腹部计算机断层扫描提示大肠肠壁增厚的临床意义
2016-06-01吴群英李建英
吴群英,李建英
福建医科大学附属协和医院消化内科,福建 福州 350009
腹部计算机断层扫描提示大肠肠壁增厚的临床意义
吴群英,李建英
福建医科大学附属协和医院消化内科,福建 福州 350009
目的 研究腹部计算机断层CT提示大肠肠壁增厚患者的临床资料,探讨腹部CT提示大肠肠壁增厚的临床意义。方法 回顾性分析2008年3月-2014年3月在福建医科大学附属协和医院行腹部CT检查提示大肠肠壁增厚的136例患者资料,所有患者在随后的1个月内均行肠镜检查且资料完整。结果 35例腹部CT提示大肠肠壁增厚并行肠镜检查提示为正常的患者中,肠壁增厚多位于右半结肠,与异常组比较差异有统计学意义(P<0.001)。41例肠道恶性肿瘤患者中,病变部位多位于左半结肠(P=0.006)。与良性疾病相比,便血、淋巴结肿大多见于恶性肿瘤(P<0.05)。与非炎症性疾病相比,腹痛在炎症性疾病中差异有统计学意义(P<0.001)。且CT提示为弥漫性肠壁增厚,多见于炎症性疾病(P<0.001)。结论 腹部CT提示右半结肠壁增厚,多见于正常者;而左半结肠壁增厚,多见于恶性肿瘤者;弥漫性肠壁增厚,多见于结肠炎症性疾病患者。如腹部CT提示肠壁增厚伴淋巴结肿大或临床有便血者,应高度警惕恶性肿瘤。
大肠肠壁增厚;腹部计算机断层扫描;肠镜检查
大肠疾病是消化系统常见疾病之一,无论肠道原发疾病还是肠外疾病累及肠道,肠壁增厚都是一种常见而重要的病理改变。计算机断层扫描(CT)用于肠道疾病的诊断已日益普遍,多层螺旋CT快速薄层扫描和强大的图像后处理能力使肠壁增厚是腹部CT比较常见的一种描述。当CT提示肠壁增厚时,是否一定提示有器质性疾病,甚至肿瘤;是否需进一步行肠镜检查以明确诊断一直存有争议[1-2]。本研究通过回顾性分析方法,对136例腹部CT提示大肠肠壁增厚患者的临床资料进行研究。分析患者的主要临床表现、CT所见、病变部位、肠镜检查结果,探讨腹部CT提示大肠肠壁增厚与肠镜检查的关系及其临床意义。
1 资料与方法
1.1 一般资料 分析2008年3月-2014年3月在福建医科大学附属协和医院行腹部CT检查提示大肠肠壁增厚患者共1 206例,而在随后1个月内行肠镜检查且住院资料完整的患者有136例。排除标准:(1)已患有恶性肠道肿瘤;(2)既往有结直肠手术史;(3)CT提示肿块、狭窄及腹腔感染引起的大肠肠壁增厚。
1.2 方法 采用德国Siemens公司SOMATOM Sensation 40CT和美国GE公司Lightspeed QX/I型(16层)螺旋CT机进行上、中腹或全腹部平扫及高压注射泵经内侧肘前浅静脉注射非粒子型造影剂碘海醇注射液(欧苏)75~100 ml(1.5 ml/kg)行增强CT扫描。由从事腹部影像诊断的1名主任医师和1名主治医师共同分析患者的CT图像,阅片时如有不同意见经协商后达成一致。在肠道充盈良好状态下,肠壁厚度>3 mm判定为肠壁增厚[3]。记录以下内容:(1)大肠肠壁增厚的部位;(2)相关CT所见;(3)是否强化及强化的部位。腹部CT提示大肠肠壁增厚并满足上述要求的患者在1个月内行肠镜检查,肠镜检查前要求肠道准备达到满意程度,以避免遗漏小的病灶,发现病灶均取活检,并行病理组织学明确诊断(我院内镜型号CF-Q260AL和CF-240l,奥林巴斯内窥镜,日本)。

2 结果
2.1 基本临床特征 共136例符合标准且资料完整的患者入选,男80例(58.82%),女56例(41.18%),年龄23~86岁,平均年龄(61.87±14.56)岁。患者的主要临床症状中,腹痛64例(47.06%),腹泻22例(16.18%),便血42例(30.88%)。
2.2 病变部位 在136例患者中,腹部CT提示大肠肠壁增厚部位在盲肠者9例(6.62%);升结肠及肝曲者41例(30.15%);横结肠及脾曲者10例(7.35%);降结肠11例(8.09%);乙状结肠者40例(29.41%);直肠者17例(12.50%);弥漫性增厚者8例(5.88%)。
2.3 CT提示大肠肠壁增厚的肠镜检查结果 136例患者中,腹部CT提示大肠肠壁增厚并行肠镜检查提示正常者35例(25.74%),异常者101例(74.26%),其中恶性肿瘤41例(30.15%),肠息肉38例(27.94%),炎症(包括结肠炎和直肠炎)22例(16.18%)。
2.4 肠镜下正常组与异常组临床特点的比较 35例正常的患者中,肠壁增厚多位于右半结肠,与异常组比较差异有统计学意义(P<0.001),而主要临床症状,如腹痛、腹泻、便血两组间比较,差异无统计学意义(P>0.05,见表1)。
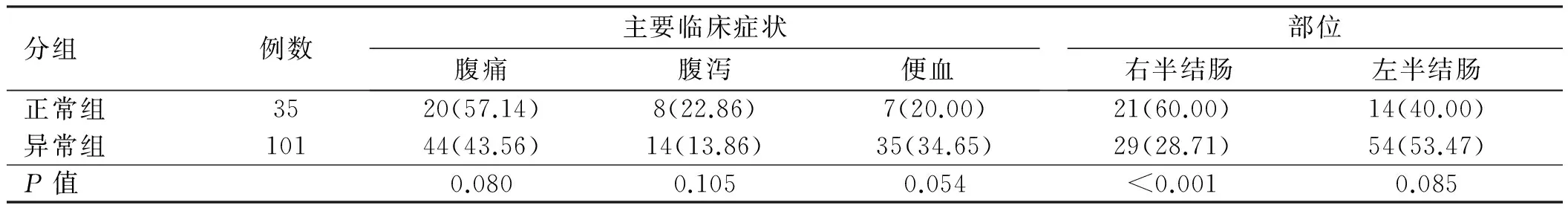
表1 肠镜下正常组与异常组临床特点比较[例数(%)]Tab 1 Comparison of the clinical characteristics between normal group and abnormal group under colonoscopy [n(%)]
2.5 肠道良恶性疾病临床因素及腹部CT所见比较 41例肠道恶性肿瘤患者中,7例(17.07%)无明显肠道症状。与良性疾病(肠息肉、炎症)相比,便血、淋巴结肿大多见于恶性肿瘤(P<0.05)。肠壁增厚位于左半结肠,多见于恶性肿瘤(P=0.006),而肠壁弥漫性增厚均见于良性疾病(P=0.005,见表2)。
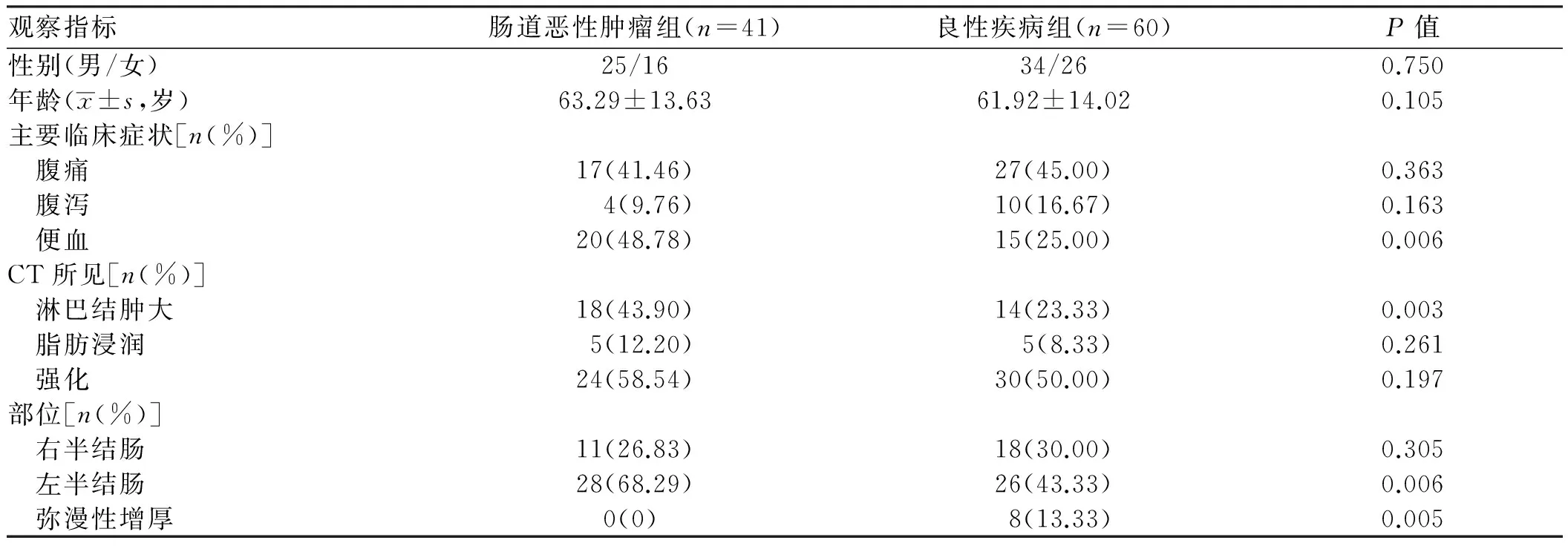
表2 肠道良恶性疾病临床因素及腹部CT所见比较Tab 2 Comparison of clinical variables and features of abdominal CT between the benign and malignant intestinal diseases
2.6 结肠炎症性疾病与非炎症疾病临床因素及腹部CT所见比较 与非炎症性疾病(肠息肉、恶性肿瘤)相比,腹痛在炎症性疾病中所占比例较高,差异有统计学意义(P<0.001)。且CT提示为弥漫性肠壁增厚,均见于炎症性疾病(P<0.001,见表3)。
2.7 CT提示肠壁增厚不同疾病的肠镜所见 CT提示肠壁增厚经肠镜检查可诊断为肠道恶性肿瘤、肠息肉及炎症性肠道疾病,不同疾病在肠镜下表现不同(见图1~4)。

表3 结肠炎症性疾病与非炎症性疾病临床因素及腹部CT所见比较[例数(%)]Tab 3 Comparison of clinical variables and features of abdominal CT between inflammatory diseases and non-inflammatory diseases[n(%)]
3 讨论
大肠肠壁增厚是腹部CT诊断中常见的异常征象,肠道是蠕动的空腔器官,肠壁厚度与其扩张程度密切相关,因此准确测量肠壁的厚度尚有一定的难度;d′Almeida等[4]提出口服清水也会导致肠壁增厚的假象,所以误诊率较高。目前判断肠壁增厚还缺乏统一标准,一般认为,排除肠管充盈不佳或肠壁收缩时导致的假象后,在充盈状态良好下,肠壁厚度超过3 mm即为肠壁增厚,并根据增厚的程度分为轻度(3~6 mm)、中度(6~12 mm)及重度(>12 mm),也有文献认为直肠壁的厚度超过5 mm为直肠壁增厚[3,5-6]。Wolff等[7]将107例CT提示大肠肠壁增厚的患者行肠镜检查发现73.9%的病变率。本研究中,腹部CT提示大肠肠壁增厚并行肠镜检查异常的比例占74.26%。
CT提示大肠肠壁增厚的患者,男性发生率高于女性,且大多数年龄在50岁以上[8]。本研究中,男性占58.82%,女性占41.18%,平均年龄为(61.87±14.56)岁。大肠肠壁增厚其病变部位可分布在各段结肠,其中升结肠和乙状结肠发病最多,目前原因尚不明确。Uzzaman等[9]也报道了CT提示肠壁增厚的165例患者中有48.48%的肠壁增厚患者病变位于乙状结肠和直肠。大肠肠壁增厚也可见于正常人[10],本研究中有35例(25.74%)腹部CT提示肠壁增厚且行肠镜检查为正常者,其中位于右半结肠者21例(60.00%),差异有统计学意义。Uzzaman等[9]报道了42.42%的腹部CT提示肠壁增厚为正常变异。Stermer等[2]也发现腹部CT提示肠壁增厚有31.91%为正常变异,且有63.33%位于右半结肠,其原因尚不清楚,可能与右半结肠的结肠带较明显、肠腔较宽大有关。虽然CT提示肠壁增厚可见于部分正常人,Padda等[11]则认为对于CT提示肠壁增厚且有可疑症状,应行进一步肠镜检查,如肠镜检查结果为正常的患者,应行灌肠检查或重复CT来协助诊断,以免漏诊。
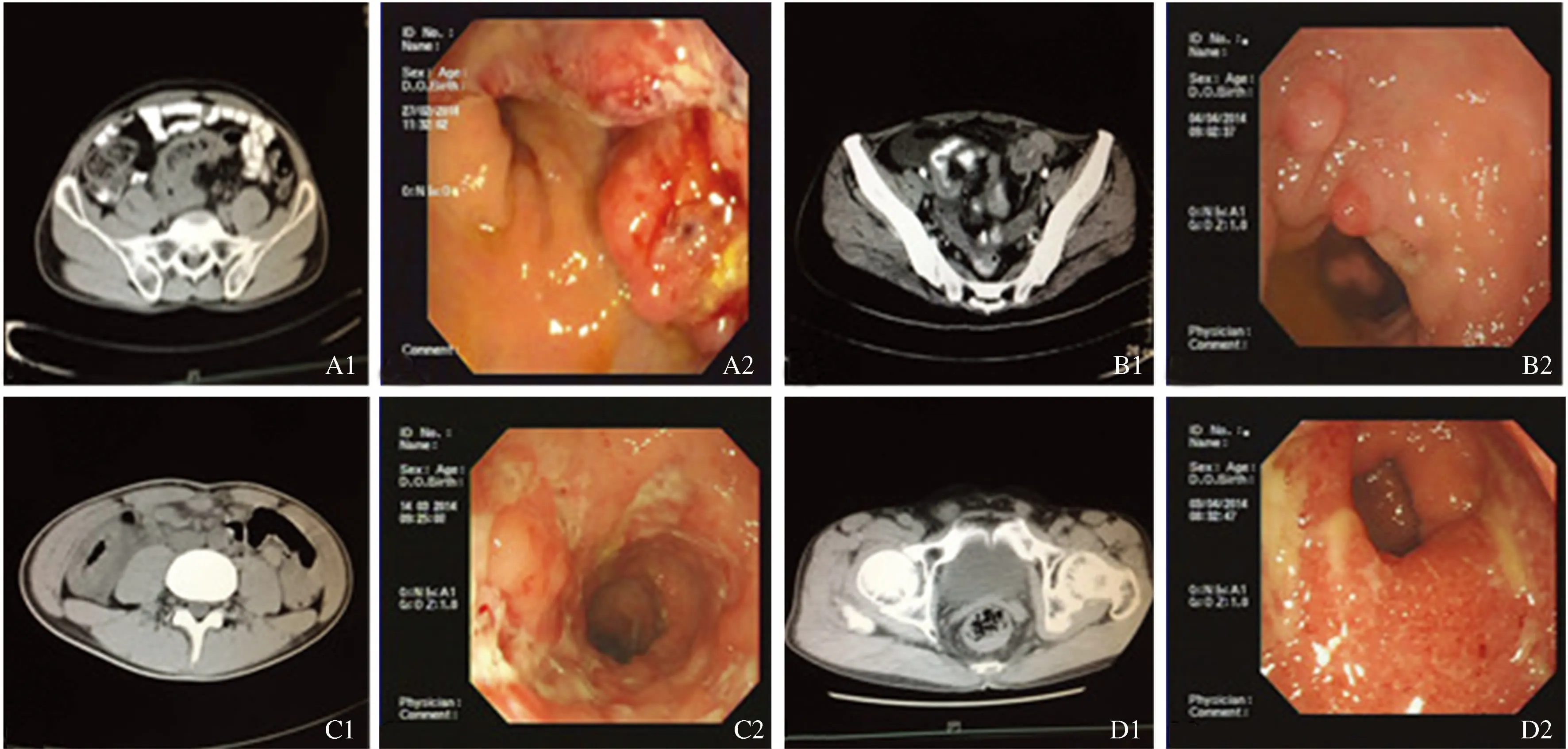
图1 肠镜下不同疾病肠壁增厚 A1:CT提示乙状结肠壁明显增厚,厚约2.1 cm,周围脂肪密度增高、模糊,增强明显强化;A2:肠镜下距肛门口15~18 cm见半环状新生物,表面溃烂,质脆易出血;B1:CT提示乙状结肠壁增厚;B2:肠镜下距肛门口约20 cm可见多个小息肉,表面充血;C1:CT提示升结肠壁增厚;C2:肠镜下盲肠部见散在不规则及环形溃疡,升结肠见节段性溃疡;D1:CT提示直肠壁增厚,增强后可见强化;D2:肠镜下距肛门口约8 cm以下直肠可见广泛充血糜烂及浅溃疡形成
Fig 1 The bowel wall thickening of different diseases under colornoscopy A1: CT images showed sigmoid colon wall was thickening obviously,with a 2.1 cm in diameter,the surrounding fat density was increased and fuzzy with obvious enhancement on contrast material-enhanced CT scan; A2: Colonoscopy showed a hemispherical bulging mass at 15~18 cm from the anus,with mucosal erosion and tendency to bleed easily; B1: CT images showed sigmoid colon wall was thickening; B2: At colonoscopy,mounts of polyps were founded at 20 cm from the anus,with a congestion surface in the wall of the intestine; C1: CT images showed ascending colon wall was thickening; C2: Colonoscopy revealed irregular and annular ulcers in cecum,with segmental ulcers in ascending colon; D1: CT images showed rectum wall was thickening,with enhancement on contrast material-enhanced CT scan; D2: At colonoscopy,a large scope covered by some mucosal erosion and ulcers were noted at 8 cm from the anus,with an erosion surface in the right anterior wall of the esophagus
在我国,大肠癌发病率呈逐年上升的趋势,目前我国大肠癌的死亡率居第5位[12]。本研究中136例CT提示大肠肠壁增厚的患者,有41例是肠道恶性肿瘤,所占比例为30.15%,比国外报道高[13-14]。Shin等[15]发现CT提示肠壁增厚并行肠镜检查为恶性肿瘤者,右半结肠癌占35%,而左半结肠占71%。本研究中,恶性肿瘤病变部位在左半结肠多于右半结肠(P=0.006),与国外报道一致。本研究也发现,相对于其他肠道疾病,便血在腹部CT提示肠壁增厚并行肠镜检查证实为恶性肿瘤的患者中比较常见(P=0.006)。Uzzaman等[9]同样认为便血在诊断是否为肠癌方面具有重要的价值。Lee等[8]报道癌症患者更常伴有淋巴结肿大,建议CT提示肠壁增厚并伴淋巴结肿大的患者行肠镜检查以明确诊断。值得注意的是,本研究中7例(17.07%)肠癌患者在临床上无明显肠道症状,Tellez-Avilla等[16]报道有29%的肠癌患者无临床症状,这意味着CT提示肠壁增厚可以发现潜在的肠道恶性肿瘤。炎症性疾病也是肠道常见疾病之一,如特发性炎症性肠病和感染性结肠炎行腹部CT检查均可见肠壁增厚。本研究中,腹部CT提示大肠肠壁增厚的136例患者中,炎症性疾病有22例(16.18%)。与非炎症性疾病相比,CT提示患者大肠肠壁增厚,且伴有腹痛,则炎症性疾病可能性更大。同时,CT提示为弥漫性肠壁增厚时,均见于炎症性疾病。Lee等[8]也报道腹部CT提示肠壁增厚为弥漫性增厚时,应考虑结肠炎的可能,建议行肠镜检查明确诊断。
对于早期发现肠壁增厚的病变,存在于体液特别是血液中易于检测,同时具有高敏感性和特异性,但目前仍然没有一种理想的方法对肠壁增厚的病变诊断符合上述要求,临床上普遍采取的还是化验相关肿瘤标记物,结合临床资料和影像学检查、内镜技术进行全面分析以提高敏感度和特异度。
[1]Bleibel W,Guerrero JE,Kim S,et al. The clinical significance of incidental computer tomography finding of gastrointestinal luminal wall thickening as evaluated by endoscopy [J]. Dig Dis Sci,2007,52(7): 1709-1712.
[2]Stermer E,Lavy A,Rainis T,et al. Incidental colorectal computed tomography abnormalities: would you send every patient for a colonoscopy [J]. Can J Gastroenterol,2008,22(9): 758-760.
[3]Low VH. Bowel wall thickening on CT [J]. Abdom Imaging,1998,23(1): 107-110.
[4]d'Almeida M,Jose J,Oneto J,et al. Bowel wall thickening in children: CT findings [J]. Radiographics,2008,28(3): 727-746.
[5]Desai RK,Tagliabue JR,Wegryn SA,et al. CT evaluation of wall thickening in the alimentary tract [J]. Radiographics,1991,11(5): 771-783.
[6]Bharucha AE,Tremaine WJ,Johnson CD,et al. Ischemic proctosigmoiditis [J]. Am J Gastroenterol,1996,91(11): 2305-2309.
[7]Wolff JH,Rubin A,Potter JD,et al. Clinical significance of colonoscopic findings associated with colonic thickening on computed tomography: is colonoscopy warranted when thickening is detected? [J]. Clin Gastroenterol,2008,42(5): 472-475.
[8]Lee JS,Cho JH,Kim KO. Clinical significance of the large intestinal wall thickening detected by abdominal computed tomography [J]. Korean J Gastroenterol,2012,60(5): 300-305.
[9]Uzzaman MM,Alam A,Nair MS,et al. Computed tomography findings of bowel wall thickening: its significance and relationship to endoscopic abnormalities [J]. Ann R Coll Surg Engl,2012,94(1): 23-27.
[10]Ainsworth AP,Fristrup CW,Mortensen MB. Diagnostic workup for incidentally found thickening of the stomach wall [J]. Ugeskr Laeger,2013,175(7): 432-435.
[11]Padda M,Vadgama J,Sandhu P,et al. Clinical significance of incidental colorectal wall thickening on computed tomography scan in African-American and Hispanic patients [J]. Dig Dis Sci,2007,52(11): 3159-3164.
[12]Li LD,Lu FZ,Zhang SW,et al. Changing trend and forecast analysis of malignant tumor mortality in the recent 20 years in China [J]. Chin J Oncol,1997,19(1): 3-5. 李连弟,鲁凤珠,张思维,等. 中国恶性肿瘤死亡率20年变化趋势和近期预测分析[J]. 中华肿瘤杂志,1997,19(1): 3-5.
[13]Moraitis D,Singh P,Jayadevan R,et al. Colonic wall thickening on computed tomography scan and clinical correlation. Does it suggest the presence of an underlying neoplasia [J]. Am Surg,2006,72(3): 269-271.
[14]Nicholson BD,Hyland R,Rembacken BJ,et al. Colonoscopy for colonic wall thickening at computed tomography: a worthwhile pursuit? [J]. Surg Endosc,2011,25(8): 2586-2589.
[15]Shin WC,Jeong MJ. Clinical significance of incidentally detected bowel wall thickening on abdominal computerized tomography scan [J]. Korean J Gastroenterol,2005,45(6): 409-416.
[16]Tellez-Avila FI,García-Osogobio S,Chavez-Tapia NC,et al. Utility of endoscopy in patients with incidental gastrointestinal luminal wall thickening detected with CT [J]. Surg Endosc,2009,23(10): 2191-2196.
(责任编辑:陈香宇)
Clinical significance of the large intestinal wall thickening detected by abdominal computed tomography
WU Qunying,LI Jianying
Department of Gastroenterology,Fujian Medical University Union Hospital,Fuzhou 350009,China
Objective To conduct retrospective analysis of abdominal computed tomography (CT) reports,and to investigate the clinical significance of the large intestinal wall thickening on CT. Methods Formal reports for all patients undergoing abdominal CT from Mar. 2008 to Mar. 2014 were included,only those patients with a report of bowel wall thickening (BWT) who had follow-up colonoscopy were included in the analysis.Results BWT of the right colon was significantly more likely to correspond to an endoscopic finding of normal than other sites (P<0.001). 41 cases (30.15%) were malignant lesions and left colon was high incidence area (P=0.006). Rectal bleeding was reported significantly more often in patients with BWT and malignant disease on endoscopy compared with those with benign disease (P<0.05) and also enlargement of lymph nodes (P<0.05). In all of the non-inflammatory lesions,abdominal pain had statistical significance compared with inflammatory diseases (P<0.001). Most of the colitis involved the entire colon (P<0.001).Conclusion The large intestinal wall thickening on CT but normal colonoscopy findings whose lesions main locate in the right colon,malignant tumor most in the left colon,and most of the colitis involved the entire colon. The large intestinal wall thickening on CT with enlargement of lymph nodes,or patients with symptom of rectal bleeding,high possibility of malignant tumor should be considered.
The large intestinal wall thickening; Abdominal computed tomography; Colonoscopy
吴群英,硕士,研究方向:消化系统疾病。E-mail:383152549@qq.com
李建英,主任医师,硕士生导师,研究方向:消化道疾病的诊疗。E-mail:jyli99@hotmail.com
10.3969/j.issn.1006-5709.2016.02.024
R574.6
A
1006-5709(2016)02-0205-04
2014-10-16
