甲状腺微小乳头状癌颈淋巴结转移的危险因素分析
2015-12-20卞雪艳孙姗姗郭文宇赵明慧孔令平张仑
卞雪艳 孙姗姗 郭文宇 赵明慧 孔令平 张仑
·临床研究与应用·
甲状腺微小乳头状癌颈淋巴结转移的危险因素分析
卞雪艳 孙姗姗 郭文宇 赵明慧 孔令平 张仑
目的:探讨甲状腺微小乳头状癌颈淋巴结转移的危险因素,分析高分辨率B超对侧颈淋巴结转移的诊断意义。方法:回顾性分析2013年1月至2013年11月天津医科大学肿瘤医院共1 037例甲状腺微小乳头状癌患者的临床病理资料。结果:1 037例患者中央区淋巴结转移率为32.02%(332例),侧颈淋巴结转移率为6.85%(71例)。男性、年龄≤45岁、肿瘤直径>5 mm、多灶性、双发性、侵犯包膜和甲状腺外局部侵犯者中央区淋巴结转移率较高(P<0.05)。男性、中央区淋巴结转移、B超诊断阳性者侧颈淋巴结转移率较高,并且随着中央区淋巴结转移数目的增多,侧颈转移率也随之增高(P<0.05)。高分辨率B超对侧颈淋巴结转移的灵敏度、特异度分别为92.96%、81.48%。结论:对中央区淋巴结转移高危因素的人群应行预防性中央区淋巴结清扫术,高分辨率B超对预测甲状腺微小乳头状癌患者颈淋巴结转移具有重要的诊断意义,对侧颈淋巴结转移高危因素的人群应行患侧侧颈淋巴结清扫术。
甲状腺微小乳头状癌 颈淋巴结清扫术 B超 诊断
近几十年甲状腺乳头状癌的发病率逐年增高,占所有新发甲状腺恶性肿瘤90%以上[1]。其可能原因是随着影像学技术如B超、CT、MRI及细针穿刺学的发展,甲状腺乳头状癌的检出率递增。甲状腺微小乳头状癌(papillary thyroid microcarcinoma,PTMC)是指肿瘤直径≤1 cm的甲状腺乳头状癌[2]。据报道,甲状腺微小乳头状癌的中央区淋巴结转移率可达24%~64%[3-4]。目前对于cN0的PMTC患者是否需行中央区淋巴结清扫术观点不一,有研究认为预防性清扫中央区淋巴结增加了喉返神经损伤及甲状旁腺功能低下的危险[5],但另有研究认为预防性中央区淋巴结清扫可降低PMTC患者复发率并提高生存率[6-7]。本研究拟分析甲状腺微小乳头状癌淋巴结转移的相关危险因素,筛选淋巴结转移高危险因素患者,从而为手术方式的选择提供参考价值并探讨高分辨率B超对诊断侧颈淋巴结转移的意义。
1 材料与方法
1.1 临床资料
天津医科大学肿瘤医院2013年1月至2013年11月PMTC患者共1 221例,其中新发病例1 120例(91.73%)。单纯行患侧腺叶切除83例,行中央区淋巴结清扫术或甲状腺癌联合根治术1 037例。纳入标准:初治,经术后病理确诊为PMTC,手术方式为腺叶+中央区淋巴结清扫术或侧颈淋巴结清扫术。中央区淋巴结清扫术的范围上界至甲状软骨,下界达胸腺,外侧界为颈动脉鞘内侧缘,包括气管前、气管旁、喉前淋巴结等。侧颈淋巴结清扫范围根据1991年美国耳鼻喉头颈外科基金会标准分为Ⅱ、Ⅲ、Ⅳ、Ⅴ区。术中在有效保留甲状旁腺及喉返神经功能的情况下行病灶同侧中央区淋巴结清扫术。若术前B超或术中探查发现有侧颈淋巴结转移,则术中清除病灶侧颈淋巴结。
1.2 统计学分析
实验数据分析采用SPSS 20.0统计软件,结果采用χ2检验,多因素分析采用非条件Logistic回归模型分析。P<0.05为差异有统计学意义。
2 结果
2.1 患者特点
1037例行中央区淋巴结清扫或侧颈淋巴结清扫术的甲状腺微小乳头状癌患者中,男性208例(20.1%)、女性829例(79.9%),男女比例1∶3.99;年龄12~76岁,平均年龄(45.67±0.99)岁,其中年龄≤45岁505例(48.7%),>45岁532例(51.3%)。肿瘤直径≤5mm 499例(48.1%),>5 mm 538例(51.9%)。1 037例患者中,多灶性、双发性、包膜侵犯、局部侵犯、伴发桥本甲状腺炎患者所占比例分别为32.5%(337例)、34.5%(358例)、68.9%(715例)、2.6%(27例)、6.3%(65例)。所有病例中,中央区淋巴结转移率为32.02%(332例),侧颈淋巴结转移率为6.85%(71例),同时发生中央区和侧颈淋巴结转移率为6.65%(69例)。其中经术前B超诊断或术中探查有侧颈区淋巴结转移者98例,均行患侧甲状腺癌联合根治术。
2.2 中央区转移危险因素
如表1所示,男性患者的中央区淋巴结转移率高于女性患者(P<0.05)。年龄≤45岁患者中央区淋巴结转移率为35.05%,年龄>45岁患者其中央区淋巴结转移率为29.16%(P=0.041),说明年龄与中央区淋巴结转移有相关性,且年龄≤45岁患病是其危险因素。肿瘤直径是否影响中央区淋巴结转移(central lymph node metastasis,CLNM)一直存在争议,本研究1 037例患者中,肿瘤直径≤5 mm 126例(25.25%),>5 mm 206例(48.33%),说明病灶大小是CLNM的影响因素(P<0.05)。同样,肿瘤侵犯包膜、侵犯局部组织、多灶性及双发性均为CLNM的危险因素(P<0.05),而伴发桥本甲状腺炎对CLNM无影响(P=0.824)。多因素分析表明,年龄、性别、肿瘤大小、侵犯包膜是甲状腺微小乳头状癌的独立危险因素(表2)。
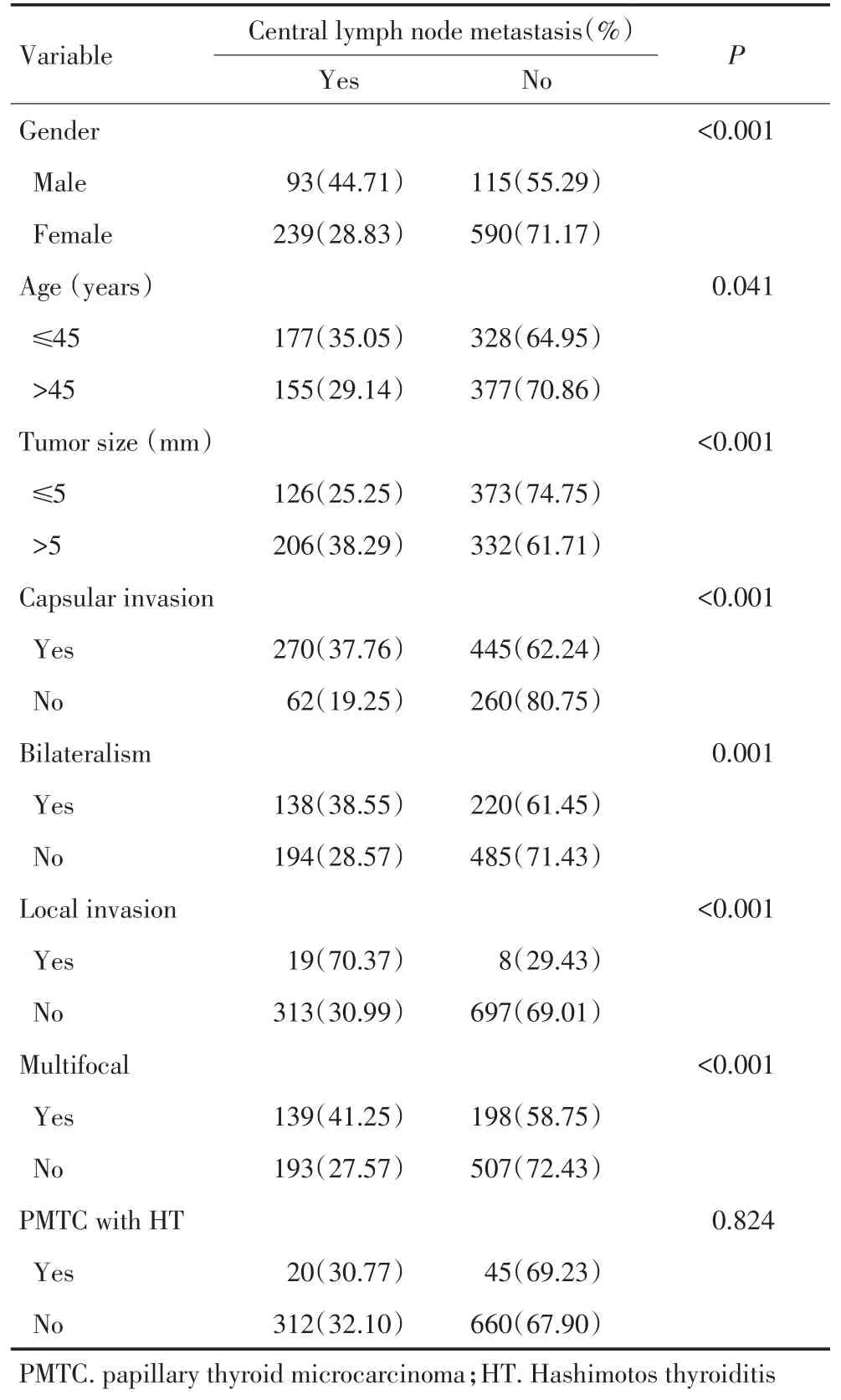
表1 中央区淋巴结转移情况与临床资料相关性分析Table 1 Correlation analysis of cervical lymph node metastases with clin⁃ical data of papillary thyroid microcarcinoma patients
2.3 侧颈淋巴结转移的危险因素
本研究分析98例行甲状腺癌联合根治术的PMTC患者,其中经术后病理确诊的侧颈淋巴结转移患者71例,转移率72.45%。单因素分析提示(表3),男性、中央区转移、术前B超诊断阳性、中央区淋巴结转移数目为侧颈转移的危险因素,且随着中央区转移淋巴结数目增多,侧颈转移的概率亦增加(P<0.05)。多因素分析表明,B超诊断是侧颈转移的独立预测因素(P=0.003),OR值为0.227,95%CI为15.358~219.644。
2.4 B超对侧颈淋巴结转移诊断的意义
98例行侧颈淋巴结清扫术的患者中经B超诊断有侧颈淋巴结转移为86例,病理确诊为71例。B超诊断有侧颈淋巴结转移而病理诊断阴性5例,而病理诊断阳性B超诊断阴性5例。高分辨率B超对侧颈淋巴结转移的灵敏度、特异度、假阴性率和假阳性率分别为92.96%、81.48%、7.04%、18.52%。

表2 中央区淋巴结转移的多因素Logistic回归分析Table 2 Multivariate logistic regression analysis for central lymph node metastasis

表3 侧颈淋巴结转移情况与临床资料相关性分析Table 3 Correlation analysis of lateral neck metastases with clinical data of papillary thyroid microcarcinoma patients

表3 侧颈淋巴结转移情况与临床资料相关性分析(续表3)Table 3 Correlation analysis of lateral neck metastases with clinical data of papillary thyroid microcarcinoma patients
3 讨论
淋巴结转移是分化型甲状腺癌最主要的转移途径,转移方式主要是由中央区淋巴结转移至侧颈区淋巴结。有研究提示PMTC颈部淋巴结转移率为24%~64%[3-4],而本研究中央区淋巴结转移率为32.02%,与文献报道一致。尽管甲状腺微小乳头状癌的颈部淋巴结转移率较高,但有报道提示颈部淋巴结转移对分化型甲状腺癌患者的死亡率无影响[8]。因此对临床上淋巴结阴性的PMTC患者是否需要预防性清扫中央区淋巴结至今仍有争议[9]。
Mao等[1]对332例甲状腺微小癌患者进行分析,认为年龄(≤45岁)、男性是甲状腺微小乳头状癌中央区转移的独立危险因素。本研究对1 037例甲状腺微小乳头状癌进行回顾性分析发现,年龄≤45岁、男性、肿瘤直径>5 mm、侵犯包膜是PMTC患者中央区转移的独立危险因素。Liu等[10]一项Meta分析统计1 928例行预防性中央区淋巴结清扫的PMTC患者,认为对于肿瘤直径>5 mm、多灶性或侵犯包膜的PMTC患者应行预防性中央区淋巴结清扫术。Popa⁃dich等[11]认为,中央区淋巴结清扫可造成暂时性的低钙及声带麻痹,但对于远期低钙症状及声带麻痹两组间比较则无统计学意义。国内有报道称二次手术喉返神经损伤率高达17%[12]。吴延升等[13]对cN0期患者行预防性淋巴结清扫术后复发率明显低于单纯肿物切除和局部广切者。因此本研究认为对于中央区转移高危因素的人群(年龄≤45岁、男性、肿瘤直径>5 mm、侵犯包膜)应预防性行患侧中央区淋巴结清扫,可以避免复发再手术时因气管食管沟瘢痕粘连或组织解剖不清造成甲状旁腺和喉返神经的损伤。
目前关于Ⅵ区淋巴结转移能否作为预测侧颈淋巴结转移的指标众说纷纭。本研究分析了98例行侧颈淋巴结清扫术的PMTC患者,其侧颈转移率为72.45%,明显高于中央区淋巴结转移率,可能是因术前B超为术式的选择提供了诊断意义。本组分析显示高分辨率B超对诊断侧颈淋巴结转移的灵敏度达92.96%,男性及中央区淋巴结转移均为侧颈淋巴结转移的危险因素,而且随着中央区淋巴结转移数目增多,侧颈淋巴结转移率增加。有研究表明当中央区淋巴结转移数目超过3枚时,甲状腺乳头状癌患者的10年无复发生存率较高[14]。本研究建议对于男性、术前B超诊断有侧颈转移或术中发现中央区转移淋巴结数目超过3枚的患者,应行预防性侧颈淋巴结清扫术。
Mizrachi等[15]发现,术前B超对中央区淋巴结转移诊断的灵敏度和特异度分别为95%和90%。Hwang等[16]发现,术前B超对侧颈淋巴结转移诊断的灵敏度和特异度分别为93.8%和80.0%。本研究应用术前超声评估,发现高分辨率B超对侧颈淋巴结转移的灵敏度、特异度、假阴性率和假阳性率分别为92.96%、81.48%、7.04%、18.52%,具有较高的诊断符合率,而且B超具有方便廉价、无放射性的优点。Hong等[17]也曾报道B超对甲状腺微小乳头状癌侧颈淋巴结转移的诊断意义。因此,本研究推荐B超作为甲状腺癌颈淋巴结转移诊断的重要评估手段。
本研究数据为回顾性分析,尚需前瞻性研究证实。但据Carling等[18]研究提示,鉴于甲状腺乳头状癌生存率较高,一项前瞻性临床试验可能需5 840例患者,花费近0.15亿美元,完成此项目耗资巨大,所以对中央区淋巴结清扫的问题至今仍是争议不断。
[1] Mao LN,Wang P,Li ZY,et al.Risk factor analysis for central nodal metastasis in papillary thyroid carcinoma[J].Oncology Let⁃ters,2015,9(1):103-107.
[2] Xu D,Lv X,Wang S,et al.Risk factors for predicting central lymph node metastasis in papillary thyroid microcarcinoma[J].Int J Clin Exp Pathol,2014,7(9):6199-6205.
[3] Cho SY,Lee TH,Ku YH,et al.Central lymph node metastasis in papillary microcarcinoma can be stratified according to the number,the size of metastatic foci,and the presence of desmopla⁃sia[J].Surgery,2014,157(1):111-118.
[4] Zhao Q,Ming J,Liu C,et al.Multifocality and total tumor diame⁃ter predict central neck lymph node metastases in papillary thy⁃roid microcarcinoma[J].Ann Surg Oncol,2013,20(3):746-752.
[5] Giugliano G,Proh M,Gibelli B,et al.Central neck dissection in differentiated thyroid cancer:technical notes[J].Acta Otorhinolar⁃yngol Ital,2014,34(1):9-14.
[6] Wang Wt,Gu J,Shang J,et al.Correlation analysis on central lymph node metastasis in 276 patients with cN0 papillary thyroid carcinoma[J].Int J Clin Exp Pathol,2013,6(3):510-515.
[7] Kim MK,Mandel SH,Baloch Z,et al.Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer [J].Arch Otolaryngol Head Neck Surg,2004,130(10):1214-1216.
[8] Mazzaferri EL,Jhiang SM.Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer[J]. Am J Med,1994,97(5):418-428.
[9] Lee J,Song Y,Soh EY.Central Lymph Node Metastasis Is an Im⁃portant Prognostic Factor in Patients with Papillary Thyroid Mi⁃crocarcinoma[J].Journal of Korean Medical Science,2014,29(1): 48-52.
[10]Liu Z,Wang L,Yi P,et al.Risk factors for central lymph node metastasis of patients with papillary thyroid microcarcinoma:a meta-analysis[J].International Journal of Clinical and Experimen⁃tal Pathology,2014,7(3):932-937.
[11]Popadich A,Levin O,Smooke-Praw S,et al.A Multicenter co⁃hort study of total thyroidectomy and routine central lymph node dissection for cN0 papillary thyroid cancer[J].Surgery, 2011,150(6):1048-1057.
[12]Liao YX,Tang HH,Tan XG,et al.Clinical analysis of 73 cases of differentiated thyroid carcinoma reoperation[J].Chinese Jour⁃nal of General Surgery,2006,15(4):310-311.[廖有祥,汤恢焕,谭兴国,等.分化型甲状腺癌73例再手术的临床分析[J].中国普通外科杂志,2006,15(4):310-311.]
[13]Wu YS,Zhang L,Wang XD,et al.Multivariate regression analy⁃sis of papillary thyroid carcinoma prognosis[J].Chin J Clin On⁃col,2007,34(22):1294-1297.[吴延升,张 仑,王旭东,等.甲状腺乳头状癌预后多因素分析[J].中国肿瘤临床,2007,34(22):1294-1297.]
[14]Ricarte-Filho J,Ganly I,Rivera M,et al.Papillary thyroid carci⁃nomas with cervical lymph node metastases can be stratified into clinically relevant prognostic categories using oncogenic BRAF, the number of nodal metastases,and extra-nodal extension[J]. Thyroid,2012,22(6):575-584.
[15]Mizrachi A,Feinmesser R,Bachar G,et al.Value of ultrasound in detecting central compartment lymph node metastases in differen⁃tiated thyroid carcinoma[J].Eur Arch Otorhinolaryngol,2014,271 (5):1215-1218.
[16]Hwang HS,Orloff LA.Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer[J].Laryngoscope,2011,121(3):487-491.
[17]Hong YR,Yan CX,Mo GQ,et al.Conventional US,elastogra⁃phy,and contrast enhanced US features of papillary thyroid mi⁃crocarcinoma predict central compartment lymph node metastases [J].Scientific Reports,2015,13(5):7748-7755.
[18]Carling T,Carty SE,Ciarleglio MM,et al.American Thyroid As⁃sociation design and feasibility of a prospective randomized con⁃trolled trial of prophylactic central lymph node dissection for pap⁃illary thyroid carcinoma[J].Thyroid,2012,22(3):237-244.
(2015-02-16收稿)
(2015-03-17修回)
(编辑:邢颖)
Risk factor analysis for cervical nodal metastasis in papillary microcarcinoma
Xueyan BIAN,Shanshan SUN,Wenyu GUO,Minghui ZHAO,Lingping KONG,Lun ZHANG
Tianjin Medical University Cancer Institute and Hospital,Department of Maxillofacial&E.N.T Oncology,National Clinical Research Center of Cancer;Key Laboratory of Cancer Prevention and Therapy of Tianjin,Tianjin 300060 China.
Lun ZHANG;E-mail:zhanglun@tjmuch.com
Objective:To investigate the risk factors of central lymph node metastasis(CLNM)and lateral neck lymph node metastasis in papillary thyroid microcarcinoma(PTMC)patients,and to analyze the importance of high resolution ultrasonography in the diagnosis of lateral neck lymph node metastasis in PTMC patients.Methods:A retrospective protocol was applied,and a total of 1 037 PTMC patients were reviewed.These patients underwent central lymph node dissection or thyroidectomy with lateral neck lymph node dissection between January and November in 2013 in the Tianjin Medical University Cancer Institute and Hospital.Clinicopathological factors,namely,age,sex,primary tumor size,multifocality,bilateralism,thyroid capsular invasion,and local invasion,were analyzed. Results:CLNMs were found in 332 of 1037 patients(32.0%),and 71 out of 1037 patients had lateral neck lymph node metastasis (6.85%).In the univariate analysis,patients with the following risk factors were at high risk of CLNM(P<0.05):male,aged≤45 years old,with primary tumor size of>5 mm,multifocality,bilateralism,thyroid capsular invasion,and local invasion.Male patients with central lymph node metastasis positively showed high lateral neck lymph node metastasis rate(P<0.05)according to high-resolution ultrasonography diagnosis.The rate of lateral neck lymph node metastasis increased with increasing number of central lymph node metastases.The sensitivity and specificity of high resolution ultrasonography for lateral neck lymph node metastasis were 92.96%and 81.48% in PTMC patients.Conclusion:Prophylactic central compartment lymph node dissection needs to be performed in patients with CLNM risk factors(i.e.,male,aged≤45 years old,primary tumor size of>5 mm,multifocality,bilateralism,thyroid capsular invasion,and local invasion).The importance of high-resolution ultrasonography in diagnosing lateral neck lymph node metastasis was revealed by the results.Thus,this method should be widely popularized.Radical neck dissection should be performed in male patients who received a positive diagnosis via ultrasonography or those with PTMC who had more than three positive nodes in the central lymph node metastasis.However,given the high occurrence rate of PTMC,a prospective study needs to be conducted in the future.
papillary thyroid microcarcinoma,central compartment lymph node dissection,ultrasonography,diagnosis

10.3969/j.issn.1000-8179.20150156
天津医科大学肿瘤医院颌面耳鼻喉肿瘤科,国家肿瘤临床医学研究中心,天津市肿瘤防治重点实验室(天津市300060)
张仑 zhanglun@tjmuch.com
卞雪艳 专业方向为头颈部肿瘤的诊疗研究。
E-mail:xueyanttkl@sina.cn
