒张功能异常,此外包括内皮素等炎症因子可收缩肾血管,降低肾小球血流量,使肾小球滤过率显著降低,最终导致急性肾损伤,其为脓毒症最常见的死亡原因[5-6]。脓毒症炎症反应导致促进炎症因子TNF-α和IL-6显著升高,而抑制炎症因子IL-10显著降低,TNF-α、IL-6和IL-10可作为脓毒症病情严重程度及预后的标志物,同时可作为抗生素治疗效果的评价标准[7-8]。胱抑素C作为一种半胱氨酸蛋白酶抑制剂,机体有核细胞均可产生且仅通过肾脏排泄,且产生速率不受外界因素影响,机体胱抑素C仅由肾小球滤过而被清除,但重吸收后被完全代谢分解而不返回血液,故胱抑素C在血液中的浓度仅由肾小球滤过决定[9]。胱抑素C不受性别、年龄及饮食等外在因素影响,是目前最理想的反映肾小球滤过率变化的标志物,在肾脏早期病变时即可检测到其改变,较传统的肾功能标志物具有更高的准确度及灵敏性[10]。基于这些证据,推测胱抑素C及炎症因子在儿童脓毒症致急性肾损伤病情及预后评估中具有重要意义。
3.2胱抑素C和炎症因子在儿童脓毒症致急性肾损伤中的评估作用
目前的研究已经证实TNF-α、IL-6和IL-10在脓毒症病情及预后评估中的价值,但这些均为对成人的研究或其他原因导致的急性肾损伤,而成人与儿童可能存在免疫及机体对重症炎症反应的显著差异,可能TNF-α、IL-6和IL-10在儿童脓毒症致急性肾损伤中的价值与成人不同。本研究中,SEP组脓毒症儿童的Scr、BUN和胱抑素C与CON组正常健康儿童均无明显差异(均P>0.05),TNF-α和IL-6均显著高于CON组正常健康儿童(均P<0.05),而IL-10显著低于CON组正常健康儿童(P<0.05);SAKI组脓毒症致急性肾损伤儿童的Scr、BUN、胱抑素C、TNF-α和IL-6均显著高于SEP组和CON组(均P<0.05),而IL-10均显著低于SEP组和CON组(均P<0.05)。这些证据表明脓毒症导致急性肾损伤时,炎症因子水平较单纯脓毒症存在明显改变,而胱抑素C仅在脓毒症并发急性肾损伤时发生改变,单纯脓毒症不存在胱抑素C的改变。基于胱抑素C与肾功能的关系,可能在儿童脓毒症致急性肾损伤中对并发肾损伤时具有预测价值,同时可用于评估其病情。根据目前证实的胱抑素C在肾损伤中的价值,推测儿童脓毒症致急性肾损伤中动态监测胱抑素C可评估其治疗疗效并可做相应调整。
目前评价重症患者最常见的指标为APACHEⅡ评分,与病情程度及预后密切相关。本研究将SAKI组和SEP组患儿的胱抑素C和炎症因子分别与APACHEⅡ评分行相关性分析,SAKI组脓毒症致急性肾损伤儿童胱抑素C、TNF-α和IL-6与APACHEⅡ评分均呈正相关(均rs>0,均P<0.05),IL-10与APACHEⅡ评分呈负相关(均rs<0,P<0.05);SEP组脓毒症儿童胱抑素C与APACHEⅡ评分无明显相关(P>0.05),TNF-α和IL-6与APACHEⅡ评分均呈正相关(均rs>0,均P<0.05),IL-10与APACHEⅡ评分呈负相关(均rs<0,P<0.05)。这些证据表明胱抑素C和炎症因子与脓毒症致急性肾损伤病情严重程度紧密相关,可作为其病情及预后评估的标志物。但本研究病例数较少,该结论有待于进一步研究证实。
[1]Kim M, Brady J E, Li G.Interaction effects of acute kidney injury, acute respiratory failure, and sepsis on 30-day postoperative mortality in patients undergoing high-risk intraabdominal general surgical procedures[J].Anesth Analg,2015,121(6):1536-1546.
[2]Nagata I, Uchino S, Tokuhira N,etal.Sepsis may not be a risk factor for mortality in patients with acute kidney injury treated with continuous renal replacement therapy[J].J Crit Care,2015,30(5):998-1002.
[3]白海涛,陈美雪.儿童脓毒症急性肾损伤与液体管理[J].中华实用儿科临床杂志,2015,30(5):328-330.
[4]Keir I, Kellum J A.Acute kidney injury in severe sepsis: pathophysiology, diagnosis, and treatment recommendations[J].J Vet Emerg Crit Care(San Antonio),2015,25(2):200-209.
[5]Heung M, Koyner J L.Entanglement of sepsis, chronic kidney disease, and other comorbidities in patients who develop acute kidney injury[J].Semin Nephrol,2015,35(1):23-37.
[6]Dai X, Zeng Z, Fu C,etal.Diagnostic value of neutrophil gelatinase-associated lipocalin, cystatin C, and soluble triggering receptor expressed on myeloid cells-1 in critically ill patients with sepsis-associated acute kidney injury[J].Critical care,2015,19:223.
[7]de Oliveira F S, Freitas F G, Ferreira E M,etal.Positive fluid balance as a prognostic factor for mortality and acute kidney injury in severe sepsis and septic shock[J].J Crit Care,2015,30(1):97-101.
[8]陈凯.严重烧伤脓毒症患者血清TNF-α、IL-6、IL-10、PLA2的变化及器官功能损害状况分析[J].重庆医学,2014,43(8):937-940.
[9]马宏星,陈淑珍,陈雪民.基于血清胱抑素C的肾功能估算公式在肾功能评价中的价值[J].中华核医学与分子影像杂志,2014,34(3):204-207.
[10]邓瑛,郭红霞,俞泓,等.血清胱抑素C在评估早期肾功能损害中的价值[J].实用妇产科杂志,2014,30(5):377-379.
[专业责任编辑:黄燕萍]
Clinical significance of cystatin C and inflammatory factors in children with sepsis induced acute kidney injury
ZHAO Hui, CHEN Ling
(Department of Emergency, Hubei Provincial Hospital of Health, Hubei Wuhan 430070, China)
2016-03-28
赵慧(1969-),女,副主任医师,主要从事儿科急诊工作。
10.3969/j.issn.1673-5293.2016.08.020
R725
A
1673-5293(2016)08-0965-03
