血液灌流联合血液透析对维持性血液透析患者微炎症状态的影响
2016-03-30赵海英
赵海英
(河北北方学院附属第一医院 河北 张家口 075000)
血液灌流联合血液透析对维持性血液透析患者微炎症状态的影响
赵海英
(河北北方学院附属第一医院 河北 张家口 075000)
摘要:目的探讨血液灌流联合血液透析对维持性血液透析(MHD)患者微炎症状态的影响。方法选取26例MHD患者为研究对象,采用随机数字表法分为血液透析组(对照组)和血液灌流联合血液透析组(治疗组),各13例,2组均进行血液透析治疗,透析时间为4.5~5 h/次,每周2~3次;治疗组在上述治疗基础上每2周进行1次血液灌流,灌流时间为2~2.5 h,完毕后再进行血液透析2 h,疗程均为3个月。对比2组治疗前、治疗3个月后C反应蛋白(CRP)、白细胞介素-6(IL-6)、肿瘤坏死因子-α(TNF-α)、血肌酐(SCr)、血尿素氮(BUN)、钙(Ca2+)、磷(P3+)水平。结果治疗3个月后,对照组CRP、IL-6、TNF-α水平较治疗前有所提高,但无统计学意义(P>0.05),治疗组CRP、IL-6、TNF-α水平较治疗前明显降低(P<0.05),与对照组比较,P<0.05;治疗3个月后,2组SCr、BUN、P3+、Ca2+均有所下降(P<0.05),但SCr、BUN比较,P>0.05,P3+、Ca2+治疗组降低程度优于对照组(P<0.05)。结论血液透析联合血液灌流对MHD可起到良好的协同作用,能有效改善患者微炎症状态,维持水电解质平衡,改善残余肾功能,提高生存质量。
关键词:血液灌流;血流透析;维持性血液透析;微炎症状态
慢性肾衰竭为损害全身各器官较严重的疾病,血液透析为有效的肾脏替代疗法,是提高患者生存质量与存活率的关键[1]。血液透析虽可清除尿毒症患者体内小分子毒素和积蓄的水分,纠正水电解质与酸碱平衡紊乱,改善病情,但远期透析相关并发症仍不可避免,预后不理想[2-4]。本研究对MHD患者采用血液灌流联合血液透析进行治疗,探讨对MHD患者微炎症状态的影响。现报道如下。
1资料与方法
1.1一般资料选取我院2014年7月—2015年7月收治的26例MHD患者为研究对象,所有患者病情均稳定,透析时间在3个月以上,无自身免疫性疾病、肝炎等,近2个月未接受过激素、免疫抑制剂等治疗。随机分为血液透析组(对照组)和血液灌流联合血液透析组(治疗组)。对照组13例,男7例,女6例;年龄33~67岁,平均(54.4±13.1)岁;其中原发病慢性肾小球肾炎7例,糖尿病肾病2例,良性小动脉肾硬化2例,高血压肾病2例。治疗组13例,男8例,女5例;年龄32~68岁,平均(55.3±12.5)岁;其中原发病慢性肾小球肾炎6例,糖尿病肾病3例,良性小动脉肾硬化2例,高血压肾病2例。2组一般资料比较,差异无统计学意义(P>0.05),具有可行性。
1.2治疗方法2组均采用AK-95血液透析机进行血液透析治疗,透析液为碳酸氢盐,膜面积1.3 m2,超滤系数为5.5 mL/(h·mmHg),透析液流量500 mL/min,血液流量200~250 mL/min,透析时间为4.5~5 h/次,每周2~3次。治疗组在上述治疗基础上采用HA130树脂灌流器每2周进行1次血液灌流,10 mg肝素加500 mL生理盐水配制成肝素生理盐水,首次使用肝素剂量为0.6~0.8 mg/kg,以后逐渐增加到10 mg/h,血流量为150~200 mL/min,灌流时间为2~2.5 h,完毕后再进行血液透析2 h。疗程均为3个月。
1.3观察指标于治疗前、治疗3个月清晨空腹采取2组患者肘静脉血,采用免疫比浊法检查CRP,采用ELISA法检测IL-6、TNF-α水平;采用全自动生化分析仪检测SCr、BUN、Ca2+、P3+;试剂盒均由宁波美康生物科技有限公司生产,严格按照试剂盒说明进行操作。
2结果
2.12组治疗前后微炎症指标比较见表1。
2.2 2组治疗前后血液毒素指标比较见表2。

±s,n=13)
注:与对照组比较,#P<0.05
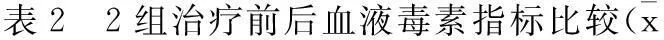
±s,n=13)
注:与治疗前比较,#P<0.05;与对照组比较,ΔP<0.053小结
本研究显示,治疗3个月后,对照组CRP、IL-6、TNF-α水平较治疗前有所提高(P>0.05),治疗组CRP、IL-6、TNF-α水平较治疗前明显降低(P<0.05),与对照组比较P<0.05;治疗3个月后,2组SCr、BUN、P3+、Ca2+均有所下降(P<0.05),SCr、BUN比较2组无统计学意义,P3+、Ca2+治疗组降低程度优于对照组(P<0.05)。说明血液透析联合血液灌流对MHD可起到良好的协同作用,能有效改善患者微炎症状态,维持水电解质平衡,改善残余肾功能,改善临床症状,提高患者生存质量[5-14]。
参考文献:
[1]王磊,王珏,付强,等.慢性肾功能衰竭的治疗现状及研究前景[J].现代生物医学进展,2012,12(10):1983-1985.
[2]朱征西,陆绍强,梁碧琴,等.不同的血液净化方式对维持性血液透析患者微炎症状态的影响[J].中国血液净化,2011,10(1):18-21,28.
[3]唐毓启.不同透析方式对维持性血液透析患者微炎症状态的影响[J].现代仪器与医疗,2014,20(5):55-57.
[4]陈建辉,廖永强,周军,等.IL-1、IL-6、TNF-α、CRP联合检测在维持性血液透析患者微炎症治疗中的临床应用[J].国际检验医学杂志,2012,33(24):2986-2987.
[5]MEUWESE C L,STENVINKEL P,DEKKER F W,et al.Monitoring of inflammation in patients on dialysis:forewarned is forearmed[J].Nature Reviews Nephrology,2011,7(3):166-176.
[6]耿明亮,周登河,段海玲,等.血液透析联合血液灌流对维持性血液透析患者微炎症状态的影响[J].中国医药指南,2015,13(1):197-198.
[7]王凌,陈洁.血液透析与血液灌流联合治疗对维持性血液透析患者微炎症状态的影响[J].健康研究,2014,34(4):400-401,404.
[8]毕光宇,刘昌华,徐军,等.血液灌流联合复方α酮酸对维持性血液透析患者微炎症及营养状况的影响[J].江苏医药,2012,38(24):2967-2969.
[9]COACCIOLI S,STANDOLI M L,BIONDI R,et al.Assessment of the oxidative stress markers in patients with chronic renal insufficiency undergoing dialysis treatment[J].La Clinica Terapeutica,2010,161(5):441-444.
[10]金领微.血液透析与血液灌流联合治疗对维持性血液透析患者微炎症状态的影响[J].南方医科大学,2010(7):7-71.
[11]谭新忠.尿毒症患者血液透析后血清CRP和IL-6水平变化及其临床意义[J].中国当代医药,2012,19(1):75-76.
[12]刘妍,成建钊,郭自炎.血液灌流联合血液透析治疗尿毒症疗效及对患者肾功能的影响[J].中国医药导刊,2014,16(2):225-226.
[13]商国君,苗雪英,郑秀清,等.中药灌肠配合高通量血液透析对尿毒症患者血清脂联素、TNF-α的影响[J].临床合理用药杂志,2014,7(28):26-27.
[14]王雅,章茵,唐进攀.血液透析联合血液灌流对尿毒症透析患者Hcy、hs-CRP、IL-6、TNF-α水平的影响[J].海南医学,2014,25(16):2401-2403.
Blood perfusion in combined with hemodialysis on the micro-inflammation state in patients with maintenance hemodialysis
ZHAO Haiying
(The First Hospital Affiliated to Hebei North University,Zhangjiakou 075000,Hebei Province,China)
Abstract:ObjectiveTo explore the effect of blood perfusion in combined with hemodialysis on the micro-inflammation state in patients with maintenance hemodialysis (MHD).MethodsA total of 26 patients with MHD who were admitted in our hospital from July,2014 to July,2015 were included in the study and randomized into the observation group (blood perfusion in combined with hemodialysis group) and the control group (hemodialysis group).The patients in the two groups were given hemodialysis,4.5~5 h/time,2~3 times each week.On this basis,the patients in the observation group were given blood perfusion,2~2.5 h/time,once every two week,and given another hemodialysis for 2 h after blood perfusion.A3 month treatment was regarded as one course.The levels of CRP,IL-6,TNF-α,SCr,BUN,Ca2+,and P3+before treatment and 3 months after treatment in the two groups were observed and compared.ResultsAfter 3-month treatment,the levels of CRP,IL-6,and TNF-α in the control group were elevated when compared with before treatment,but the difference was not statistically significant (P>0.05);the levels of CRP,IL-6,and TNF-α in the observation group were significantly reduced when compared with before treatment (P<0.05),and the difference was statistically significant when compared with the control group (P<0.05).After 3-month treatment,the levels of SCr,BUN,Ca2+,and P3+in the two groups were significantly reduced (P<0.05),but the comparison of SCr,and BUN was not statistically significant (P>0.05).The decreased degree of Ca2+,and P3+levels in the observation group was significantly superior to that in the control group (P<0.05).ConclusionBlood perfusion in combined with hemodialysis in the treatment of MHD can produce a favorable synergistic effect,effectively improve the micro-inflammation state,maintain the water-electrolyte balance,improve the residual renal function and clinical symptoms,and enhance the patients’ living qualities.
Keywords:blood perfusion;hemodialysis;maintenance hemodialysis;micro inflammation state
(收稿日期:2015-10-22)
文章编号:2095-6258(2016)01-0168-03
中图分类号:R459.6
文献标志码:A
作者简介:赵海英(1983-),女,大学本科,主管护师,主要从事血液透析护理研究。
基金项目:河北省科技研究与发展指导项目(1021057D)。
DOI:10.13463/j.cnki.cczyy.2016.01.059
