血浆D二聚体水平在预测子前期发病中的价值
2016-07-10侯燕燕
周 晔, 顾 玮, 林 婧, 侯燕燕
(上海交通大学医学院附属国际和平妇幼保健院产科,上海 200030)
·临床研究·

周 晔, 顾 玮, 林 婧, 侯燕燕
(上海交通大学医学院附属国际和平妇幼保健院产科,上海 200030)
目的 探讨血浆D二聚体在预测子前期发病中的的价值。方法 收集2013年6月至2014年12月间建卡产检并分娩的孕产妇资料共计13285例,所有孕妇均定期产检,随访至产后3个月并收集相关资料。其中有10623例为无妊娠合并症的正常孕产妇,作为正常对照组;有577例诊断为妊娠期高血压,作为妊娠期高血压组。291例为子前期患者,作为子前期组对象,其中214例为轻度子前期,77例为重度子前期。所有研究对象在孕32周~34周间进行血浆D-二聚体的检测,分析D-二聚体在预测子前期发病中的作用及其与不良妊娠结局的关系。结果 经T检验表明,子前期组的D-二聚体水平高于妊娠期高血压组,而妊娠期高血压组高于对照组(P<0.01)。但在轻、重度子前期组间D-二聚体的表达差异无统计学意义(P=0.728)。通过Pearson双变量相关法研究D-二聚体水平与各妊娠结局间的关系,结果表明D-二聚体水平越高,产后出血量越大,早产和难产率也越高,而新生儿Apgar评分和出生体质量均越低。应用Logistics回归方程证实了孕晚期D-二聚体水平的升高可预测子前期的发病。并应用ROC曲线计算得出D-二聚体的预测界值为0.995mg/L时,其预测敏感度为95.8%,相对危险度为7.35。结论 D-二聚体可作为预测子前期发病的实验室指标,且其与各种不良妊娠结局均有相关性,D-二聚体预测子前期发病的界值为0.995mg/L,其预测敏感度为95.8%,相对危险度为7.35。
子前期; D-二聚体; 妊娠结局

1 资料与方法
1.1 一般资料

1.2 研究方法
所有研究对象在孕32~34周间于前臂抽取静脉血3ml检测D-二聚体,抗凝剂采用枸橼酸钠,离心半径18cm,3000r/min,对血标本进行离心5min,然后按照本院标准作业程序检测血浆中的D-二聚体水平,所有试剂均为配套试剂,所有标本均在采血后2h内完成。
表1 各组研究对象的一般情况


组别n年龄/岁孕次/次产次/次分娩孕周/周出生体质量/g对照组1062329.7±2.91.5±0.81.1±1.038.2±1.53401.7±2051.3妊娠期高血压组57729.5±2.71.5±0.81.0±0.437.9±3.83326.4±490.1子前期组29130.2±3.01.4±0.81.0±0.337.3±3.43216.7±542.0轻度子前期21430.1±3.31.4±0.81.0±0.337.3±5.63299.4±493.7重度子前期7730.3±3.71.4±0.81.0±0.237.4±1.92987.0±622.5
1.3 统计学处理
2. 结 果
2.1 各组研究对象的D-二聚体水平


表2 各组研究对象的D-二聚体水平
2.2 D-二聚体水平与各妊娠结局间的关系
通过Pearson双变量相关法研究D-二聚体水平与各妊娠结局间的关系,结果表明,D-二聚体与产后出血量呈正相关,即D-二聚体水平越高,产后出血量越大;而D-二聚体与新生儿Apgar评分,新生儿体质量及孕周均呈负相关,即D-二聚体水平越高,新生儿Apgar评分越低,新生儿体质量越低,且孕周越小,差异有统计学意义。另外,D-二聚体水平与分娩方式也有关,D-二聚体水平越高,难产(剖宫产及产钳)率也越高,见表3。

表3 D-二聚体与各妊娠结局的相关性

表4 子前期各影响因素的Logistics回归分析
Tab.4 Logistic regression for the influence factors
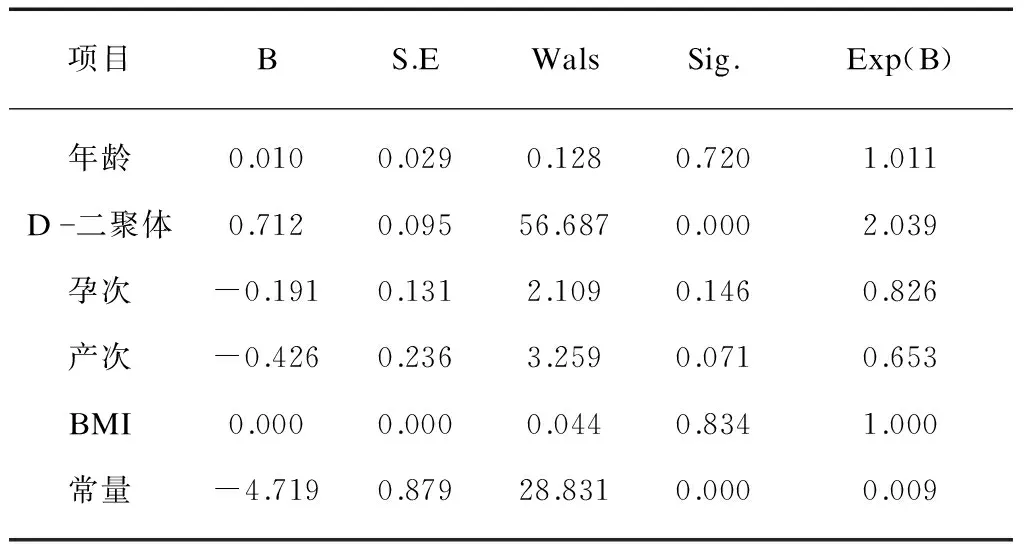
表4 子前期各影响因素的Logistics回归分析
项目BS.EWalsSig.Exp(B)年龄0.0100.0290.1280.7201.011D二聚体0.7120.09556.6870.0002.039孕次-0.1910.1312.1090.1460.826产次-0.4260.2363.2590.0710.653BMI0.0000.0000.0440.8341.000常量-4.7190.87928.8310.0000.009

表5 ROC曲线下的面积

图1 ROC曲线分析血浆D-二聚体水平在子前期预测中的价值Fig.1 The value of plasma D-dimer levels in predicting preeclampsia
3 讨 论
3.1 正常妊娠时D-二聚体的表达
D-二聚体是在血液凝固及纤溶系统中,纤维蛋白单体经活化因子交联后,再经纤溶水解所产生的一种特异性降解产物,可作为高凝状态和纤溶亢进的分子标志物。正常非孕期时人体内的凝血、抗凝以及纤溶系统处于一个相互作用相互制约的动态平衡状态。妊娠时,体内的凝血因子Ⅱ、Ⅴ、Ⅶ、Ⅷ等水平均有所增加,使孕妇的血液处于高凝状态,有利于产后快速有效止血及子宫内膜的再生和修复。这种生理性的妊娠期高凝状态是机体一种保护措施。但是这种血液的高凝状态过度时会引起血管内凝血,形成血栓,使得继发性纤溶活动增强,以清除血栓。孕妇血液中D-二聚体的水平明显升高,反映体内高凝和继发性纤溶亢进的状态[8],对诊断血栓性疾病也有重要意义[9]。
高凝状态下血栓形成,会导致胎盘缺血缺氧,坏死的微小绒毛途经肺循环时释放出大量的组织凝血活酶,引起血管内凝血的发生,并激活纤溶系统来清除子宫螺旋动静脉内的血栓。许多研究证明D-二聚体随妊娠进展将逐步增加[10]。Kovac等[11]和Hansen等[12]研究分别发现D-二聚体在妊娠早期、中期和晚期各超出孕前16%~31%、67%~76%及98%以上。最近Reger等[10]在正常妊娠第16、26、36周3个时间点分别测量D-二聚体水平,发现高于非妊娠期的42%、66%、98%。正常妊娠妇女的生理性高凝状态自孕3个月开始,且随着妊娠日渐显著,母体D-二聚体水平也在妊娠期升高明显[13]。
3.2 D-二聚体水平与妊娠结局的相关性
从血液流变学方面观察,妊娠期血液处于高凝状态,浓缩的血液使孕妇的血液黏稠度增高,外周循环阻力增加,令胎盘灌注减少,致使各重要脏器灌注不足,发生胎儿缺血缺氧,可出现FGR、死胎、羊水过少、早产、胎儿宫内窘迫及新生儿窒息等并发症。近年来,在许多关于不良妊娠结局的研究中,普遍认为“血栓前状态”是一个高危因素。研究表明,发生反复流产、胎儿生长受限、胎盘早剥甚至死胎等的妇女,其血栓形成倾向发生率高达65%[14]。
D-二聚体是标志继发性纤溶亢进的物质,比APTT,PT等指标发生异常的时间更早,可在早期判断凝血功能异常。当孕妇体内存在异常增高的凝血活性,会在凝血的同时激发继发性纤溶活动,使D-二聚体水平显著增加[15]。有学者认为临床上检测血浆D-二聚体水平对预测围产儿预后有一定价值,实验表明孕晚期孕妇血浆D-二聚体浓度升高和产后出血的发生有一定的相关性,若孕妇临产后血浆D-二聚体水平位于临界高值,其产后出血率明显上升[16-17]。血液高凝状态可诱发静脉血栓生成,导致反复流产、胎儿宫内缺氧、胎儿生长受限及早产等[18]不良结局。本研究结果也表明,D-二聚体的水平与各妊娠结局均有相关性,当D-二聚体异常升高时,发生产后出血、早产、胎儿窘迫、FGR及难产的概率均会增加。故临床上若发现D-二聚体水平异常升高,需及时采取干预措施,从而改善母儿预后,保护母婴的健康。

[1] George EM, Granger JP. Mechanisms and potential therapies for preeclampsia[J]. Curr Hypertens Rep, 2011,13(4): 269-275.
[2] Dusse LM, Rios DR, Pinheiro MB, et al. Pre-eclampsia: relationship between coagulation, fibrinol-ysis and inflammation[J]. Clin Chim Acta, 2011,412(1-2): 17-21.
[3] Joly B, Barbay V, Borg JY, et al. Comparison of markers of coagulation activation and thrombin generation test in uncomplicated pregnancies[J]. Thromb Res, 2013,132(3): 386-391.
[4] Szecsi PB, Jorgensen M, Klajnbard A, et al. Haemostaticreference intervals in pregnancy[J]. Thromb Haemost,2010,103(4): 718-727.
[7] Pinheiro Mde B, Junqueira DR, Coelho FF, et al. D-dimer in preeclampsia: systematic review and meta-analysis[J].Clin Chim Acta,2012,414: 166-170.
[8] 黄中海.正常孕妇不同孕期及产后3天D-二聚体和凝血指标的变化及意义[J].蚌埠医学院学报,2011,36(4): 407-409.
[9] 彭海云.D-二聚体在孕妇检测中的临床意义[J].现代中西医结合杂志,2011,20(22): 2826-2827.
[10] Reger B, Peterfalvi A, Litter I, et al. Challenges in the evaluation of D-dimer and fibrinogen levels in pregnant women[J]. Thromb Res, 2013,131(4): e183-e187.
[11] Kovac M, Mikovic Z, Rakicevic L, et al. The use of D-dimer with new cutoff can be useful in diagnosis of venous thromboembolism in pregnancy[J]. Eur J Obstet Gynecol Reprod Biol, 2010,148(1): 27-30.
[12] Hansen AT, Andreasen BH, Salvig JD, et al. Changes infibrin D-dimer, fibrinogen, and protein S during pregnancy[J]. Scand J Clin Lab Invest, 2011,71(2): 173-176.
[13] Maiello M, Torella M, Caserta L, et al. Hypercoagulability during pregn-ancy; evidences for a thrombophilic state[J]. Minerva Ginecol, 2006,58(5): 417-422.
[14] 赵智慧,柳志红.血栓形成倾向与妊娠静脉血栓栓塞症的治疗[J].中国分子心脏病学杂志,2003,3(1): 46-49.
[15] Morikawa M, Yamada T, Yamada T, et al. Changes in D dimer levels after cesarean section in women with singleton and twin pregnancies[J]. Thromb Res, 2011,128(4): e33-e38.
[16] 杜建钢.临产孕妇血浆D-二聚体纤维蛋白原及抗凝血酶Ⅲ检测的临产意义[J].检验医学与临床,2011.8(21): 2616-2617.
[17] Bates SM. D-dimer assays in diagnosis and manage-ment of thrombotic and bleeding disorders[J]. Semin Thromb Hemost, 2012,38(7): 673-682.
[18] 丁虹,朱付凡.妊娠期血液高凝状态与产科并发症[J].中华妇产科杂志,2003,38(10): 643-646.
[19] Anderson UD, Olsson MG, Kristensen KH, et al. Review: Biochemical markers to predict preeclampsia[J]. Placenta, 2012,33(Suppl): 42-47.
[20] Boij R, Svensson J, Nilsson-ekdahl K, et al. Biomarkers of coagulation,inflammation, and angioge-nesis are independently associated with preeclampsia[J]. Am J Reprod Immunol, 2012,68(3): 258-270.
[21] Zhang Y, Hu Y, Guo T, et al. Thrombinactivatable fibrinolysis inhibitor in preeclampsia and gestational hypertension throughout the gestation[J]. J Huazhong Univ Sci Technolog Med Sci, 2008,28(2): p.140- 143.
[22] Pinheiro MB, Junqueira DR, Coelho FF, et al. D-dimer inpreeclampsia: systematic review and meta-analysis[J]. Clin Chim Acta, 2012,414: 166-170.
Value of plasma D-dimer levels in predicting preeclampsia
ZHOUYe,GUWei,LINJing,HOUYan-yan
(Dept. of Obstetrics, International Peace Maternity and Child Health Hospital Affiliated to Shanghai Jiaotong University School of Medicine, Shanghai 200030, China)
Objective To evaluate the detection of plasma D-dimer in predicting preeclampsia. Methods Total of 13285 pregnant women undergoing regular antenatal examination and delivery between June 2013 and December 2014 were enrolled in the study. All pregnant women were followed up for 3 months postpartumly and the related information was collected. There were 10623 cases without pregnancy complications(control group), 577 cases with pregnancy induced hypertension(gestational hypertension group) and 291 cases with preeclampsia, including 214 mild cases and 77 severe cases. Plasma D-dimer levels were measured in all subjects, and the association of D-dimer with preeclampsia and adverse pregnancy outcomes was analyzed. Results Plasma D-dimer levels in preeclampsia group were higher than those in control group and gestational hypertension group(P<0.01); however, there was no significant difference(P=0.728) between the mild and severe preeclampsia group. Pearson bivariate correlation showed that D-dimer levels were positively correlated with incidence of postpartum hemorrhage, premature birth and difficult delivery, and negatively correlated with Apgar score and birth weight. Logistic regression equation showed that the increase of D-dimer level was associated with the onset of preeclampsia. The ROC curves showed the predicted cut-off value of D-dimer was 0.995mg/L, the sensitivity was 95.8% and the relative risk was 7.35. Conclusion D-dimer can be used as a laboratory index to predict the onset of preeclampsia, and it is correlated with adverse pregnant outcomes.
preeclampsia; D-dimer; pregnancy outcomes
10.16118/j.1008-0392.2016.02.020
2015-11-17
周 晔(1966—),女,副主任医师,硕士.E-mail: victoriazhou66@163.com
顾 玮.E-mail: krisgu@163.com
R 714.24+5
A
1008-0392(2016)02-0087-05
